Hacer una valoración del tratamiento quirúrgico de los meningiomas parasellares.
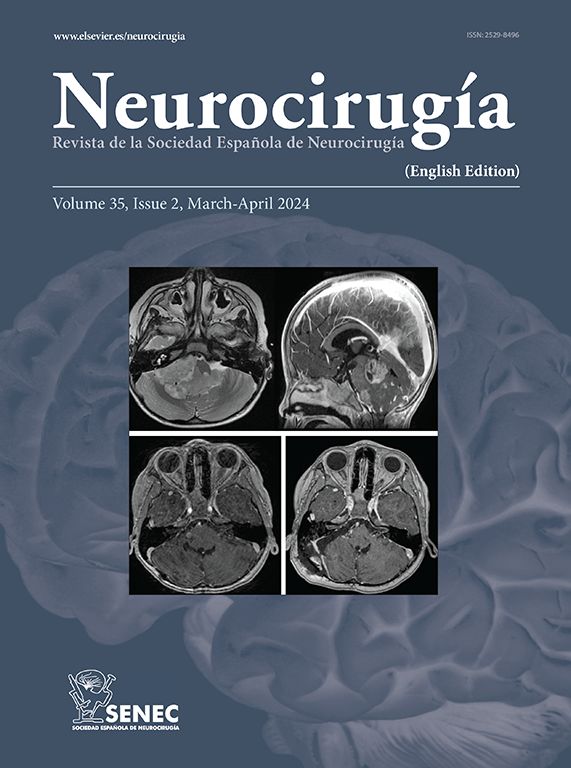
Material y métodosEn los últimos 12 años han sido revisadas de forma retrospectiva las historias clínicas e iconografía de 33 pacientes diagnosticados de meningioma que asentaban en la región parasellar. Bajo esta denominación se ha considerado un área que rodea la silla turca y que está constituida por estructuras situadas profundamente, por lo tanto de difícil acceso, y cuya lesión tiene un alto grado de morbi-mortalidad.
ResultadosSe ha conseguido una extirpación macroscópica completa en el 84.84%, con aparición de recidiva en tres pacientes suponiendo un 9.1%, durante un seguimiento medio de 39.75 meses. El porcentaje preoperatorio de afectación de pares craneales se redujo en un 15.6%. La mortalidad postquirúrgica es de un 9.1%, con una mortalidad global durante todo el seguimiento del 21.21%, siendo la causa más importante de morbi-mortalidad el tromboembolismo pulmonar. Como complicaciones neurológicas en el postoperatorio aparecieron tres hemiparesias y 15 nuevos pares craneales en nueve pacientes en su mayoría de carácter reversible. El 60.60% de los casos (20 pacientes) no presentaron ningún tipo de complicación ni neurológica ni general. Al final del seguimiento el 75% de los enfermos presentaron un Karnofski entre 90 y 100 pudiendo realizar sus actividades preoperatorias con normalidad.
ConclusionesLa cirugía de estos tumores a pesar de su volumen, generalmente importante, y la afectación de estructuras como los pares craneales y vasos del polígono de Willis, puede presentar unos resultados aceptables de morbi-mortalidad. Si se consigue una extirpación completa macroscópica del tumor, las posibilidades de recidiva son bajas, ensombreciéndose el pronóstico del paciente de forma importante si no se consigue una exéresis completa o aparece una recidiva. Finalmente se valora el papel de la radiocirugía y la radioterapia convencional como tratamiento complementario de estos tumores.
To evaluate the surgical treatment of parasellar meningiomas.
Material and methodsA retrospective study of the clinical histories and imaging studies of 33 patients diagnosed of meningiomas located in the parasellar region who were admitted to our Unit over the last 12 years has been performed. Under this name, we considered an area surrounding the sella turca including deeply located structures. These lesions are difficult to approach and carry a high degree of morbidity and mortality.
ResultsComplete macroscopic tumour removal was achieved in 84.4% of the cases, three tumors relapsing (9.1%) over a mean follow-up period of 39.7 months. The preoperative percentage of affectation of cranial nerves was reduced by 15.6%. Post-surgery mortality was 9.1% with an overall mortality along the follow-up period of 21.21%. The most important cause of morbidity-mortality was pulmonary thromboemboIism. Neurological complications during the postoperative period included three cases with hemiparesis and 15 adquired cranial nerve deficits in nine patients, most of which were transient. A 60% of the cases (20 patients) did not have complications, either neurologicalor general. At the end of the follow-up, 75% of the patients had a Karnofski index between 90 and 100.
ConclusionsDespite their volume, which is usually important, and the involvement of structures such as the cranial nerves and vessels of the circle of Willis, surgical treatment of this type of tumor offers acceptable results in terms of morbidity and mortality. If complete macroscopic removal of the tumor can be achived, the possibilities of relapse are low, although the prognosis is considerably worsened if the removal is not complete or if the tumor relapses. Finally, the roles of radiosurgery and conventional radiation therapy as complementary treatment for this type of tumor are discussed.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.