Transorbitary intracranial penetrating traumatic injuries are uncommon in the paediatric population, and may occur in the context of domestic, sporting or school accidents. They can extend to skull base and compromise vascular structures such as cavernous sinus and internal carotid.
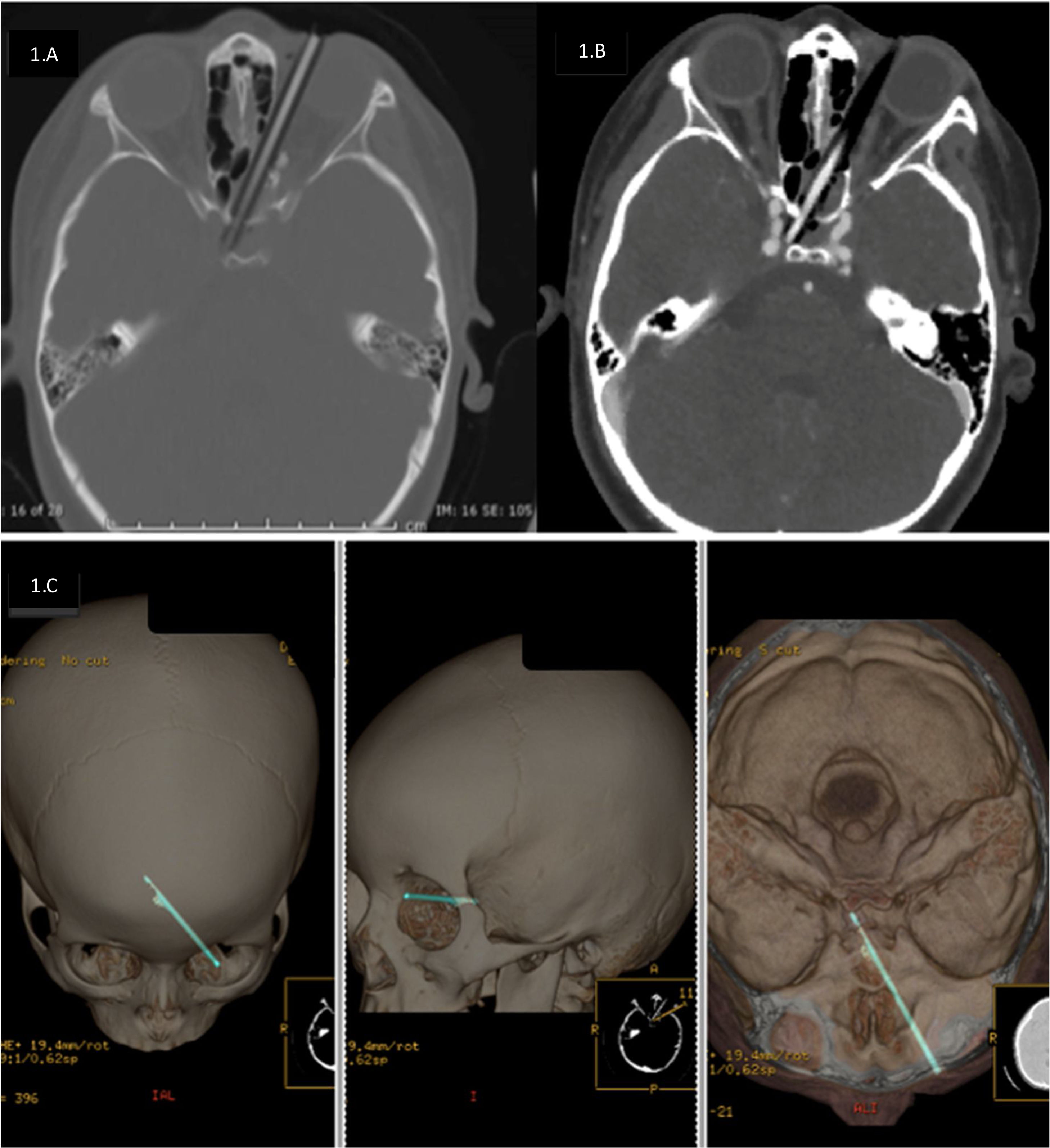
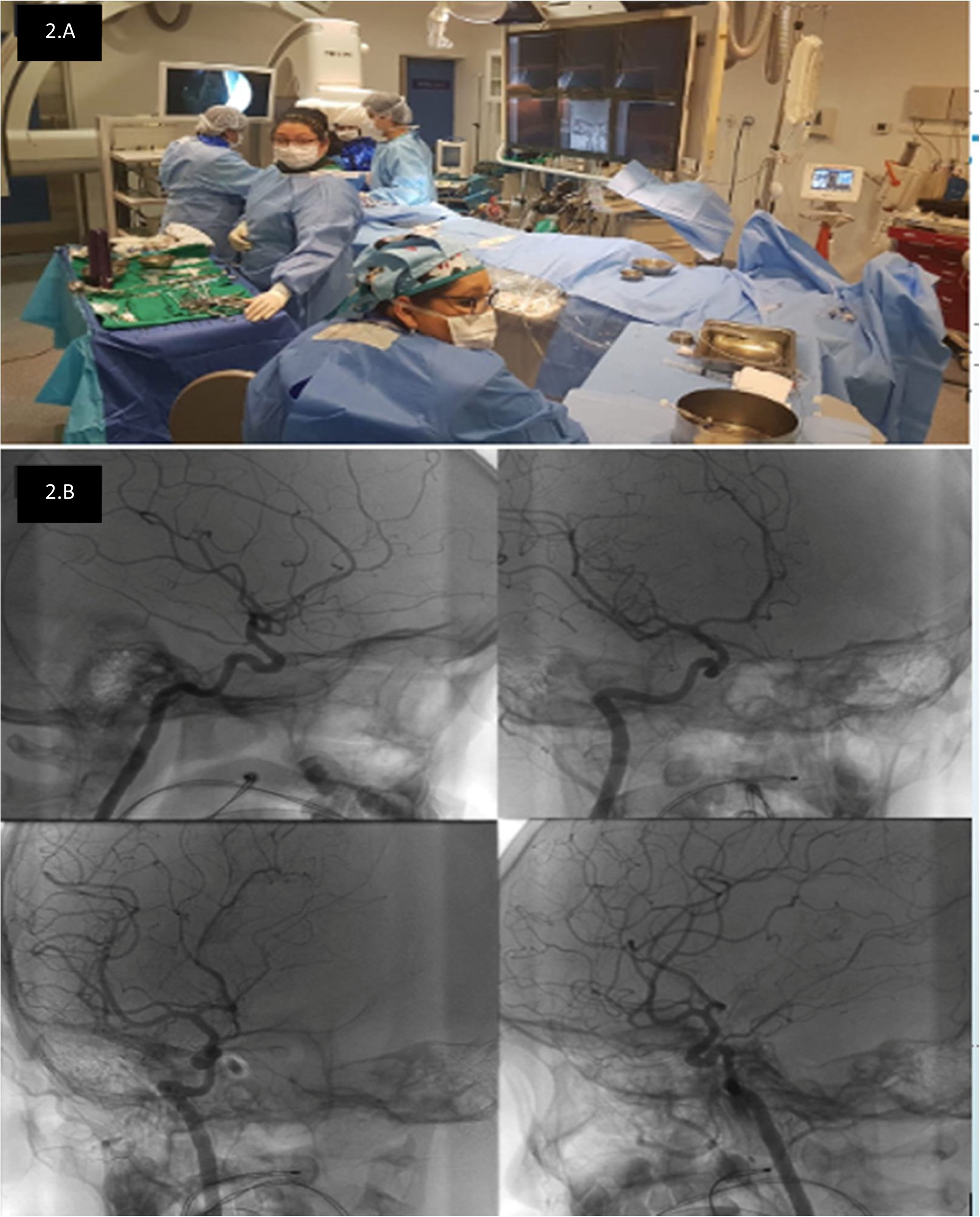
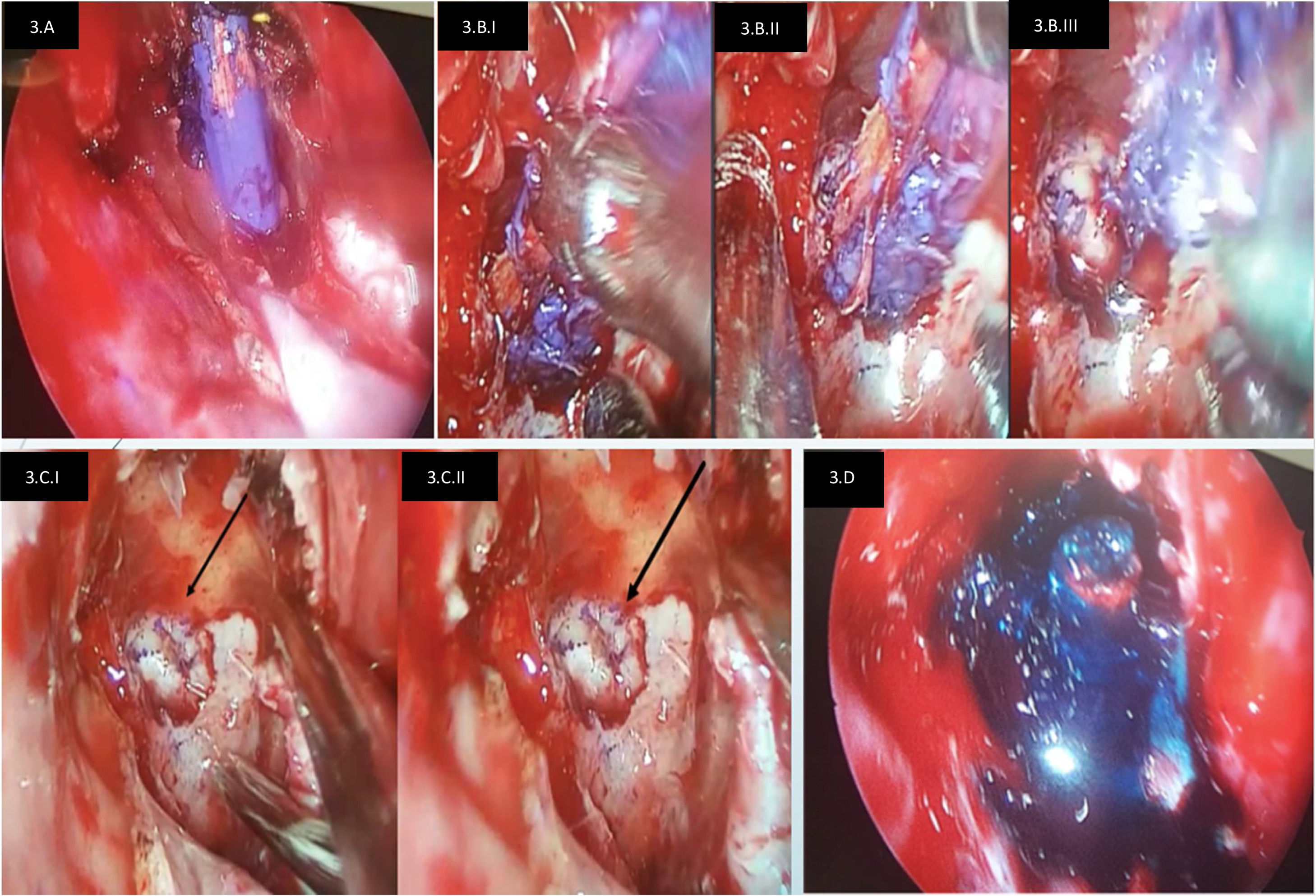
We present a case of 6 years-old girl that suffered an intracranial transorbital penetrating injury with a wooden pencil that crossed from the medial edge of left orbit, transetmoidal and trans-sphenoidal, entering the right sellar region and leaving its end in contact with carotid artery (cavernous segment). After pre-surgical studies, foreign body removal was performed with endoscopic surgery + endovascular control in case of carotid injury. After removing the foreign body, a CSF fistula occurred and was repaired. Patient recovered adequately, without neurological deficit, without postoperative CSF fistula, without CNS infection or oculomotor alteration.
Las lesiones traumáticas penetrantes transorbitarias-intracraneanas, son infrecuentes en población pediátrica, pudiendo ocurrir en el contexto de accidentes domésticos, deportivos o escolares. Pueden extenderse a la base del cráneo y comprometer estructuras vasculares como el seno cavernoso y carótida interna.
Se presenta caso de niña de 6 años de edad, sufre lesión penetrante transorbitaria intracraneal con un lápiz de madera, con trayecto cruzado desde borde medial de órbita izquierda, transetmoidal y transesfenoidal, ingresando a región selar derecha e improntando a arteria carótida derecha (porción cavernosa). Luego de los estudios pre-quirúrgicos, se realizó extirpación de cuerpo extraño con cirugía endoscópica + control endovascular en caso de lesión carotidea. Posterior a resecar cuerpo extraño, se reparó fístula de LCR evidenciada intraoperatoriamente. Paciente se recuperó adecuadamente, sin déficit neurológico, sin fístula postoperatoria de LCR, sin infección del SNC ni alteración oculomotora.
Artículo

Si es la primera vez que accede a la web puede obtener sus claves de acceso poniéndose en contacto con Elsevier España en suscripciones@elsevier.com o a través de su teléfono de Atención al Cliente 902 88 87 40 si llama desde territorio español o del +34 932 418 800 (de 9 a 18h., GMT + 1) si lo hace desde el extranjero.
Si ya tiene sus datos de acceso, clique aquí.
Si olvidó su clave de acceso puede recuperarla clicando aquí y seleccionando la opción "He olvidado mi contraseña".
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora