C-0240 - CHRONIC ENCAPSULATED EXPANDING HEMATOMA AFTER STEROTACTIC RADIOSURGERY FOR CEREBRAL ARTERIOVENOUS MALFORMATION
Servicio de Neurocirugía, Complejo Hospitalario Universitario de Albacete, Albacete, Spain. Servicio de Radiología, Complejo Hospitalario Universitario de Albacete, Albacete, Spain. Servicio de Anatomía Patológica, Complejo Hospitalario Universitario de Albacete, Albacete, Spain.
Objectives: Chronic encapsulated intracerebral hematoma (CEIH) is a rare and uncommon late stage of intracerebral hemorrhage with progressive and slow growth. This entity usually presents with a gradual onset of neurological symptoms and nonspecific radiological features, so it is often misdiagnosed as a space-occupying lesion. The pathophysiology is unclear, but focal activation of the VEGF pathway by small clot-sized hemorrhages in a hypoxic state may lead to the formation of granulation tissue with neovascularization.
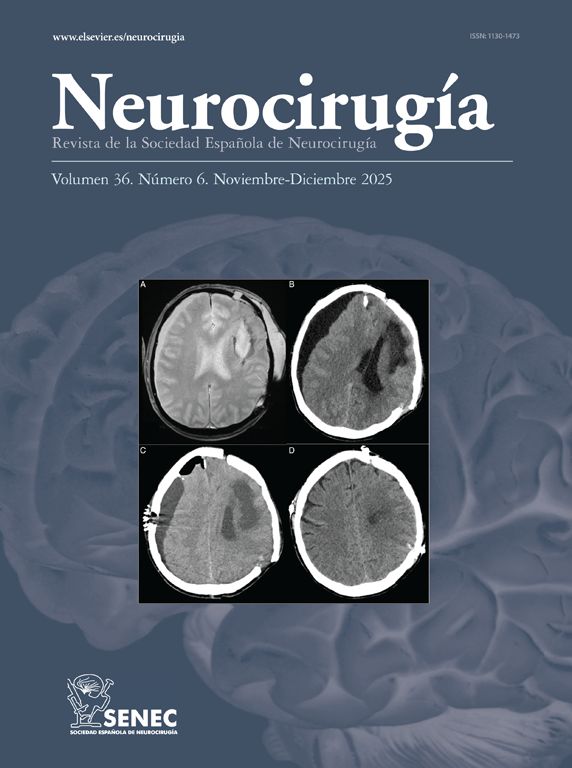
Methods: A 52-year-old man was referred to our hospital with a history of occipital deep AVM, which was treated with two embolization attempts and SRS with a dose of 22 Gy. Cerebral angiography at 18-month follow-up confirmed complete obliteration. Five years later, the patient suffered from slowly progressive occipital headache, bilateral tinnitus, and visual disturbances. Physical examination revealed disorientation and right-sided homonymous hemianopsia. T1-weighted MRI image showed central high-intensity and peripheral isointense signals heterogeneously enhanced after gadolinium. T2-weighted image showed a polilobular lesion with mixed intensities separated by a low-intensity rim. MR Perfusion showed decreased blood flow in the contents of the lesion. F-FDG PET/ CT showed increased uptake in the mass.
Results: Left occipital craniotomy revealed a lesion with a thick fibrous capsule containing a brownish-fluid hematoma. Small vessels were noted in the deepest zone in the periphery of the residual nidus of the AVM. Histological examination confirmed the diagnosis of CEIH. The capsule consisted of organized collagenous tissue and fibrobastic granulation with rich neovascularity without epithelial lining. The patient made a full neurological recovery with a persistent right-sided homonymous visual field deficit.
Conclusions: Regardless of the benign condition of CEIH, its confounding radiological and clinical features often slow down diagnosis and treatment, which is associated with high morbidity due to rebleeding and brain edema. Therefore, radical excision is required for histological diagnosis and treatment.