Compartir
array:24 [
"pii" => "S2529849622000764"
"issn" => "25298496"
"doi" => "10.1016/j.neucie.2022.11.006"
"estado" => "S300"
"fechaPublicacion" => "2023-05-01"
"aid" => "562"
"copyright" => "Sociedad Española de Neurocirugía"
"copyrightAnyo" => "2022"
"documento" => "article"
"crossmark" => 1
"subdocumento" => "fla"
"cita" => "Neurocirugia. 2023;34:139-52"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"Traduccion" => array:1 [
"es" => array:19 [
"pii" => "S113014732200077X"
"issn" => "11301473"
"doi" => "10.1016/j.neucir.2022.08.001"
"estado" => "S300"
"fechaPublicacion" => "2023-05-01"
"aid" => "562"
"copyright" => "Sociedad Española de Neurocirugía"
"documento" => "article"
"crossmark" => 1
"subdocumento" => "fla"
"cita" => "Neurocirugia. 2023;34:139-52"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"es" => array:13 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Artículo especial</span>"
"titulo" => "Consenso sobre guías de tratamiento de gliomas de bajo grado elaborado por el grupo de tumores de la SENEC"
"tienePdf" => "es"
"tieneTextoCompleto" => "es"
"tieneResumen" => array:2 [
0 => "es"
1 => "en"
]
"paginas" => array:1 [
0 => array:2 [
"paginaInicial" => "139"
"paginaFinal" => "152"
]
]
"titulosAlternativos" => array:1 [
"en" => array:1 [
"titulo" => "Low grade gliomas guide-lines elaborated by the tumor section of Spanish Society of Neurosurgery"
]
]
"contieneResumen" => array:2 [
"es" => true
"en" => true
]
"contieneTextoCompleto" => array:1 [
"es" => true
]
"contienePdf" => array:1 [
"es" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:7 [
"identificador" => "fig0005"
"etiqueta" => "Figura 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 2274
"Ancho" => 2508
"Tamanyo" => 293309
]
]
"descripcion" => array:1 [
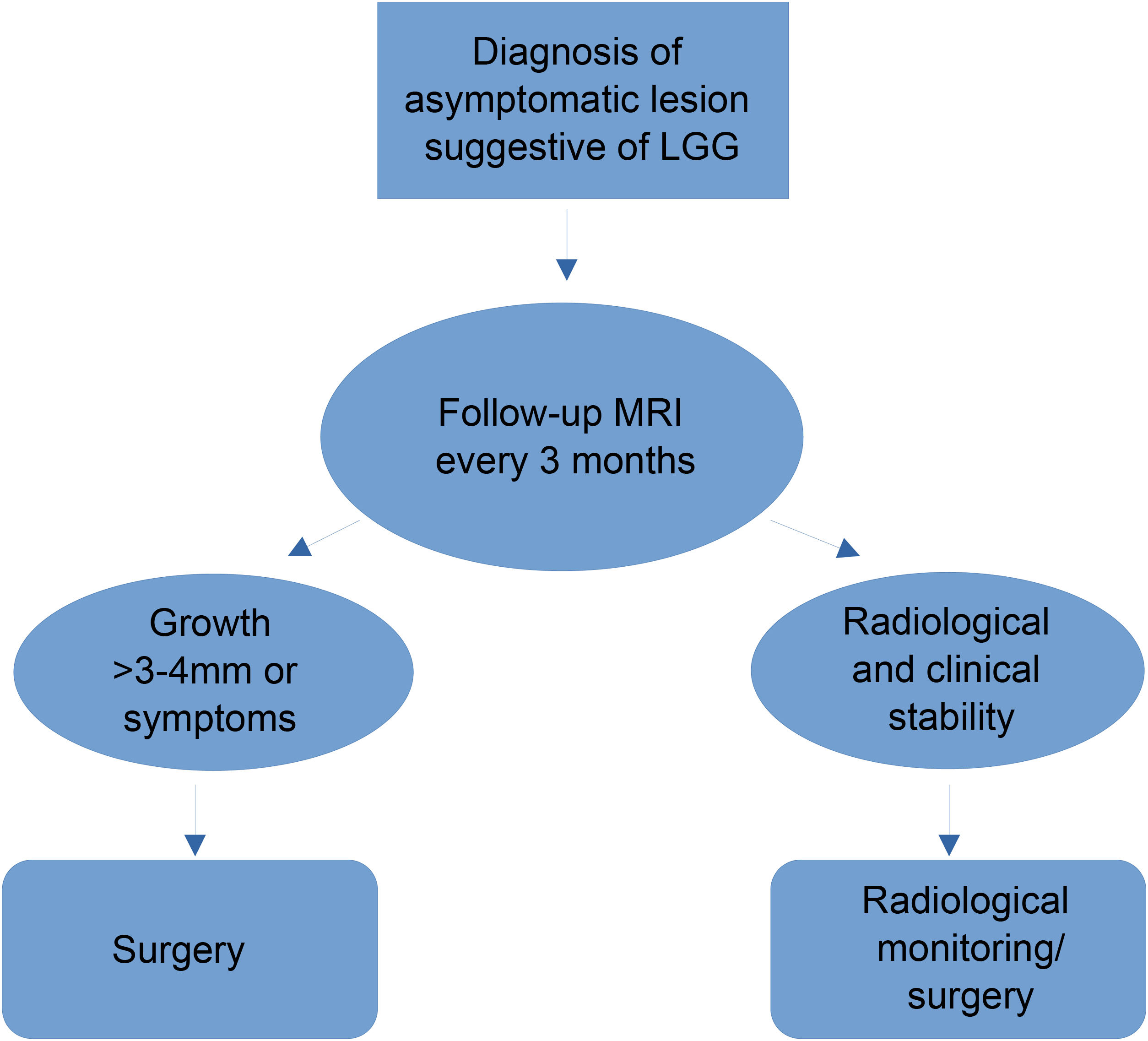
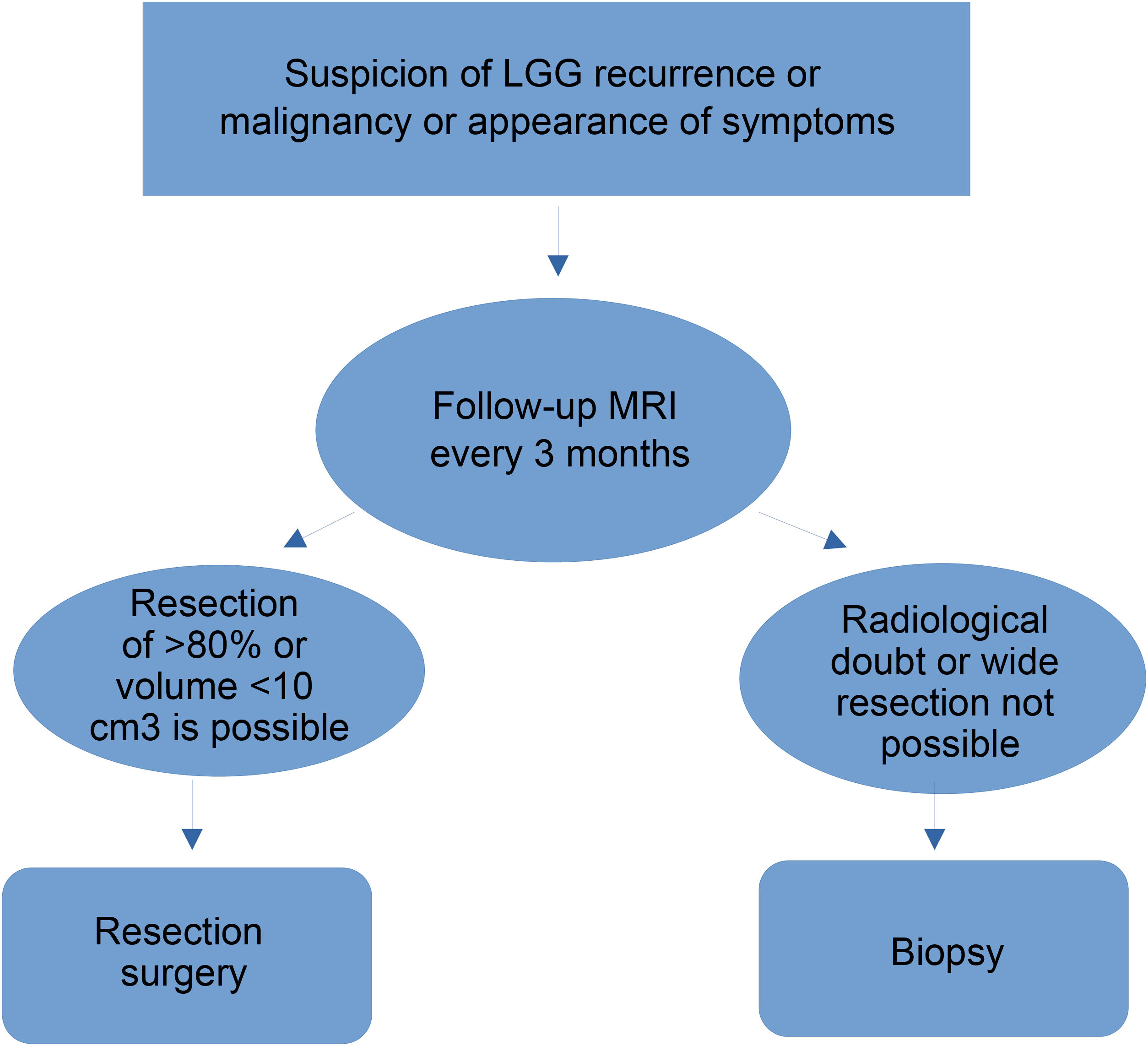
"es" => "<p id="spar0045" class="elsevierStyleSimplePara elsevierViewall">Algoritmo en lesiones asintomáticas sugestivas de gliomas de bajo grado.</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "Sonia Tejada Solís, Josep González Sánchez, Irene Iglesias Lozano, Gerard Plans Ahicart, Angel Pérez Núñez, Leonor Meana Carballo, Jose Luis Gil Salú, Alejandro Fernández Coello, Juan Carlos García Romero, Angel Rodríguez de Lope Llorca, Sara García Duque, Ricardo Díez Valle, Jose Luis Narros Giménez, Ricardo Prat Acín"
"autores" => array:15 [
0 => array:2 [
"nombre" => "Sonia"
"apellidos" => "Tejada Solís"
]
1 => array:2 [
"nombre" => "Josep"
"apellidos" => "González Sánchez"
]
2 => array:2 [
"nombre" => "Irene"
"apellidos" => "Iglesias Lozano"
]
3 => array:2 [
"nombre" => "Gerard"
"apellidos" => "Plans Ahicart"
]
4 => array:2 [
"nombre" => "Angel"
"apellidos" => "Pérez Núñez"
]
5 => array:2 [
"nombre" => "Leonor"
"apellidos" => "Meana Carballo"
]
6 => array:2 [
"nombre" => "Jose Luis"
"apellidos" => "Gil Salú"
]
7 => array:2 [
"nombre" => "Alejandro"
"apellidos" => "Fernández Coello"
]
8 => array:2 [
"nombre" => "Juan Carlos"
"apellidos" => "García Romero"
]
9 => array:2 [
"nombre" => "Angel"
"apellidos" => "Rodríguez de Lope Llorca"
]
10 => array:2 [
"nombre" => "Sara"
"apellidos" => "García Duque"
]
11 => array:2 [
"nombre" => "Ricardo"
"apellidos" => "Díez Valle"
]
12 => array:2 [
"nombre" => "Jose Luis"
"apellidos" => "Narros Giménez"
]
13 => array:2 [
"nombre" => "Ricardo"
"apellidos" => "Prat Acín"
]
14 => array:1 [
"colaborador" => "Grupo de trabajo de la SENEC"
]
]
]
]
]
"idiomaDefecto" => "es"
"Traduccion" => array:1 [
"en" => array:9 [
"pii" => "S2529849622000764"
"doi" => "10.1016/j.neucie.2022.11.006"
"estado" => "S300"
"subdocumento" => ""
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"idiomaDefecto" => "en"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849622000764?idApp=UINPBA00004B"
]
]
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S113014732200077X?idApp=UINPBA00004B"
"url" => "/11301473/0000003400000003/v1_202305030948/S113014732200077X/v1_202305030948/es/main.assets"
]
]
"itemSiguiente" => array:19 [
"pii" => "S2529849622000946"
"issn" => "25298496"
"doi" => "10.1016/j.neucie.2022.11.019"
"estado" => "S300"
"fechaPublicacion" => "2023-05-01"
"aid" => "551"
"copyright" => "Sociedad Española de Neurocirugía"
"documento" => "simple-article"
"crossmark" => 1
"subdocumento" => "crp"
"cita" => "Neurocirugia. 2023;34:153-8"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"en" => array:13 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Case Report</span>"
"titulo" => "Sporadic hemangioblastoma of cauda equina: A case-report and brief literature review"
"tienePdf" => "en"
"tieneTextoCompleto" => "en"
"tieneResumen" => array:2 [
0 => "en"
1 => "es"
]
"paginas" => array:1 [
0 => array:2 [
"paginaInicial" => "153"
"paginaFinal" => "158"
]
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Hemangioblastoma esporádico de cauda equina: aporte de un caso y breve revisión de la literatura"
]
]
"contieneResumen" => array:2 [
"en" => true
"es" => true
]
"contieneTextoCompleto" => array:1 [
"en" => true
]
"contienePdf" => array:1 [
"en" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:7 [
"identificador" => "fig0010"
"etiqueta" => "Fig. 2"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr2.jpeg"
"Alto" => 457
"Ancho" => 756
"Tamanyo" => 72185
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">Intraoperative photo showed an encapsulated tan-red mass was evident, with several nerve rootlet englobed the tumor, arising from a motor rootlet.</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "Salvatore D’Oria, David Giraldi, Vincenzo Fanelli, Vincenzo D’Angelo"
"autores" => array:4 [
0 => array:2 [
"nombre" => "Salvatore"
"apellidos" => "D’Oria"
]
1 => array:2 [
"nombre" => "David"
"apellidos" => "Giraldi"
]
2 => array:2 [
"nombre" => "Vincenzo"
"apellidos" => "Fanelli"
]
3 => array:2 [
"nombre" => "Vincenzo"
"apellidos" => "D’Angelo"
]
]
]
]
]
"idiomaDefecto" => "en"
"Traduccion" => array:1 [
"en" => array:9 [
"pii" => "S113014732200046X"
"doi" => "10.1016/j.neucir.2022.04.001"
"estado" => "S300"
"subdocumento" => ""
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"idiomaDefecto" => "en"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S113014732200046X?idApp=UINPBA00004B"
]
]
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849622000946?idApp=UINPBA00004B"
"url" => "/25298496/0000003400000003/v1_202305031136/S2529849622000946/v1_202305031136/en/main.assets"
]
"itemAnterior" => array:18 [
"pii" => "S2529849622000788"
"issn" => "25298496"
"doi" => "10.1016/j.neucie.2022.11.008"
"estado" => "S300"
"fechaPublicacion" => "2023-05-01"
"aid" => "547"
"documento" => "article"
"crossmark" => 1
"subdocumento" => "rev"
"cita" => "Neurocirugia. 2023;34:128-38"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"en" => array:13 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Review article</span>"
"titulo" => "A meta-analysis of Lateral supraorbital vs mini Pterional approach in the outcome of rupture and unruptured noncomplex aneurysms’ surgery"
"tienePdf" => "en"
"tieneTextoCompleto" => "en"
"tieneResumen" => array:2 [
0 => "en"
1 => "es"
]
"paginas" => array:1 [
0 => array:2 [
"paginaInicial" => "128"
"paginaFinal" => "138"
]
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Metaanálisis entre el abordaje subfrontal y minipterional en los aneurismas cerebrales no complejos"
]
]
"contieneResumen" => array:2 [
"en" => true
"es" => true
]
"contieneTextoCompleto" => array:1 [
"en" => true
]
"contienePdf" => array:1 [
"en" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:7 [
"identificador" => "fig0065"
"etiqueta" => "Fig. 2"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr2.jpeg"
"Alto" => 1091
"Ancho" => 3175
"Tamanyo" => 271786
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">2A: (a) Forest Plot Time of surgery, early (eaOt): Results demonstrate a statistical significant difference between the two groups (OR −0.21, CI 95% −0.59 to 0.18, and <span class="elsevierStyleItalic">p</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>0.04), but with heterogeneity (<span class="elsevierStyleItalic">p</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>0.02 and <span class="elsevierStyleItalic">I</span><span class="elsevierStyleSup">2</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>68.97%); (b) Forest Plot eaOt without “Lan Q et al., 2015”<a class="elsevierStyleCrossRef" href="#bib0200"><span class="elsevierStyleSup">13</span></a> article: Results demonstrate an additionally statistically significant difference between the two groups [OR −0.01, CI 95% −10.42 to −0.39), and <span class="elsevierStyleBold"><span class="elsevierStyleItalic">p</span></span><span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleBold">=</span><span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleBold">0.03</span>]; (c) and (d) Funnel plots of the eaOt in the groups, with (left) or without (right) “Lan Q et al., 2015”<a class="elsevierStyleCrossRef" href="#bib0200"><span class="elsevierStyleSup">13</span></a> article, and with high (left) heterogeneity (<span class="elsevierStyleItalic">p</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>0.02 and <span class="elsevierStyleItalic">I</span><span class="elsevierStyleSup">2</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>68.97%) or with no (right) heterogeneity (<span class="elsevierStyleItalic">p</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>0.93 and <span class="elsevierStyleItalic">I</span><span class="elsevierStyleSup">2</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>−1339.%). <span class="elsevierStyleItalic">Abbreviations</span>: LSO<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>lateral supraorbital and supraorbital craniotomy group, MPT<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>mini pterional craniotomy group, eaOt<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>early time of surgery. 2B: (a) Forest Plot Time of surgery, late (laOt): Results demonstrate a statistical significant difference between the two groups (OR −0.21, CI 95% −0.69 to 0.28, and <span class="elsevierStyleBold"><span class="elsevierStyleItalic">p</span></span><span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleBold">=</span><span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleBold">0.05</span>), but with heterogeneity and thus publication bias (<span class="elsevierStyleItalic">p</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>0.05 and <span class="elsevierStyleItalic">I</span><span class="elsevierStyleSup">2</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>61.74%); and (b) Forest Plot laOt without “Lan Q et al. 2015”<a class="elsevierStyleCrossRef" href="#bib0200"><span class="elsevierStyleSup">13</span></a> article: Results demonstrate an additionally statistically significant difference between the two groups [OR −0.03, CI 95% −0.49 to 0.55, and <span class="elsevierStyleBold"><span class="elsevierStyleItalic">p</span></span><span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleBold">=</span><span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleBold">0.02</span>; (c) and (d) Funnel plots of the laOt in the groups, with (left) or without (right) “Lan Q et al. 2015”<a class="elsevierStyleCrossRef" href="#bib0200"><span class="elsevierStyleSup">13</span></a> article, and with high (left) heterogeneity (<span class="elsevierStyleItalic">p</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>0.05 and <span class="elsevierStyleItalic">I</span><span class="elsevierStyleSup">2</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>61.74%) or with no (right) heterogeneity (<span class="elsevierStyleItalic">p</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>0.98 and <span class="elsevierStyleItalic">I</span><span class="elsevierStyleSup">2</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>−6029.%). <span class="elsevierStyleItalic">Abbreviations</span>: LSO<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>lateral supraorbital and supraorbital craniotomy group, MPT<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>mini pterional craniotomy group, laOt<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>late time of surgery, laOtLSO<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>late time of surgery in LSO group, laOtMPT<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>late time of surgery in MPT group. 2C: (a) Forest Plot Postoperative hemorrhage (Ph): Results demonstrate a statistically significant difference between the two groups group (OR −0.30, CI 95% −0.96 to 0.36, and <span class="elsevierStyleBold"><span class="elsevierStyleItalic">p</span></span><span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleBold">=</span><span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleBold">0.05</span>); (b) Funnel plot of the same parameter demonstrated no heterogeneity (<span class="elsevierStyleItalic">p</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>0.91 and <span class="elsevierStyleItalic">I</span><span class="elsevierStyleSup">2</span><span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>−219.45%). <span class="elsevierStyleItalic">Abbreviations</span>: LSO<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>lateral supraorbital and supraorbital craniotomy group, MPT<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>mini pterional craniotomy group, Ph<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>Postoperative hemorrhage, PhLSO<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>Postoperative hemorrhage in LSO group, PhMPT<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>Postoperative hemorrhage in MPT group.</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "George Fotakopoulos, Hugo Andrade-Barazarte, Brotis Alexandros, Juha Hernesniemi"
"autores" => array:4 [
0 => array:2 [
"nombre" => "George"
"apellidos" => "Fotakopoulos"
]
1 => array:2 [
"nombre" => "Hugo"
"apellidos" => "Andrade-Barazarte"
]
2 => array:2 [
"nombre" => "Brotis"
"apellidos" => "Alexandros"
]
3 => array:2 [
"nombre" => "Juha"
"apellidos" => "Hernesniemi"
]
]
]
]
]
"idiomaDefecto" => "en"
"Traduccion" => array:1 [
"en" => array:9 [
"pii" => "S1130147322000410"
"doi" => "10.1016/j.neucir.2022.03.002"
"estado" => "S300"
"subdocumento" => ""
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"idiomaDefecto" => "en"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S1130147322000410?idApp=UINPBA00004B"
]
]
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849622000788?idApp=UINPBA00004B"
"url" => "/25298496/0000003400000003/v1_202305031136/S2529849622000788/v1_202305031136/en/main.assets"
]
"en" => array:19 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Special article</span>"
"titulo" => "Low grade gliomas guide-lines elaborated by the tumor section of Spanish Society of Neurosurgery"
"tieneTextoCompleto" => true
"paginas" => array:1 [
0 => array:2 [
"paginaInicial" => "139"
"paginaFinal" => "152"
]
]
"autores" => array:1 [
0 => array:4 [
"autoresLista" => "Sonia Tejada Solís, Josep González Sánchez, Irene Iglesias Lozano, Gerard Plans Ahicart, Angel Pérez Núñez, Leonor Meana Carballo, Jose Luis Gil Salú, Alejandro Fernández Coello, Juan Carlos García Romero, Angel Rodríguez de Lope Llorca, Sara García Duque, Ricardo Díez Valle, Jose Luis Narros Giménez, Ricardo Prat Acín"
"autores" => array:15 [
0 => array:4 [
"nombre" => "Sonia"
"apellidos" => "Tejada Solís"
"email" => array:1 [
0 => "stejadasolis@yahoo.es"
]
"referencia" => array:3 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">a</span>"
"identificador" => "aff0005"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
2 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">*</span>"
"identificador" => "cor0005"
]
]
]
1 => array:3 [
"nombre" => "Josep"
"apellidos" => "González Sánchez"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">b</span>"
"identificador" => "aff0010"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
2 => array:3 [
"nombre" => "Irene"
"apellidos" => "Iglesias Lozano"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">c</span>"
"identificador" => "aff0015"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
3 => array:3 [
"nombre" => "Gerard"
"apellidos" => "Plans Ahicart"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">d</span>"
"identificador" => "aff0020"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
4 => array:3 [
"nombre" => "Angel"
"apellidos" => "Pérez Núñez"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">e</span>"
"identificador" => "aff0025"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
5 => array:3 [
"nombre" => "Leonor"
"apellidos" => "Meana Carballo"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">f</span>"
"identificador" => "aff0030"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
6 => array:3 [
"nombre" => "Jose Luis"
"apellidos" => "Gil Salú"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">c</span>"
"identificador" => "aff0015"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
7 => array:3 [
"nombre" => "Alejandro"
"apellidos" => "Fernández Coello"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">d</span>"
"identificador" => "aff0020"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
8 => array:3 [
"nombre" => "Juan Carlos"
"apellidos" => "García Romero"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">g</span>"
"identificador" => "aff0035"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
9 => array:3 [
"nombre" => "Angel"
"apellidos" => "Rodríguez de Lope Llorca"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">h</span>"
"identificador" => "aff0040"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
10 => array:3 [
"nombre" => "Sara"
"apellidos" => "García Duque"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">j</span>"
"identificador" => "aff0050"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
11 => array:3 [
"nombre" => "Ricardo"
"apellidos" => "Díez Valle"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">a</span>"
"identificador" => "aff0005"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
12 => array:3 [
"nombre" => "Jose Luis"
"apellidos" => "Narros Giménez"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">g</span>"
"identificador" => "aff0035"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
13 => array:3 [
"nombre" => "Ricardo"
"apellidos" => "Prat Acín"
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">j</span>"
"identificador" => "aff0050"
]
1 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">i</span>"
"identificador" => "aff0045"
]
]
]
14 => array:1 [
"colaborador" => "Working Group of the SENEC"
]
]
"afiliaciones" => array:10 [
0 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Universitario Fundación Jiménez Díaz, Madrid, Spain"
"etiqueta" => "a"
"identificador" => "aff0005"
]
1 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Clínic i Provincial de Barcelona, Barcelona, Spain"
"etiqueta" => "b"
"identificador" => "aff0010"
]
2 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Universitario Puerta del Mar, Cádiz, Spain"
"etiqueta" => "c"
"identificador" => "aff0015"
]
3 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Universitari Bellvitge, Barcelona, Spain"
"etiqueta" => "d"
"identificador" => "aff0020"
]
4 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Universitario 12 de Octubre, Madrid, Spain"
"etiqueta" => "e"
"identificador" => "aff0025"
]
5 => array:3 [
"entidad" => "Departamento de Neurocirugía, Centro Médico de Asturias, Oviedo, Spain"
"etiqueta" => "f"
"identificador" => "aff0030"
]
6 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Virgen del Rocío, Sevilla, Spain"
"etiqueta" => "g"
"identificador" => "aff0035"
]
7 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Virgen de la Salud, Toledo, Spain"
"etiqueta" => "h"
"identificador" => "aff0040"
]
8 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Universitario HM Montepríncipe, Madrid, Spain"
"etiqueta" => "i"
"identificador" => "aff0045"
]
9 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Universitario La Fe, Valencia, Spain"
"etiqueta" => "j"
"identificador" => "aff0050"
]
]
"correspondencia" => array:1 [
0 => array:3 [
"identificador" => "cor0005"
"etiqueta" => "⁎"
"correspondencia" => "<span class="elsevierStyleItalic">Corresponding author</span>."
]
]
]
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Consenso sobre guías de tratamiento de gliomas de bajo grado elaborado por el grupo de tumores de la SENEC"
]
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:8 [
"identificador" => "fig0005"
"etiqueta" => "Figure 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 2274
"Ancho" => 2508
"Tamanyo" => 274492
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0005"
"detalle" => "Figure "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Algorithm in asymptomatic lesions suggestive of low-grade gliomas.</p>"
]
]
]
"textoCompleto" => "<span class="elsevierStyleSections"><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0025">Introduction</span><p id="par0005" class="elsevierStylePara elsevierViewall">Low-grade gliomas (LGGs) in adults are tumors that originate from the glial cells of the brain, the management of which causes great controversy today, from their diagnosis, to the treatment and subsequent follow-up of these patients. That is what prompted the Grupo de Tumores de la Sociedad Española de Neurocirugía (GT-SENEC) [Spanish Society of Neurosurgery Tumor Group] to hold a consensus meeting, in which the most relevant neurosurgical issues were discussed and recommendations were reached, based on the best scientific evidence. This manuscript offers a summary of the overall management of this pathology, and aims to serve as a guide or as a reference for professionals who treat patients with LGG.</p><p id="par0010" class="elsevierStylePara elsevierViewall">LGG is a tumor usually diagnosed in young adults. The onset of the disease generally takes the form of an epileptic seizure, and patients do not usually present neurological or neuropsychological involvement during diagnosis. It is accepted that LGG is an incurable and slowly progressive disease with an average tumor growth of about 3−4 mm per year. Median survival after diagnosis ranges from 7 to 10 years and there is a common tendency to malignancy when it is left untreated (<a class="elsevierStyleCrossRefs" href="#fig0005">Figs. 1 and 2</a>).</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><elsevierMultimedia ident="fig0010"></elsevierMultimedia></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0030">Initial management of low-grade gliomas</span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0035">Diagnosis and treatment of asymptomatic lesions suggestive of low-grade glioma</span><p id="par0015" class="elsevierStylePara elsevierViewall">Incidental low-grade glioma (iLGG) is defined as a brain lesion diagnosed by imaging tests without symptoms attributable to it. Its management is controversial, given the limited scientific evidence available.</p><p id="par0020" class="elsevierStylePara elsevierViewall">The incidence of incidental brain lesions has increased in recent years due to the increasing use of magnetic resonance imaging. Weber and Knopf demonstrated in 2006, with a study carried out on 2389 healthy volunteers, an incidence of low-grade glial lesions between 0.05% and 0.2%<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a>. Another study by Jansen et al. in 2017 described a 0.10% incidence of these lesions in children<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a>.</p><p id="par0025" class="elsevierStylePara elsevierViewall">Although there is little literature on the subject, one of the most studied aspects of these lesions is their natural history. According to different studies, iLGGs present a continuous spectrum from their biological birth (pre-radiological phase), possible detection in imaging tests (silent radiological phase) and symptomatic transformation phase. The silent period can be up to 15 years, and some authors believe that early treatment during this period could improve the prognosis of the disease and prevent malignancy, and some even suggest it could be a cure<a class="elsevierStyleCrossRef" href="#bib0015"><span class="elsevierStyleSup">3</span></a>. In what has been published on the natural history of iLGGs, a growth rate very similar to non-incidental lesions of around 3−4 mm per year is also described. Regarding this parameter, the recommendation in the literature is to analyse tumor growth from the tumor diameter derived from serial volumetric tumor growth<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a>.</p><p id="par0030" class="elsevierStylePara elsevierViewall">In relation to the characteristics of iLGGs, authors such as Pallud et al. and Potts et al. have compared series of incidental lesions with symptomatic cases and shown that the former are more common lesions in young women, in the non-dominant hemisphere, with smaller volume, less extension (<1 lobe) and invasion of the corpus callosum, less contrast uptake, shorter interval until oncological treatment, higher percentages of total resection, as well as higher overall survival (OS), disease-free period and malignancy-free period<a class="elsevierStyleCrossRefs" href="#bib0020"><span class="elsevierStyleSup">4,5</span></a>.</p><p id="par0035" class="elsevierStylePara elsevierViewall">All these data allow us to establish treatment recommendations, which are not exempt from controversy. On the one hand, the authors agree on the need for monitoring by magnetic resonance imaging (MRI) of any iLGG. With the exception of studies such as the one by Wijnenga et al. of 2017<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">6</span></a>, in which they describe the non-existence of significant differences between the surgical and conservative treatment of these lesions, in general the majority of authors opt for early preventive surgery based on lesion growth observed in follow-up MRI scans between three and nine months after diagnosis. Some authors, such as Duffau, have even proposed, not without controversy, the need to introduce population screening for these lesions in young individuals<a class="elsevierStyleCrossRefs" href="#bib0035"><span class="elsevierStyleSup">7,8</span></a>.</p><p id="par0040" class="elsevierStylePara elsevierViewall">Regarding surgical treatment, Duffau et al. say that this needs to be carried out early, using intraoperative monitoring techniques and in hospitals that have specialised equipment. This group also insists that supratotal resection<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">9</span></a>, extended beyond the tumor borders detectable on MRI, should be considered, since they are non-quiescent lesions that in up to 27% of cases present foci of increased grade at diagnosis.</p><p id="par0045" class="elsevierStylePara elsevierViewall">The literature on molecular biology of iLGG is scarce, but there are two studies that stand out. On the one hand, Zhang et al. describe a series of 22 cases in which the majority of iLGGs are IDH1-mutant and 1p/19q codeleted (oligodendroglial lineage)<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">10</span></a>. On the other hand, in a more recent study by Ius et al. in which iLGG cases are compared with symptomatic cases, no significant differences are shown in the molecular profile of both groups, detecting a higher incidence of 1p19q codeletions in the iLGG group. These findings contrast with a higher OS in the iLGG group that is attributed to the higher rate of total resections<a class="elsevierStyleCrossRef" href="#bib0055"><span class="elsevierStyleSup">11</span></a>.</p><p id="par0050" class="elsevierStylePara elsevierViewall">In conclusion, iLGG is an increasingly diagnosed condition. It represents an early stage in the natural history of the disease with certain clinical-radiological (lower volume, eloquence), therapeutic (higher rate of total resection) and molecular biology (IDHmut and 1p19q codeletion) advantages. This means that the most accepted therapeutic recommendation is early surgical resection if, after initial follow-up with MRI at 3, 6 and 9 months, significant growth equal to or greater than 3−4 mm is demonstrated. Population screening and supratotal resection represent currently unresolved points of controversy. Multicentre prospective studies are necessary to increase the evidence in the treatment of iLGG.</p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0040">Histological and molecular classification of low-grade gliomas</span><p id="par0055" class="elsevierStylePara elsevierViewall">The classification of central nervous system tumors based on their molecular profile represented a paradigm shift in the 2016 World Health Organization (WHO) classification<a class="elsevierStyleCrossRef" href="#bib0060"><span class="elsevierStyleSup">12</span></a>, in which low-grade glial lesions were grouped according to molecular criteria<a class="elsevierStyleCrossRef" href="#bib0065"><span class="elsevierStyleSup">13</span></a>. In this way, tumors belonging to the same group share biological and prognostic characteristics. Based on this classification, the following molecular markers are necessary to establish the diagnosis of LGG:<ul class="elsevierStyleList" id="lis0005"><li class="elsevierStyleListItem" id="lsti0005"><span class="elsevierStyleLabel">1</span><p id="par0060" class="elsevierStylePara elsevierViewall">IDH1 R132 or IDH2 R172: the mutation in IDH is the genetic marker of astrocytomas and oligodendrogliomas<a class="elsevierStyleCrossRef" href="#bib0070"><span class="elsevierStyleSup">14</span></a>. It also has prognostic significance, with IDH-mutated lesions presenting a better prognosis<a class="elsevierStyleCrossRef" href="#bib0075"><span class="elsevierStyleSup">15</span></a>. The most common mutation is in codon R132 of IDH1 (90%), which is determined by immunohistochemical techniques. However, in those lesions with no IDH mutation, sequencing is indicated to assess other less common mutations, except in patients over 55 years of age with suspected glioblastoma or midline gliomas<a class="elsevierStyleCrossRef" href="#bib0060"><span class="elsevierStyleSup">12</span></a>.</p></li><li class="elsevierStyleListItem" id="lsti0010"><span class="elsevierStyleLabel">2</span><p id="par0065" class="elsevierStylePara elsevierViewall">1p19q codeletion: genetic <span class="elsevierStyleBold">marker</span> of oligodendrogliomas<a class="elsevierStyleCrossRefs" href="#bib0080"><span class="elsevierStyleSup">16,17</span></a>, with prognostic and predictive significance. They are lesions with a better prognosis and with a good response to treatment with alkylating agents<a class="elsevierStyleCrossRef" href="#bib0090"><span class="elsevierStyleSup">18</span></a>. They can be determined by FISH or loss of heterozygosity (LOH)<a class="elsevierStyleCrossRefs" href="#bib0095"><span class="elsevierStyleSup">19–21</span></a>.</p></li><li class="elsevierStyleListItem" id="lsti0015"><span class="elsevierStyleLabel">3</span><p id="par0070" class="elsevierStylePara elsevierViewall">Nuclear loss of ATRX: it is a diagnostic indicator of astrocytic tumor together with the mutation in IDH. It is determined by immunohistochemical techniques<a class="elsevierStyleCrossRefs" href="#bib0110"><span class="elsevierStyleSup">22,23</span></a>.</p></li><li class="elsevierStyleListItem" id="lsti0020"><span class="elsevierStyleLabel">4</span><p id="par0075" class="elsevierStylePara elsevierViewall">TERT promoter mutation: it is a marker of good prognosis in patients with oligodendroglial lesions with 1p19q codeletion and IDH mutation<a class="elsevierStyleCrossRefs" href="#bib0120"><span class="elsevierStyleSup">24,25</span></a>.</p></li><li class="elsevierStyleListItem" id="lsti0025"><span class="elsevierStyleLabel">5</span><p id="par0080" class="elsevierStylePara elsevierViewall">Mutation in p53: mutations in the p53 tumor suppressor gene are characteristic of IDH-mutated astrocytomas, but not necessary for their diagnosis.</p></li></ul></p><p id="par0085" class="elsevierStylePara elsevierViewall">IDH-mutated astrocytomas usually show nuclear loss of ATRX, mutations in p53 and absence of 1p19q codeletion. In fact, the detection of nuclear loss in ATRX and the presence of IDH mutation are sufficient for the diagnosis of astrocytic tumor, without the need for codeletion analysis. Similarly, the nuclear retention of ATRX and the IDH mutation make it necessary to determine the codeletion to distinguish an astrocytic tumor from an oligodendroglial one.</p><p id="par0090" class="elsevierStylePara elsevierViewall">Nuclear loss of ATRX and 1p19q codeletion are mutually exclusive, so if there is 1p19q codeletion, ATRX immunohistochemistry is not necessary.</p><p id="par0095" class="elsevierStylePara elsevierViewall">The fifth edition of the WHO classification, published in 2021, reaffirms the importance of molecular characterisation in the diagnosis of central nervous system tumors, as well as integrated diagnosis<a class="elsevierStyleCrossRef" href="#bib0130"><span class="elsevierStyleSup">26</span></a>. In addition, it establishes important modifications in terms of the nomenclature and grade of tumors. One of the most important changes is the use of Arabic numerals, instead of Roman numerals. This is intended to accentuate biological similarities and bring the classification closer to that of other tumors that do not belong to the central nervous system.</p><p id="par0100" class="elsevierStylePara elsevierViewall">In the new classification, LGGs belong to the group “Gliomas, glioneuronal tumors and neuronal tumors”, to which six families belong, including adult-type diffuse gliomas. Within this group we find three types of tumor<a class="elsevierStyleCrossRef" href="#bib0130"><span class="elsevierStyleSup">26</span></a>, defining the genetic-molecular profile for each of them:<ul class="elsevierStyleList" id="lis0010"><li class="elsevierStyleListItem" id="lsti0030"><span class="elsevierStyleLabel">•</span><p id="par0105" class="elsevierStylePara elsevierViewall">IDH-mutated astrocytomas (grades 2–4): IDH1, IDH2, ATRX, TP53, CDKN2A/B.</p></li><li class="elsevierStyleListItem" id="lsti0035"><span class="elsevierStyleLabel">•</span><p id="par0110" class="elsevierStylePara elsevierViewall">IDH-mutated and 1p19q-codeleted oligodendrogliomas (grades 2–3): IDH1, IDH2, 1p19q, TERT promoter, CIC1, FUBP1, NOTCH1.</p></li><li class="elsevierStyleListItem" id="lsti0040"><span class="elsevierStyleLabel">•</span><p id="par0115" class="elsevierStylePara elsevierViewall">IDH-WT glioblastomas (grade 4): IDH-wildtype, TERT promoter, chromosomes 7/10, EGFR.</p></li></ul></p><p id="par0120" class="elsevierStylePara elsevierViewall">It should be noted that now, therefore, all IDH-mutated astrocytomas are a single tumor, with grades 2–4, with the term anaplastic astrocytoma or IDH-mutated glioblastoma disappearing.</p><p id="par0125" class="elsevierStylePara elsevierViewall">As for diffuse gliomas in the paediatric age, they are now more precisely defined molecularly, differentiating between low-grade and high-grade diffuse paediatric-type gliomas.</p><span id="sec0025" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0045">Grades of recommendation<a class="elsevierStyleCrossRef" href="#bib0135"><span class="elsevierStyleSup">27</span></a></span><p id="par0130" class="elsevierStylePara elsevierViewall"><ul class="elsevierStyleList" id="lis0015"><li class="elsevierStyleListItem" id="lsti0045"><span class="elsevierStyleLabel">•</span><p id="par0135" class="elsevierStylePara elsevierViewall">LGG classification should follow the most recent WHO classification, supplemented by the cIMPACT-NOW update<a class="elsevierStyleCrossRef" href="#bib0140"><span class="elsevierStyleSup">28</span></a>. <span class="elsevierStyleItalic">Grade of recommendation: IV. Level of evidence: B.</span></p></li><li class="elsevierStyleListItem" id="lsti0050"><span class="elsevierStyleLabel">•</span><p id="par0140" class="elsevierStylePara elsevierViewall">Immunohistochemical determination of the R132 mutation in IDH1 and nuclear loss of ATRX should be performed routinely in the diagnostic evaluation of diffuse gliomas. <span class="elsevierStyleItalic">Grade of recommendation: IV. Level of evidence: B.</span></p></li><li class="elsevierStyleListItem" id="lsti0055"><span class="elsevierStyleLabel">•</span><p id="par0145" class="elsevierStylePara elsevierViewall">If the immunohistochemistry of R132 in IDH1 is negative, the sequencing of codon 132 in IDH1 and codon 172 in IDH2 should be performed in astrocytic and oligodendroglial tumors grades II-III, as well as in glioblastomas in patients aged <55 years <span class="elsevierStyleItalic">Grade of recommendation: IV. Level of evidence: B.</span></p></li><li class="elsevierStyleListItem" id="lsti0060"><span class="elsevierStyleLabel">•</span><p id="par0150" class="elsevierStylePara elsevierViewall">1p19q codeletion should be determined in all IDH-mutated lesions with nuclear retention of ATRX. <span class="elsevierStyleItalic">Grade of recommendation: II. Level of evidence: B.</span></p></li></ul></p></span></span><span id="sec0030" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0050">Low-grade glioma (LGG) surgery</span><p id="par0155" class="elsevierStylePara elsevierViewall">LGGs usually extend to brain regions considered eloquent<a class="elsevierStyleCrossRef" href="#bib0145"><span class="elsevierStyleSup">29</span></a>, so adequate pre-surgical planning is essential for optimal surgical performance. Functional brain MRI and tractography is recommended to determine the tumor's anatomical relationship with motor, language or other eloquent areas that are at risk of being injured. During the surgical intervention, the intraoperative use of brain mapping techniques and neurophysiological monitoring is recommended<a class="elsevierStyleCrossRefs" href="#bib0150"><span class="elsevierStyleSup">30,31</span></a>.</p><p id="par0160" class="elsevierStylePara elsevierViewall">The goals of LGG surgery are to achieve a complete or widest possible resection of the tumor while preserving neurological functions, to have a pathological and molecular diagnosis of the tumor, to treat epilepsy, to increase progression-free survival (PFS), to delay anaplastic transformation of the tumor (mPFS) and increase OS.</p><p id="par0165" class="elsevierStylePara elsevierViewall">Despite the fact that surgery is, in general, the first therapeutic option to consider, in most published review studies<a class="elsevierStyleCrossRef" href="#bib0160"><span class="elsevierStyleSup">32</span></a> and in clinical practice guidelines<a class="elsevierStyleCrossRefs" href="#bib0135"><span class="elsevierStyleSup">27,33</span></a>, there is no level 1 scientific evidence regarding the impact of surgery in the natural history of LGGs, since the data come from case series, retrospective studies or studies with historical controls and include a heterogeneity of tumors with different prognosis.</p><p id="par0170" class="elsevierStylePara elsevierViewall">It is accepted that a higher degree of tumor resection implies a longer survival of patients with LGG (level C recommendation). In a study review, 82% of the studies reviewed that related the degree of tumor resection with OS showed a positive impact, especially in cases of complete resection<a class="elsevierStyleCrossRef" href="#bib0160"><span class="elsevierStyleSup">32</span></a>.</p><p id="par0175" class="elsevierStylePara elsevierViewall">The effect of surgery on local disease control (PFS and mPFS) is clearer (level 2 recommendation). In the same study review, 90% of the studies reviewed that related the degree of tumor resection with PFS showed a positive impact, especially when complete resection was achieved.</p><p id="par0180" class="elsevierStylePara elsevierViewall">Despite the optimisation of intraoperative techniques to achieve a greater degree of tumor resection, including neuronavigation or intraoperative magnetic resonance imaging, the percentage of patients with LGG in whom a complete resection is achieved does not exceed 70%<a class="elsevierStyleCrossRef" href="#bib0170"><span class="elsevierStyleSup">34</span></a>.</p><p id="par0185" class="elsevierStylePara elsevierViewall">In this context, there is no clear consensus on the minimum percentage of tumor resection that is necessary to achieve an oncological impact and increase OS and PFS<a class="elsevierStyleCrossRef" href="#bib0165"><span class="elsevierStyleSup">33</span></a>, although it is accepted that a therapeutic benefit is obtained with tumor resections greater than 80%<a class="elsevierStyleCrossRef" href="#bib0170"><span class="elsevierStyleSup">34</span></a>. Some authors indicate a biopsy for diagnostic purposes if, based on preoperative studies, the estimated resection percentage will not exceed 50%<a class="elsevierStyleCrossRef" href="#bib0175"><span class="elsevierStyleSup">35</span></a>.</p><p id="par0190" class="elsevierStylePara elsevierViewall">If a biopsy is proposed, it is recommended that advanced neuroimaging techniques (spectroscopy, perfusion or PET) be used to choose the tumor area to be biopsied<a class="elsevierStyleCrossRef" href="#bib0180"><span class="elsevierStyleSup">36</span></a> and reduce the risk of under-diagnosing the tumor grade<a class="elsevierStyleCrossRefs" href="#bib0185"><span class="elsevierStyleSup">37,38</span></a>.</p><p id="par0195" class="elsevierStylePara elsevierViewall">It should be noted that the percentage of resection is a relative variable and possibly the most important data to take into account is the residual tumor volume after surgery<a class="elsevierStyleCrossRef" href="#bib0135"><span class="elsevierStyleSup">27</span></a>. A lower percentage of recurrence, a higher PFS and a lower tendency to malignancy of the tumor (mPFS) have been observed if the residual volume after surgery is less than 10 cm<span class="elsevierStyleSup">3</span><a class="elsevierStyleCrossRefs" href="#bib0175"><span class="elsevierStyleSup">35,39</span></a>. Regarding OS, most studies show a longer survival of patients in cases of complete tumor resection or residual tumor volume of less than 5 cm<span class="elsevierStyleSup">3</span><a class="elsevierStyleCrossRefs" href="#bib0200"><span class="elsevierStyleSup">40,41</span></a>. Other studies show a positive impact on OS if the tumor volume is less than 15 cm<span class="elsevierStyleSup">3</span><a class="elsevierStyleCrossRef" href="#bib0210"><span class="elsevierStyleSup">42</span></a>.</p><p id="par0200" class="elsevierStylePara elsevierViewall">Regarding the control of epileptic seizures, some authors have shown good control of tumor-related epilepsy in the case of partial resections as long as the resection is greater than 80%<a class="elsevierStyleCrossRef" href="#bib0215"><span class="elsevierStyleSup">43</span></a>, 90% or a residual tumor volume of less than 19 cm<span class="elsevierStyleSup">3</span><a class="elsevierStyleCrossRef" href="#bib0220"><span class="elsevierStyleSup">44</span></a>.</p><p id="par0205" class="elsevierStylePara elsevierViewall">LGGs are considered an infiltrative disease. Tumor cells have been shown to exist between 10 and 20 mm beyond the tumor border defined by nuclear magnetic resonance (NMR)<a class="elsevierStyleCrossRef" href="#bib0225"><span class="elsevierStyleSup">45</span></a>. For this reason, some authors propose performing a supratotal tumor resection in those cases in which it is possible<a class="elsevierStyleCrossRefs" href="#bib0230"><span class="elsevierStyleSup">46,47</span></a>. In a group of 16 patients who underwent supratotal resection with 11 years of follow-up, the PFS at five years was 75% (higher than the expected average). In half of the patients, there was progression during follow-up, with a mean recurrence of 70.3 months (32−105 m)<a class="elsevierStyleCrossRef" href="#bib0240"><span class="elsevierStyleSup">48</span></a>.</p><p id="par0210" class="elsevierStylePara elsevierViewall">Despite the fact that at the present time there is not enough scientific evidence to recommend supratotal tumor resection<a class="elsevierStyleCrossRef" href="#bib0245"><span class="elsevierStyleSup">49</span></a>, recently published studies have shown a greater oncological benefit compared to total or partial resections<a class="elsevierStyleCrossRef" href="#bib0235"><span class="elsevierStyleSup">47</span></a>.</p></span><span id="sec0035" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0055">Differential role of surgery for low-grade gliomas based on their molecular profile</span><p id="par0215" class="elsevierStylePara elsevierViewall">The incorporation of molecular diagnosis into the classification of adult brain gliomas aroused interest in the role that surgery could have in each molecular subgroup of LGGs. Thus, various studies appeared, mostly retrospective and with significant heterogeneity among them in terms of the type of patients, methodology and precision of the evaluation of surgical resection (volumetric, qualitative studies, population registries…).</p><p id="par0220" class="elsevierStylePara elsevierViewall">In gliomas with IDH mutation and without 1p-19q codeletion (diffuse astrocytomas with IDH mutation), there is unanimity about the beneficial effect of surgery.</p><p id="par0225" class="elsevierStylePara elsevierViewall">In those studies with volumetric analysis of the resection, there is consensus that the absence of tumor remnants is better than the presence of any tumor remnant, and that in residual volumes below 15 cm<span class="elsevierStyleSup">3</span>, the smaller the tumor remnant, the greater the survival benefit<a class="elsevierStyleCrossRefs" href="#bib0030"><span class="elsevierStyleSup">6,50–52</span></a>.</p><p id="par0230" class="elsevierStylePara elsevierViewall">In gliomas with IDH mutation and 1p19q codeletion (oligodendrogliomas), there is less agreement on the effect of surgery. Among the studies that show no benefit, those that do not perform a volumetric analysis of the degree of resection predominate<a class="elsevierStyleCrossRefs" href="#bib0265"><span class="elsevierStyleSup">53–56</span></a>. Among those that do, there is agreement that surgery improves survival, although they suggest that small tumor remnants may not have a worse impact than complete resections on medium-term progression<a class="elsevierStyleCrossRef" href="#bib0275"><span class="elsevierStyleSup">55</span></a>. In this case, the study is also on a group of patients with molecularly homogeneous tumors, but nevertheless the average survival is around 16 years. None of these studies exceeds a mean follow-up of 10 years, so the analysis of the influence of any treatment on OS may be compromised, as previous clinical trials in gliomas have shown<a class="elsevierStyleCrossRefs" href="#bib0285"><span class="elsevierStyleSup">57,58</span></a>.</p><p id="par0235" class="elsevierStylePara elsevierViewall">Finally, in the case of LGGs without IDH mutation, the results are contradictory, although studies showing a benefit of surgery predominate<a class="elsevierStyleCrossRefs" href="#bib0250"><span class="elsevierStyleSup">50–53,59,60</span></a>. The detection of this benefit may be reduced by the low number of cases in each series, since they represent around 20% of these tumors and include patients with very different survival rates<a class="elsevierStyleCrossRef" href="#bib0305"><span class="elsevierStyleSup">61</span></a>. It is currently recognised that this is a very heterogeneous molecular group that includes diffuse astrocytomas with molecular characteristics of glioblastoma (pTERT mutation, EGFR amplifications, chromosome 7 gain + chromosome 10 loss), diffuse gliomas typical of paediatric age and even circumscribed gliomas<a class="elsevierStyleCrossRefs" href="#bib0310"><span class="elsevierStyleSup">62,63</span></a>.</p><p id="par0240" class="elsevierStylePara elsevierViewall">In conclusion, the data available in the literature do not allow us to affirm that there is a differential role of surgery in terms of survival benefit, and the principle of "maximum safe resection" currently recommended in all treatment guidelines should be applied to the group of diffuse low-grade gliomas in adults. In light of the improvements provided by molecular diagnosis in the classification of gliomas, future studies aimed at assessing the therapeutic value of surgical resection should include homogeneous groups of patients, an objective evaluation of the resection, and follow-up according to the expected survival.</p></span><span id="sec0040" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0060">Radiotherapy in low-grade gliomas</span><p id="par0245" class="elsevierStylePara elsevierViewall">Radiotherapy is one of the main components in the treatment of patients with LGG. Its objective is to improve local control by reducing neurotoxicity and increasing survival, as several clinical trials have shown<a class="elsevierStyleCrossRefs" href="#bib0320"><span class="elsevierStyleSup">64,65</span></a>.</p><p id="par0250" class="elsevierStylePara elsevierViewall">In terms of dose and treatment schedule, current recommendations state that low doses of irradiation are equivalent to high doses (45–50.4 versus 59.4–64.8 Gy) in the treatment of LGG with postoperative radiotherapy, which also reduces toxicity<a class="elsevierStyleCrossRefs" href="#bib0330"><span class="elsevierStyleSup">66,67</span></a>. There is no evidence to suggest an additional benefit of high-dose versus low-dose radiation in patients with LGG<a class="elsevierStyleCrossRef" href="#bib0340"><span class="elsevierStyleSup">68</span></a>. Radiotherapy should be given around four weeks after surgery and is commonly given in daily fractions of 1.8–2 Gy. Hypofractionated radiotherapy with a higher dose per fraction and a lower total dose (e.g.15 × 2.67 Gy) would be appropriate in older patients (>65-70 years) or in those with a poor prognosis (Karnosky <70)<a class="elsevierStyleCrossRef" href="#bib0345"><span class="elsevierStyleSup">69</span></a>.</p><p id="par0255" class="elsevierStylePara elsevierViewall">Macroscopic tumor volume is defined as the area of the surgical site plus residual tumor area identified on T1-, T2-, and FLAIR-weighted MRI sequences. To this, a margin of 1.0–2.0 cm (microscopic invasion) is added, creating the target clinical volume, which is usually modified to include abnormalities visualised on T2 or FLAIR (e.g. oedema) and restrict anatomical barriers such as ventricles, tentorium and falx. Finally, another margin of 0.3 to 0.5 cm is added, to allow for uncertainties in patient set-up and treatment delivery, thereby establishing the final planned target volume<a class="elsevierStyleCrossRef" href="#bib0350"><span class="elsevierStyleSup">70</span></a>. Structures at greatest risk of radiotherapy toxicity, such as the retina, lens, hippocampus, pituitary gland, cochlea, brainstem, optic nerves and chiasm, should be delineated.</p><p id="par0260" class="elsevierStylePara elsevierViewall">The decision of when to proceed with radiotherapy treatment, either immediately after surgery or delayed to clinical or radiological progression, has been a historically controversial issue due to concerns about possible acute and long-term side effects that may affect the quality of life of patients. The risk of cognitive impairment associated with early versus late radiotherapy for the treatment of LGG is not clear, and neurocognitive evaluation should be an integral part of the long-term follow-up of these patients to improve the evidence in this regard<a class="elsevierStyleCrossRef" href="#bib0355"><span class="elsevierStyleSup">71</span></a>. The optimal time to administer additional therapy remains uncertain<a class="elsevierStyleCrossRefs" href="#bib0360"><span class="elsevierStyleSup">72,73</span></a>, and the decision must be made on an individual basis. In this sense, attempts have been made to identify risk groups in which the benefit of early radiotherapy would not only be in delaying recurrence, but also in increasing overall survival (high-risk patients). Thus, to the prognostic factors established by Pignatti et al. (age, astrocytic histology, tumor size, neurological deficits, uni- or bilaterality), new genetic-molecular aspects are added that include, among others, IDH mutation, ATRX or 1p/19q codeletion as factors of good prognosis, classifying patients as "low and high risk". Factors to consider when selecting high-risk patients for post-immediate therapy include: age >40 years, incomplete resection and unfavourable molecular characteristics<a class="elsevierStyleCrossRefs" href="#bib0130"><span class="elsevierStyleSup">26,74</span></a>. In low-risk patients (age <40 years with complete resection and favourable molecular characteristics), follow-up could be performed by delaying additional therapy at the time of progression. The more unfavourable the molecular or risk factors are, the more we will be inclined towards immediate radiotherapy<a class="elsevierStyleCrossRefs" href="#bib0135"><span class="elsevierStyleSup">27,33</span></a>.</p><p id="par0265" class="elsevierStylePara elsevierViewall">Modern, highly conformal radiation techniques, including intensity-modulated radiotherapy for newly diagnosed tumors and radiosurgery for recurrent tumors, could provide superior target coverage while sparing non-malignant brain tissue. Radiotherapy with protons or heavy ions may be options to consider for patients with tumors close to brain regions at risk, or in those with a favourable prognosis, in order to avoid late toxicities. However, more clinical trials are required to determine the tolerability, safety and efficacy of these approaches compared to standard radiotherapy<a class="elsevierStyleCrossRefs" href="#bib0375"><span class="elsevierStyleSup">75,76</span></a>.</p></span><span id="sec0045" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0065">Chemotherapy: evolution in management over the last two decades</span><p id="par0270" class="elsevierStylePara elsevierViewall">Chemotherapy (CT) treatment in the last two decades has changed considerably. Although until the end of the last century its use in LGGs was anecdotal, in an attempt to delay radiotherapy (RT) in children<a class="elsevierStyleCrossRef" href="#bib0385"><span class="elsevierStyleSup">77</span></a>, or in the progression of optic nerve gliomas<a class="elsevierStyleCrossRef" href="#bib0390"><span class="elsevierStyleSup">78</span></a>, during the years from 2000 to 2015 CT began to be used empirically, given the evidence that surgery alone left us with many unresolved patients<a class="elsevierStyleCrossRef" href="#bib0195"><span class="elsevierStyleSup">39</span></a>, and in many series during that period the percentage of patients treated with various CT regimens rose to 10−15%.</p><p id="par0275" class="elsevierStylePara elsevierViewall">It was not until the publication of both the new WHO classification in 2016<a class="elsevierStyleCrossRef" href="#bib0060"><span class="elsevierStyleSup">12</span></a> and the study by Buckner et al.<a class="elsevierStyleCrossRef" href="#bib0285"><span class="elsevierStyleSup">57</span></a> that the use of CT in LGGs began to spread. It was possible to demonstrate that diffuse grade II gliomas can be subdivided into groups with different prognoses, based on the presence of molecular alterations, which mainly include IDH mutations and 1p/19q codeletion (LOH)<a class="elsevierStyleCrossRef" href="#bib0300"><span class="elsevierStyleSup">60</span></a>.</p><p id="par0280" class="elsevierStylePara elsevierViewall">By then, Pignatti et al.<a class="elsevierStyleCrossRef" href="#bib0370"><span class="elsevierStyleSup">74</span></a> had categorised patients into "low and high risk", based on five factors (age, astrocytoma histology, neurological deficits, tumor diameter, and uni- or bilaterality), in a manner that those who had a score of 0–2 had a longer survival time (7.8 years) than those who scored 3–5 (3.67 years). However, the new genetic-molecular findings that reclassify LGGs make it necessary to consider a new prognostic grading, so that age <40 years and complete surgical resection mean these patients are classified as "low risk", whereas those who do not meet one of these factors are "high risk". Together with these, 1p/19q LOH and the presence of mutated IDH imply a better prognosis, but in patients classified as high risk we must always consider carrying out complementary treatments<a class="elsevierStyleCrossRef" href="#bib0395"><span class="elsevierStyleSup">79</span></a>. Other second-line molecular factors that we can point to, and that also imply a prognostic value, are the state of the TERT promoter, ATRX and EGFR amplification.</p><p id="par0285" class="elsevierStylePara elsevierViewall">In this way, we could simplify the complementary therapeutic management of patients with LGG after surgery<a class="elsevierStyleCrossRefs" href="#bib0290"><span class="elsevierStyleSup">58,80</span></a>:<ul class="elsevierStyleList" id="lis0020"><li class="elsevierStyleListItem" id="lsti0065"><span class="elsevierStyleLabel">a)</span><p id="par0290" class="elsevierStylePara elsevierViewall"><span class="elsevierStyleItalic">Grade II oligodendroglioma</span> (1p/19q LOH) and grade II astrocytoma with mutated IDH:<ul class="elsevierStyleList" id="lis0025"><li class="elsevierStyleListItem" id="lsti0070"><span class="elsevierStyleLabel">-</span><p id="par0295" class="elsevierStylePara elsevierViewall">Low risk = follow up.</p></li><li class="elsevierStyleListItem" id="lsti0075"><span class="elsevierStyleLabel">-</span><p id="par0300" class="elsevierStylePara elsevierViewall">High risk = RT + PCV (procarbazine, lomustine [CCNU] and vincristine).</p></li></ul></p></li><li class="elsevierStyleListItem" id="lsti0080"><span class="elsevierStyleLabel">b)</span><p id="par0305" class="elsevierStylePara elsevierViewall"><span class="elsevierStyleItalic">Grade II astrocytoma with IDH-wildtype</span> (IDH-WT): <ul class="elsevierStyleList" id="lis0030"><li class="elsevierStyleListItem" id="lsti0085"><span class="elsevierStyleLabel">-</span><p id="par0310" class="elsevierStylePara elsevierViewall">Favourable molecular and risk factors = a subgroup of patients may be included for treatment with RT + PCV.</p></li><li class="elsevierStyleListItem" id="lsti0090"><span class="elsevierStyleLabel">-</span><p id="par0315" class="elsevierStylePara elsevierViewall">Unfavourable molecular and risk factors = they will be treated as glioblastoma: Stupp protocol: RT + TMZ (temozolamide).</p></li></ul></p></li><li class="elsevierStyleListItem" id="lsti0095"><span class="elsevierStyleLabel">c)</span><p id="par0320" class="elsevierStylePara elsevierViewall"><span class="elsevierStyleItalic">Tumors of uncertain nature</span>; for example, presence of 1p/19q LOH, but with IDH-WT, individualise the best CT treatment for each patient. Remember that elderly patients or patients with neurological deficits tolerate CT with PCV poorly.</p></li></ul></p><p id="par0325" class="elsevierStylePara elsevierViewall">It should be noted that, while new studies do not update it (RTGO 9802)<a class="elsevierStyleCrossRef" href="#bib0405"><span class="elsevierStyleSup">81</span></a>, we must individualise the best possible treatment for each patient, starting from discussion in the neuro-oncology committees of each centre and taking into account other risk factors: tumor size/volume, bilaterality and the existence or not of neurological deficit<a class="elsevierStyleCrossRef" href="#bib0410"><span class="elsevierStyleSup">82</span></a>.</p></span></span><span id="sec0050" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0070">Second line of treatments</span><span id="sec0055" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0075">Surgery after recurrence: indications</span><p id="par0330" class="elsevierStylePara elsevierViewall">Approximately half of the patients diagnosed and treated for an LGG will present a recurrence at five years of follow-up<a class="elsevierStyleCrossRef" href="#bib0415"><span class="elsevierStyleSup">83</span></a>. Due to this high recurrence rate and the risk of malignant transformation of these lesions, adequate follow-up after a first line of treatment is essential.</p><p id="par0335" class="elsevierStylePara elsevierViewall">Surgery is considered the first option in case of recurrence, since it helps to improve those symptoms derived from the lesion, provides tissue for analysis, and can improve both PFS and OS, especially if a complete resection of the lesion is achieved, without causing new neurological deficits<a class="elsevierStyleCrossRef" href="#bib0420"><span class="elsevierStyleSup">84</span></a>. As in the first line of treatment, the literature offers the best results in resections that exceed 80–90%, or with remnants smaller than 10−15 cm<span class="elsevierStyleSup">3</span> in volume<a class="elsevierStyleCrossRefs" href="#bib0200"><span class="elsevierStyleSup">40,85</span></a>. In the case of not having a pattern of resectable recurrence, a biopsy should be considered to rule out post-treatment changes or change in tumor grade, which would suggest a change in the treatment plan for the patient.</p><p id="par0340" class="elsevierStylePara elsevierViewall">The timing of surgical indication depends on the type of recurrence, which can be clinical and/or radiological. A worsening in the control of epileptic seizures can give us the first evidence of recurrence of an LGG. Surgery has proven to have an impact on tumor-related epilepsy, with the most extensive resections being those that achieve better seizure control<a class="elsevierStyleCrossRef" href="#bib0220"><span class="elsevierStyleSup">44</span></a>.</p><p id="par0345" class="elsevierStylePara elsevierViewall">There are two possible radiological scenarios that make us suspect a tumor recurrence, and therefore propose a reintervention. The first is the suspicion of a change of grade<a class="elsevierStyleCrossRef" href="#bib0430"><span class="elsevierStyleSup">86</span></a>. The second is a progressive increase in tumor volume in the absence of signs that suggest malignancy. In this second case, the moment of surgical indication is more delicate, since the increase is frequently not accompanied by a clear clinical progression. Taking objective radiological quantitative measurements, such as tumor growth rate<a class="elsevierStyleCrossRef" href="#bib0435"><span class="elsevierStyleSup">87</span></a>, turns out to be more accurate than the follow-up radiological report, since the simple visual comparison can result in a delay in the indication of treatment<a class="elsevierStyleCrossRef" href="#bib0440"><span class="elsevierStyleSup">88</span></a>.</p><p id="par0350" class="elsevierStylePara elsevierViewall">In conclusion, it is essential to ensure the timely indication of treatment for tumor recurrence in LGG, identifying those patients with a high risk of tumor recurrence or progression, based on clinical criteria (age and neurological symptoms, including epileptic seizures), radiological criteria (tumor growth rate or suspected change in grade), histological criteria (astrocytic lineage or risk subtypes) and finally molecular criteria (IDH mutation, MGMT methylation or 1p-19q codeletion).</p></span><span id="sec0060" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0080">Radiotherapy in recurrences: indications</span><p id="par0355" class="elsevierStylePara elsevierViewall">The benefits of radiotherapy in the case of recurrent LGGs must be carefully weighed against possible secondary adverse effects<a class="elsevierStyleCrossRefs" href="#bib0285"><span class="elsevierStyleSup">57,89</span></a> (radionecrosis, leukoencephalopathy, cognitive alterations, radiation-induced neoplasms, etc.).</p><p id="par0360" class="elsevierStylePara elsevierViewall">In cases of recurrence, we can divide patients into two groups<a class="elsevierStyleCrossRef" href="#bib0395"><span class="elsevierStyleSup">79</span></a>: those who have received prior radiotherapy and those who have not.<ul class="elsevierStyleList" id="lis0035"><li class="elsevierStyleListItem" id="lsti0100"><span class="elsevierStyleLabel">a)</span><p id="par0365" class="elsevierStylePara elsevierViewall"><span class="elsevierStyleItalic">Patients without previous radiotherapy:</span> in these cases, the RTOG 9802<a class="elsevierStyleCrossRef" href="#bib0290"><span class="elsevierStyleSup">58</span></a> study supports the use of radiotherapy and PCV in patients who have not received previous complementary treatment, in the same way as it does in newly diagnosed patients.</p></li><li class="elsevierStyleListItem" id="lsti0105"><span class="elsevierStyleLabel">b)</span><p id="par0370" class="elsevierStylePara elsevierViewall">Patients who have received previous radiotherapy: <span class="elsevierStyleItalic">re-irradiation may be considered in these patients with highly focused radiotherapy techniques in cases of small and geometrically favourable recurrence, as well as when the recurrence occurs outside the field of previous irradiation.</span></p></li></ul></p><p id="par0375" class="elsevierStylePara elsevierViewall">Within the radiotherapy techniques that can be used in patients with previous irradiation, radiosurgery techniques can be considered. Due to the infiltrative nature of LGGs, the role of radiosurgery in these patients is difficult to justify and the scientific evidence in this regard is low. But there are non-comparative studies that have shown that they are safe and effective techniques in the treatment of LGG with results in OS and disease-free period comparable to conventional techniques<a class="elsevierStyleCrossRefs" href="#bib0450"><span class="elsevierStyleSup">90,91</span></a>.</p><p id="par0380" class="elsevierStylePara elsevierViewall">The proton therapy techniques developed in recent years have the potential to preserve crucial neurological structures while maintaining adequate radiation doses in the area to be irradiated. The benefits in LGG are unknown, and there are very few studies in this regard in adults<a class="elsevierStyleCrossRefs" href="#bib0460"><span class="elsevierStyleSup">92,93</span></a>. The only study that analyses the long-term effects of proton therapy in the treatment of LGG shows survival rates and disease-free period at five years comparable to those achieved with conventional radiotherapy techniques<a class="elsevierStyleCrossRef" href="#bib0470"><span class="elsevierStyleSup">94</span></a>. Other studies have shown the absence of changes in the cognitive<a class="elsevierStyleCrossRef" href="#bib0475"><span class="elsevierStyleSup">95</span></a> or neuroendocrine<a class="elsevierStyleCrossRef" href="#bib0480"><span class="elsevierStyleSup">96</span></a> sphere.</p></span><span id="sec0065" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0085">Chemotherapy in recurrences</span><p id="par0385" class="elsevierStylePara elsevierViewall">In second-line treatment based on molecular markers, the National Comprehensive Cancer Network guidelines recommend modifying treatment based on that used in the first line: thus, patients treated with PCV switch to temozolamide, and vice versa. Those patients with IDH-WT would be considered as high grade and would be included in the Stupp protocol. In these patients, the determination of the MGMT gene methylation status would have prognostic value for the response to treatment<a class="elsevierStyleCrossRefs" href="#bib0135"><span class="elsevierStyleSup">27,79</span></a>.</p><p id="par0390" class="elsevierStylePara elsevierViewall">Of note is the introduction in the guidelines of the treatment possibilities in those patients in whom the tumor presents mutation of the BRAF V600E gene. This can occur in tumors such as pilocytic astrocytoma, ganglioglioma and pleomorphic xanthoastrocytoma. In these cases, treatment with inhibitors of the BRAF/MEK pathway would be indicated, so determination of this mutation is also important in cases of IDH-WT to ascertain if this therapeutic possibility exists. In this sense, studies such as VE-BASKET, or the one published by Brown et al. in 2017, offer guidance in these therapeutic possibilities<a class="elsevierStyleCrossRefs" href="#bib0485"><span class="elsevierStyleSup">97,98</span></a>.</p><p id="par0395" class="elsevierStylePara elsevierViewall">The guidelines also point out that in cases where there may be a mutation in mTOR in the context of tuberous sclerosis complex, inhibitors of this pathway, such as everolimus, can offer targeted treatment. The randomised EXIST study published acceptable results with good tolerance to treatment<a class="elsevierStyleCrossRef" href="#bib0495"><span class="elsevierStyleSup">99</span></a>.</p><p id="par0400" class="elsevierStylePara elsevierViewall">It is foreseeable that in the future more precise molecular determinations will be achieved in more patients and that therapeutic targets and specific treatments will be developed.</p></span><span id="sec0070" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0090">Low-grade glioma in the elderly: radiological interpretation and treatment</span><p id="par0405" class="elsevierStylePara elsevierViewall">Advanced age is a widely recognised poor prognostic factor in glial tumors. This population group has been extensively studied in high-grade gliomas, while in low-grade tumors there is a lack of consensus.</p><p id="par0410" class="elsevierStylePara elsevierViewall">LGGs are mostly diagnosed between the third and fourth decades of life, and only 10–18% of these tumors are diagnosed in people over 60 years of age<a class="elsevierStyleCrossRef" href="#bib0500"><span class="elsevierStyleSup">100</span></a>.</p><p id="par0415" class="elsevierStylePara elsevierViewall">The clinical manifestations in this group are usually characterised by a lower incidence of seizures and a higher frequency of focal deficit, which usually implies worse scores on the KPS scale, but also an earlier diagnosis<a class="elsevierStyleCrossRef" href="#bib0505"><span class="elsevierStyleSup">101</span></a>. On the other hand, advanced age increases the existence of comorbidities and the vulnerability of patients.</p><p id="par0420" class="elsevierStylePara elsevierViewall">From the radiological point of view, they are tumors with a larger size on NMR, greater contrast uptake and bihemispheric involvement<a class="elsevierStyleCrossRef" href="#bib0505"><span class="elsevierStyleSup">101</span></a>. Regarding their genetic characteristics, a higher frequency of IDH-WT and TERT<a class="elsevierStyleCrossRef" href="#bib0500"><span class="elsevierStyleSup">100</span></a> mutation stand out.</p><p id="par0425" class="elsevierStylePara elsevierViewall">Traditionally, treatment has tended towards more conservative resections and greater adjuvant chemotherapy<a class="elsevierStyleCrossRef" href="#bib0510"><span class="elsevierStyleSup">102</span></a>. In contrast, several studies have shown similar rates of complications in young people, so a gross total resection (GTR) with criteria similar to high-grade gliomas should be aimed for<a class="elsevierStyleCrossRef" href="#bib0515"><span class="elsevierStyleSup">103</span></a>.</p><p id="par0430" class="elsevierStylePara elsevierViewall">Adjuvant therapy in these patients consists of radiotherapy and temozolamide in cases of IDH wildtype/without 1p/19q codeletion or PCV (mutated IDH/1p/19q codeletion), although given the toxicity of PCV and the greater frailty of patients, this latter option must be individualised, with temozolamide being more commonly used<a class="elsevierStyleCrossRef" href="#bib0520"><span class="elsevierStyleSup">104</span></a>.</p><p id="par0435" class="elsevierStylePara elsevierViewall">Age over 50 years in LGG is associated with worse OS and PFS, without a significant improvement in these being achieved in recent years, probably due to their more conservative management from the surgical point of view<a class="elsevierStyleCrossRef" href="#bib0525"><span class="elsevierStyleSup">105</span></a>.</p><p id="par0440" class="elsevierStylePara elsevierViewall">Therefore, it is recommended to make an effort to achieve the maximum possible resection in this age group, followed by adjuvant treatment, mainly with temozolamide and radiotherapy.</p></span></span><span id="sec0075" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0095">New treatments</span><span id="sec0080" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0100">Innovation in surgery</span><p id="par0445" class="elsevierStylePara elsevierViewall">Surgery is the oldest form of LGG treatment and also the one that has shown the most benefit to date.</p><p id="par0450" class="elsevierStylePara elsevierViewall">Surgery today is very different from that of 100 years ago, with improvements being made based on a multitude of small innovations.</p><p id="par0455" class="elsevierStylePara elsevierViewall">The objectives of surgery have always been the same: a diagnosis with analysis of the tissue and the maximum removal of tumor tissue, with the minimum risk of neurological deficit and the least discomfort.</p><p id="par0460" class="elsevierStylePara elsevierViewall">Despite the advances, these objectives are not fully achieved. The most recent advances have allowed improvements in:</p><p id="par0465" class="elsevierStylePara elsevierViewall">Preoperative planning with images with better resolution, in all planes, in 3D, and with the possibility of including multimodal information. In addition to the structural information, we can add more exact information on the metabolism of the tumor with amino-acid PET and perfusion MRI, and on brain function in the areas adjacent to the tumor with functional MRI and tractography. As well as for planning, all this information can be used as a guide during the resection itself, in the most advanced navigation systems.</p><p id="par0470" class="elsevierStylePara elsevierViewall">The resection assistance can be completed with better possibilities of intraoperative imaging, MRI, (increasingly advanced) ultrasound or CT. These techniques are not yet widely available, but they are becoming more widespread.</p><p id="par0475" class="elsevierStylePara elsevierViewall">As technical possibilities that have not yet been incorporated into routine practice but are already in clinical trial phases, there are various imaging systems with resolution at the cellular level, which have shown similar results to intraoperative biopsy<a class="elsevierStyleCrossRef" href="#bib0530"><span class="elsevierStyleSup">106</span></a>, including various confocal microscopy systems and optical coherence tomography (OCT).</p><p id="par0480" class="elsevierStylePara elsevierViewall">Among the techniques that may be applied in the coming years, but have yet to prove their effectiveness, there are other ways of removing tumor tissue that can be applied less invasively. They include LITT, or laser thermal ablation, and focused ultrasound. The former has already been used in small, deep tumors<a class="elsevierStyleCrossRef" href="#bib0535"><span class="elsevierStyleSup">107</span></a>; the latter has shown efficacy for making very small lesions in functional neurosurgery, although still has technical limitations that prevent its use in tumors.</p><p id="par0485" class="elsevierStylePara elsevierViewall">From the point of view of adjusting the removal limit, in recent years there has been enormous advances in the use of neurophysiological monitoring. Much progress has been made both in the number of centres capable of using it and in the sophistication of the functions that can be monitored<a class="elsevierStyleCrossRef" href="#bib0540"><span class="elsevierStyleSup">108</span></a>.</p><p id="par0490" class="elsevierStylePara elsevierViewall">All these advances that are introduced in surgery encounter the problem of there being little evidence of the benefits of their use. It is impossible to answer the innumerable questions that are generated with randomised clinical trials. That is why it is very interesting to see the push that has been given by the NIH (National Institute of Health)<a class="elsevierStyleCrossRef" href="#bib0545"><span class="elsevierStyleSup">109</span></a> to the concept of developing a "science of practice", in which enormous amounts of data on surgery are collected that can be analysed with sophisticated computer tools to answer many of these questions more quickly.</p></span><span id="sec0085" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0105">Integration of anatomy and neurological function for the planning of surgery for low-grade tumors in eloquent areas</span><p id="par0495" class="elsevierStylePara elsevierViewall">Making 3D tractography models of the relationship with tumor lesions seems to be low cost and relevantly useful for neurosurgeon training, intervention planning and doctor-patient communication<a class="elsevierStyleCrossRef" href="#bib0550"><span class="elsevierStyleSup">110</span></a>.</p><p id="par0500" class="elsevierStylePara elsevierViewall">Studies have also been carried out with 3D models with hybridisation of CT and MR images for planning lesion surgery involving bone elements, which adds greater precision when segmenting these structures and thus creates models with greater anatomical precision, which supports translational research in this area<a class="elsevierStyleCrossRef" href="#bib0555"><span class="elsevierStyleSup">111</span></a>.</p><p id="par0505" class="elsevierStylePara elsevierViewall">Lastly, progress has been made in the creation of 3D models that integrate the anatomy and function of cortical and subcortical structures for use in complex LGG cases. These models have been useful both in their practical application when planning the intervention, in doctor-patient communication and in the training of neurosurgeons in this type of complex surgery, serving as an aid to the techniques that are essential today to face this type of intervention: anatomical knowledge, intraoperative imaging (ultrasound, CT, MRI), neuronavigation, neurophysiological monitoring, mapping, awake patient, etc.<a class="elsevierStyleCrossRef" href="#bib0560"><span class="elsevierStyleSup">112</span></a>.</p></span><span id="sec0090" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0110">Brain monitoring/mapping in awake patients in surgery for low-grade gliomas of the non-dominant hemisphere (NDH)</span><p id="par0510" class="elsevierStylePara elsevierViewall">Neurophysiological monitoring is a basic tool in LGG surgery. Although brain mapping with cortico-subcortical stimulation in an awake patient (BM in AP) has been used preferentially in LGG surgery on the dominant hemisphere (DH), there is growing evidence that it may be useful in LGG surgery on the NDH<a class="elsevierStyleCrossRef" href="#bib0565"><span class="elsevierStyleSup">113</span></a>, to the point of relativising the classical concepts of dominance and eloquence<a class="elsevierStyleCrossRef" href="#bib0570"><span class="elsevierStyleSup">114</span></a>.</p><p id="par0515" class="elsevierStylePara elsevierViewall">The absence of systematic pre- and postoperative cognitive and metacognitive assessments in operated patients may lead to an underestimation of deficits in these areas<a class="elsevierStyleCrossRef" href="#bib0575"><span class="elsevierStyleSup">115</span></a>.</p><p id="par0520" class="elsevierStylePara elsevierViewall">During BM in AP of the NDH, linguistic alterations are found in frontal cortical stimulation with the appearance of dysarthria in the ventral premotor cortex, anomia in the dorsal premotor cortex, and semantic paraphasias in the dorsolateral prefrontal cortex. Phonetic paraphasias can be seen during parietal cortical stimulation, and anomia and semantic paraphasias can be seen during temporal cortical stimulation. For its part, subcortical stimulation of the superior longitudinal fasciculus and the arcuate fasciculus triggers phonetic paraphasias, that of the inferior fronto-occipital fasciculus triggers semantic paraphasias, that of the aslant tract triggers perseverations, and that of the frontostriatal tract triggers dysarthria.</p><p id="par0525" class="elsevierStylePara elsevierViewall">Possible explanations for these phenomena include stimulation in unknowingly ambidextrous and atypical right-handed patients. In cases in which transient intraoperative aphasia is observed after stimulation, it may be related to the organisation of cortico-subcortical language networks in the NDH that would constitute a mirror configuration with respect to the dominant hemisphere.</p><p id="par0530" class="elsevierStylePara elsevierViewall">The literature details IOP monitoring in the NDH of cognitive functions such as nonverbal semantics in the superior temporal gyrus, pars triangularis, dorsolateral prefrontal cortex and inferior fronto-occipital fasciculus<a class="elsevierStyleCrossRef" href="#bib0580"><span class="elsevierStyleSup">116</span></a>, and working memory in the right angular gyrus. Alterations in metacognitive functions have been described, such as the recognition of emotions/empathy<a class="elsevierStyleCrossRef" href="#bib0585"><span class="elsevierStyleSup">117</span></a> in the right arcuate and superior longitudinal fasciculus, and the attribution of intention to others in the right cingulum.</p><p id="par0535" class="elsevierStylePara elsevierViewall">The different experiences point to obtaining larger resections and better clinical results in terms of quality of life and return to work, when cognitive and metacognitive functions are monitored and considered at the time of resection.</p><p id="par0540" class="elsevierStylePara elsevierViewall">In conclusion, monitoring with BM in AP in LGG surgery on the NDH is a very useful tool in terms of increasing the degree of resection and decreasing neuropsychological alterations after surgery. In order to verify these results, a neuropsychological examination should be carried out in a more systematic way before and after surgery on the NDH.</p></span></span><span id="sec0095" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0115">Conclusions</span><p id="par0545" class="elsevierStylePara elsevierViewall">The management and treatment of LGG includes a wide range of possibilities depending on the characteristics of the tumor. The neurosurgeon plays a leading role in this pathology, therefore it is important to have a deep understanding of the advantages and disadvantages of each of the options, as well as each patient's situation, in order to be able to adapt them in an individualised way.</p></span><span id="sec0100" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0120">Funding</span><p id="par0550" class="elsevierStylePara elsevierViewall">This study has received no specific funding from public, private or non-profit organisations.</p></span><span id="sec0105" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0125">Conflicts of interest</span><p id="par0555" class="elsevierStylePara elsevierViewall">The authors declare that they have no conflicts of interest.</p></span></span>"
"textoCompletoSecciones" => array:1 [
"secciones" => array:12 [
0 => array:3 [
"identificador" => "xres1891801"
"titulo" => "Abstract"
"secciones" => array:1 [
0 => array:1 [
"identificador" => "abst0005"
]
]
]
1 => array:2 [
"identificador" => "xpalclavsec1637072"
"titulo" => "Keywords"
]
2 => array:3 [
"identificador" => "xres1891802"
"titulo" => "Resumen"
"secciones" => array:1 [
0 => array:1 [
"identificador" => "abst0010"
]
]
]
3 => array:2 [
"identificador" => "xpalclavsec1637071"
"titulo" => "Palabras clave"
]
4 => array:2 [
"identificador" => "sec0005"
"titulo" => "Introduction"
]
5 => array:3 [
"identificador" => "sec0010"
"titulo" => "Initial management of low-grade gliomas"
"secciones" => array:6 [
0 => array:2 [
"identificador" => "sec0015"
"titulo" => "Diagnosis and treatment of asymptomatic lesions suggestive of low-grade glioma"
]
1 => array:3 [
"identificador" => "sec0020"
"titulo" => "Histological and molecular classification of low-grade gliomas"
"secciones" => array:1 [
0 => array:2 [
"identificador" => "sec0025"
"titulo" => "Grades of recommendation"
]
]
]
2 => array:2 [
"identificador" => "sec0030"
"titulo" => "Low-grade glioma (LGG) surgery"
]
3 => array:2 [
"identificador" => "sec0035"
"titulo" => "Differential role of surgery for low-grade gliomas based on their molecular profile"
]
4 => array:2 [
"identificador" => "sec0040"
"titulo" => "Radiotherapy in low-grade gliomas"
]
5 => array:2 [
"identificador" => "sec0045"
"titulo" => "Chemotherapy: evolution in management over the last two decades"
]
]
]
6 => array:3 [
"identificador" => "sec0050"
"titulo" => "Second line of treatments"
"secciones" => array:4 [
0 => array:2 [
"identificador" => "sec0055"
"titulo" => "Surgery after recurrence: indications"
]
1 => array:2 [
"identificador" => "sec0060"
"titulo" => "Radiotherapy in recurrences: indications"
]
2 => array:2 [
"identificador" => "sec0065"
"titulo" => "Chemotherapy in recurrences"
]
3 => array:2 [
"identificador" => "sec0070"
"titulo" => "Low-grade glioma in the elderly: radiological interpretation and treatment"
]
]
]
7 => array:3 [
"identificador" => "sec0075"
"titulo" => "New treatments"
"secciones" => array:3 [
0 => array:2 [
"identificador" => "sec0080"
"titulo" => "Innovation in surgery"
]
1 => array:2 [
"identificador" => "sec0085"
"titulo" => "Integration of anatomy and neurological function for the planning of surgery for low-grade tumors in eloquent areas"
]
2 => array:2 [
"identificador" => "sec0090"
"titulo" => "Brain monitoring/mapping in awake patients in surgery for low-grade gliomas of the non-dominant hemisphere (NDH)"
]
]
]
8 => array:2 [
"identificador" => "sec0095"
"titulo" => "Conclusions"
]
9 => array:2 [
"identificador" => "sec0100"
"titulo" => "Funding"
]
10 => array:2 [
"identificador" => "sec0105"
"titulo" => "Conflicts of interest"
]
11 => array:1 [
"titulo" => "References"
]
]
]
"pdfFichero" => "main.pdf"
"tienePdf" => true
"fechaRecibido" => "2022-03-09"
"fechaAceptado" => "2022-08-01"
"PalabrasClave" => array:2 [
"en" => array:1 [
0 => array:4 [
"clase" => "keyword"
"titulo" => "Keywords"
"identificador" => "xpalclavsec1637072"
"palabras" => array:4 [
0 => "Low grade glioma"
1 => "Consensus"
2 => "Treatment guideline"
3 => "Surgery brain tumor"
]
]
]
"es" => array:1 [
0 => array:4 [
"clase" => "keyword"
"titulo" => "Palabras clave"
"identificador" => "xpalclavsec1637071"
"palabras" => array:4 [
0 => "Gliomas bajo grado"
1 => "Consenso"
2 => "Guía tratamiento"
3 => "Cirugía tumor cerebral"
]
]
]
]
"tieneResumen" => true
"resumen" => array:2 [
"en" => array:2 [
"titulo" => "Abstract"
"resumen" => "<span id="abst0005" class="elsevierStyleSection elsevierViewall"><p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Adult low-grade gliomas (Low Grade Gliomas, LGG) are tumors that originate from the glial cells of the brain and whose management involves great controversy, starting from the diagnosis, to the treatment and subsequent follow-up. For this reason, the Tumor Group of the Spanish Society of Neurosurgery (GT-SENEC) has held a consensus meeting, in which the most relevant neurosurgical issues have been discussed, reaching recommendations based on the best scientific evidence. In order to obtain the maximum benefit from these treatments, an individualised assessment of each patient should be made by a multidisciplinary team.</p><p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">Experts in each LGG treatment field have briefly described it based in their experience and the reviewed of the literature.</p><p id="spar0025" class="elsevierStyleSimplePara elsevierViewall">Each area has been summarized and focused on the best published evidence.</p><p id="spar0030" class="elsevierStyleSimplePara elsevierViewall">LGG have been surrounded by treatment controversy, although during the last years more accurate data has been published in order to reach treatment consensus. Neurosurgeons must know treatment options, indications and risks to participate actively in the decision making and to offer the best surgical treatment in every case.</p></span>"
]
"es" => array:2 [
"titulo" => "Resumen"
"resumen" => "<span id="abst0010" class="elsevierStyleSection elsevierViewall"><p id="spar0035" class="elsevierStyleSimplePara elsevierViewall">Los gliomas de bajo grado (<span class="elsevierStyleItalic">Low Grade Gliomas</span>, LGG) del adulto son tumores que se originan a partir de las células gliales del cerebro y cuyo manejo implica gran controversia a día de hoy, comenzando desde el diagnóstico, hasta el tratamiento y seguimiento posterior de estos pacientes. Es por ello que el grupo de tumores de la Sociedad Española de Neurocirugía (GT-SENEC) ha llevado a cabo una reunión de consenso, en la que se han debatido las cuestiones neuroquirúrgicas más relevantes, llegando a recomendaciones basadas en la mejor evidencia científica. Con el fin de obtener el máximo beneficio a estos tratamientos se debe hacer una valoración individualizada de cada paciente por un equipo multidisciplinar, constituido por aquellas especialidades involucradas tanto en el diagnóstico como en el tratamiento.</p><p id="spar0040" class="elsevierStyleSimplePara elsevierViewall">El objetivo de este trabajo es elaborar unas recomendaciones de tratamiento para los pacientes con LGG, para lo cual un experto en cada campo ha descrito lo más relevante de dicha área basado tanto en su experiencia, como en la literatura.</p><p id="spar0045" class="elsevierStyleSimplePara elsevierViewall">Se han desarrollado los apartados más relevantes en el manejo de los LGG basados en la mejor evidencia publicada.</p><p id="spar0050" class="elsevierStyleSimplePara elsevierViewall">A pesar de que existe controversia en algunos aspectos del manejo de los LGG, cada vez hay más datos para poder hacer recomendaciones de tratamiento consensuadas. El neurocirujano debe conocer las distintas opciones de tratamientos, sus indicaciones y riesgos para poder participar activamente en la toma de decisiones y poder ofrecer un tratamiento neuroquirúrgico oportuno a cada situación.</p></span>"
]
]
"multimedia" => array:2 [
0 => array:8 [
"identificador" => "fig0005"
"etiqueta" => "Figure 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 2274
"Ancho" => 2508
"Tamanyo" => 274492
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0005"
"detalle" => "Figure "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Algorithm in asymptomatic lesions suggestive of low-grade gliomas.</p>"
]
]
1 => array:8 [
"identificador" => "fig0010"
"etiqueta" => "Figure 2"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr2.jpeg"
"Alto" => 2285
"Ancho" => 2508
"Tamanyo" => 307581
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0010"
"detalle" => "Figure "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">Algorithm in recurrence of low-grade gliomas.</p>"
]
]
]
"bibliografia" => array:2 [
"titulo" => "References"
"seccion" => array:1 [
0 => array:2 [
"identificador" => "bibs0005"
"bibliografiaReferencia" => array:117 [
0 => array:3 [
"identificador" => "bib0005"
"etiqueta" => "1"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Incidental findings in magnetic resonance imaging of the brains of healthy young men"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.jns.2005.09.008"
"Revista" => array:6 [
"tituloSerie" => "J Neurol Sci"
"fecha" => "2006"
"volumen" => "240"
"paginaInicial" => "81"
"paginaFinal" => "84"
"link" => array:1 [ …1]
]
]
]
]
]
]
1 => array:3 [
"identificador" => "bib0010"
"etiqueta" => "2"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Incidental findings on brain imaging in the general pediatric population"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1056/NEJMc1710724"
"Revista" => array:6 [
"tituloSerie" => "N Engl J Med"
"fecha" => "2017"
"volumen" => "377"
"paginaInicial" => "1593"
"paginaFinal" => "1595"
"link" => array:1 [ …1]
]
]
]
]
]
]
2 => array:3 [
"identificador" => "bib0015"
"etiqueta" => "3"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Incidental diffuse low-grade gliomas: from early detection to preventive neuro-oncological surgery"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s10143-015-0675-6"
"Revista" => array:6 [
"tituloSerie" => "Neurosurg Rev"
"fecha" => "2016"
"volumen" => "39"
"paginaInicial" => "377"
"paginaFinal" => "384"
"link" => array:1 [ …1]
]
]
]
]
]
]
3 => array:3 [
"identificador" => "bib0020"
"etiqueta" => "4"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Natural history and surgical management of incidentally discovered low-grade gliomas"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/2011.9.JNS111068"
"Revista" => array:6 [
"tituloSerie" => "J Neurosurg"
"fecha" => "2012"
"volumen" => "116"
"paginaInicial" => "365"
"paginaFinal" => "372"
"link" => array:1 [ …1]
]
]
]
]
]
]
4 => array:3 [
"identificador" => "bib0025"
"etiqueta" => "5"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Natural history of incidental World Health Organization grade II gliomas"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1002/ana.22106"
"Revista" => array:6 [
"tituloSerie" => "Ann Neurol"
"fecha" => "2010"
"volumen" => "68"
"paginaInicial" => "727"
"paginaFinal" => "733"
"link" => array:1 [ …1]
]
]
]
]
]
]
5 => array:3 [
"identificador" => "bib0030"
"etiqueta" => "6"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Does early resection of presumed low-grade glioma improve survival? A clinical perspective"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-017-2418-8"
"Revista" => array:6 [
"tituloSerie" => "J Neurooncol"
"fecha" => "2017"
"volumen" => "133"
"paginaInicial" => "137"
"paginaFinal" => "146"
"link" => array:1 [ …1]
]
]
]
]
]
]
6 => array:3 [
"identificador" => "bib0035"
"etiqueta" => "7"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "The rationale to perform early resection in incidental diffuse low-grade glioma: toward a ‘preventive surgical neurooncology’"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.wneu.2012.06.036"
"Revista" => array:6 [
"tituloSerie" => "World Neurosurg"
"fecha" => "2013"
"volumen" => "80"
"paginaInicial" => "e115"
"paginaFinal" => "7"
"link" => array:1 [ …1]
]
]
]
]
]
]
7 => array:3 [
"identificador" => "bib0040"
"etiqueta" => "8"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "The silent phase of diffuse low-grade gliomas. Is it when we missed the action?"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s00701-013-1886-7"
"Revista" => array:6 [
"tituloSerie" => "Acta Neurochir (Wien)"
"fecha" => "2013"
"volumen" => "155"
"paginaInicial" => "2237"
"paginaFinal" => "2242"
"link" => array:1 [ …1]
]
]
]
]
]
]
8 => array:3 [
"identificador" => "bib0045"
"etiqueta" => "9"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Surgical resection of incidental diffuse gliomas involving eloquent brain areas. Rationale, functional, epileptological and oncological outcomes"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.neuchi.2016.08.007"
"Revista" => array:6 [
"tituloSerie" => "Neurochirurgie"
"fecha" => "2017"
"volumen" => "63"
"paginaInicial" => "250"
"paginaFinal" => "258"
"link" => array:1 [ …1]
]
]
]
]
]
]
9 => array:3 [
"identificador" => "bib0050"
"etiqueta" => "10"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Surgically treated incidentally discovered low-grade gliomas are mostly IDH mutated and 1p19q co-deleted with favorable prognosis"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:6 [
"tituloSerie" => "Int J Clin Exp Pathol"
"fecha" => "2014"
"volumen" => "7"
"paginaInicial" => "8627"
"paginaFinal" => "8636"
"link" => array:1 [ …1]
]
]
]
]
]
]
10 => array:3 [
"identificador" => "bib0055"
"etiqueta" => "11"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Incidental low-grade gliomas: single-institution management based on clinical, surgical, and molecular data"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuros/nyz114"
"Revista" => array:6 [
"tituloSerie" => "Neurosurgery"
"fecha" => "2020"
"volumen" => "86"
"paginaInicial" => "391"
"paginaFinal" => "399"
"link" => array:1 [ …1]
]
]
]
]
]
]
11 => array:3 [
"identificador" => "bib0060"
"etiqueta" => "12"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s00401-016-1545-1"
"Revista" => array:6 [
"tituloSerie" => "Acta Neuropathol"
"fecha" => "2016"
"volumen" => "131"
"paginaInicial" => "803"
"paginaFinal" => "820"
"link" => array:1 [ …1]
]
]
]
]
]
]
12 => array:3 [
"identificador" => "bib0065"
"etiqueta" => "13"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Practical implications of integrated glioma classification according to the World Health Organization classification of tumors of the central nervous system 2016"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1097/CCO.0000000000000327"
"Revista" => array:6 [
"tituloSerie" => "Curr Opin Oncol"
"fecha" => "2016"
"volumen" => "28"
"paginaInicial" => "494"
"paginaFinal" => "501"
"link" => array:1 [ …1]
]
]
]
]
]
]
13 => array:3 [
"identificador" => "bib0070"
"etiqueta" => "14"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "IDH1 and IDH2 mutations in gliomas"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1056/NEJMoa0808710"
"Revista" => array:6 [
"tituloSerie" => "N Engl J Med"
"fecha" => "2009"
"volumen" => "360"
"paginaInicial" => "765"
"paginaFinal" => "773"
"link" => array:1 [ …1]
]
]
]
]
]
]
14 => array:3 [
"identificador" => "bib0075"
"etiqueta" => "15"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Prognostic significance of IDH mutation in adult low-grade gliomas: a meta-analysis"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-013-1107-5"
"Revista" => array:6 [
"tituloSerie" => "J Neurooncol"
"fecha" => "2013"
"volumen" => "113"
"paginaInicial" => "277"
"paginaFinal" => "284"
"link" => array:1 [ …1]
]
]
]
]
]
]
15 => array:3 [
"identificador" => "bib0080"
"etiqueta" => "16"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Allelic loss at 1p and 19q frequently occurs in association and may represent early oncogenic events in oligodendroglial tumors"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1002/ijc.2910640311"
"Revista" => array:6 [
"tituloSerie" => "Int J cancer"
"fecha" => "1995"
"volumen" => "64"
"paginaInicial" => "207"
"paginaFinal" => "210"
"link" => array:1 [ …1]
]
]
]
]
]
]
16 => array:3 [
"identificador" => "bib0085"
"etiqueta" => "17"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Molecular genetic analysis of oligodendroglial tumors shows preferential allelic deletions on 19q and 1p"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:6 [
"tituloSerie" => "Am J Pathol"
"fecha" => "1994"
"volumen" => "145"
"paginaInicial" => "1175"
"paginaFinal" => "1190"
"link" => array:1 [ …1]
]
]
]
]
]
]
17 => array:3 [
"identificador" => "bib0090"
"etiqueta" => "18"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC brain tumor group study 26951"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1200/JCO.2012.43.2229"
"Revista" => array:6 [
"tituloSerie" => "J Clin Oncol"
"fecha" => "2013"
"volumen" => "31"
"paginaInicial" => "344"
"paginaFinal" => "350"
"link" => array:1 [ …1]
]
]
]
]
]
]
18 => array:3 [
"identificador" => "bib0095"
"etiqueta" => "19"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Detection of allelic status of 1p and 19q by microsatellite-based PCR versus FISH: limitations and advantages in application to patient management"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1097/PDM.0b013e3181e961e9"
"Revista" => array:6 [
"tituloSerie" => "Diagn Mol Pathol"
"fecha" => "2011"
"volumen" => "20"
"paginaInicial" => "40"
"paginaFinal" => "47"
"link" => array:1 [ …1]
]
]
]
]
]
]
19 => array:3 [
"identificador" => "bib0100"
"etiqueta" => "20"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "FISHing Tips: What Every Clinician Should Know About 1p19q Analysis in Gliomas Using Fluorescence in situ Hybridisation"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.clon.2015.04.008"
"Revista" => array:6 [
"tituloSerie" => "Clin Oncol (R Coll Radiol)"
"fecha" => "2015"
"volumen" => "27"
"paginaInicial" => "445"
"paginaFinal" => "453"
"link" => array:1 [ …1]
]
]
]
]
]
]
20 => array:3 [
"identificador" => "bib0105"
"etiqueta" => "21"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "FISH-based detection of 1p 19q codeletion in oligodendroglial tumors: procedures and protocols for neuropathological practice - a publication under the auspices of the Research Committee of the European Confederation of Neuropathological Societies (Euro-CNS)"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.5414/npp30047"
"Revista" => array:6 [
"tituloSerie" => "Clin Neuropathol"
"fecha" => "2011"
"volumen" => "30"
"paginaInicial" => "47"
"paginaFinal" => "55"
"link" => array:1 [ …1]
]
]
]
]
]
]
21 => array:3 [
"identificador" => "bib0110"
"etiqueta" => "22"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "ATRX and IDH1-R132H immunohistochemistry with subsequent copy number analysis and IDH sequencing as a basis for an ‘integrated’ diagnostic approach for adult astrocytoma, oligodendroglioma and glioblastoma"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s00401-014-1370-3"
"Revista" => array:6 [
"tituloSerie" => "Acta Neuropathol"
"fecha" => "2015"
"volumen" => "129"
"paginaInicial" => "133"
"paginaFinal" => "146"
"link" => array:1 [ …1]
]
]
]
]
]
]
22 => array:3 [
"identificador" => "bib0115"
"etiqueta" => "23"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Clinical Neuropathology practice news 2-2014: ATRX, a new candidate biomarker in gliomas"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.5414/np300758"
"Revista" => array:6 [
"tituloSerie" => "Clin Neuropathol"
"fecha" => "2014"
"volumen" => "33"
"paginaInicial" => "108"
"paginaFinal" => "111"
"link" => array:1 [ …1]
]
]
]
]
]
]
23 => array:3 [
"identificador" => "bib0120"
"etiqueta" => "24"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Diffuse gliomas classified by 1p/19q co-deletion, TERT promoter and IDH mutation status are associated with specific genetic risk loci"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s00401-018-1825-z"
"Revista" => array:6 [
"tituloSerie" => "Acta Neuropathol"
"fecha" => "2018"
"volumen" => "135"
"paginaInicial" => "743"
"paginaFinal" => "755"
"link" => array:1 [ …1]
]
]
]
]
]
]
24 => array:3 [
"identificador" => "bib0125"
"etiqueta" => "25"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Glioma Groups Based on 1p/19q, IDH, and TERT Promoter Mutations in Tumors"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:5 [
"tituloSerie" => "N Engl J Med"
"fecha" => "2015"
"volumen" => "372"
"paginaInicial" => "2499"
"paginaFinal" => "2508"
]
]
]
]
]
]
25 => array:3 [
"identificador" => "bib0130"
"etiqueta" => "26"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "The 2021 WHO Classification of Tumors of the Central Nervous System: a summary"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuonc/noab106"
"Revista" => array:6 [
"tituloSerie" => "Neuro Oncol"
"fecha" => "2021"
"volumen" => "23"
"paginaInicial" => "1231"
"paginaFinal" => "1251"
"link" => array:1 [ …1]
]
]
]
]
]
]
26 => array:3 [
"identificador" => "bib0135"
"etiqueta" => "27"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1038/s41571-020-00447-z"
"Revista" => array:6 [
"tituloSerie" => "Nat Rev Clin Oncol"
"fecha" => "2021"
"volumen" => "18"
"paginaInicial" => "170"
"paginaFinal" => "186"
"link" => array:1 [ …1]
]
]
]
]
]
]
27 => array:3 [
"identificador" => "bib0140"
"etiqueta" => "28"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "cIMPACT-NOW update 6: new entity and diagnostic principle recommendations of the cIMPACT-Utrecht meeting on future CNS tumor classification and grading"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1111/bpa.12832"
"Revista" => array:6 [
"tituloSerie" => "Brain Pathol"
"fecha" => "2020"
"volumen" => "30"
"paginaInicial" => "844"
"paginaFinal" => "856"
"link" => array:1 [ …1]
]
]
]
]
]
]
28 => array:3 [
"identificador" => "bib0145"
"etiqueta" => "29"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Preferential brain locations of low-grade gliomas"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1002/cncr.20297"
"Revista" => array:6 [
"tituloSerie" => "Cancer"
"fecha" => "2004"
"volumen" => "100"
"paginaInicial" => "2622"
"paginaFinal" => "2626"
"link" => array:1 [ …1]
]
]
]
]
]
]
29 => array:3 [
"identificador" => "bib0150"
"etiqueta" => "30"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Impact of intraoperative stimulation brain mapping on glioma surgery outcome: A meta-analysis"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1200/JCO.2011.38.4818"
"Revista" => array:6 [
"tituloSerie" => "J Clin Oncol"
"fecha" => "2012"
"volumen" => "30"
"paginaInicial" => "2559"
"paginaFinal" => "2565"
"link" => array:1 [ …1]
]
]
]
]
]
]
30 => array:3 [
"identificador" => "bib0155"
"etiqueta" => "31"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Evaluation of the High-Frequency Monopolar Stimulation Technique for Mapping and Monitoring the Corticospinal Tract in Patients With Supratentorial Gliomas. A Proposal for Intraoperative Management Based on Neurophysiological Data Analysis in a Series of 92 patients"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuros/nyw087"
"Revista" => array:6 [
"tituloSerie" => "Neurosurgery"
"fecha" => "2017"
"volumen" => "81"
"paginaInicial" => "585"
"paginaFinal" => "594"
"link" => array:1 [ …1]
]
]
]
]
]
]
31 => array:3 [
"identificador" => "bib0160"
"etiqueta" => "32"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "The role of surgery in the management of patients with diffuse low grade glioma: A systematic review and evidence-based clinical practice guideline"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-015-1867-1"
"Revista" => array:6 [
"tituloSerie" => "J Neurooncol"
"fecha" => "2015"
"volumen" => "125"
"paginaInicial" => "503"
"paginaFinal" => "530"
"link" => array:1 [ …1]
]
]
]
]
]
]
32 => array:3 [
"identificador" => "bib0165"
"etiqueta" => "33"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "SEOM clinical guideline of diagnosis and management of low-grade glioma (2017)"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s12094-017-1790-3"
"Revista" => array:6 [
"tituloSerie" => "Clin Transl Oncol"
"fecha" => "2018"
"volumen" => "20"
"paginaInicial" => "3"
"paginaFinal" => "15"
"link" => array:1 [ …1]
]
]
]
]
]
]
33 => array:3 [
"identificador" => "bib0170"
"etiqueta" => "34"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Extent of resection in diffuse low-grade gliomas and the role of tumor molecular signature-a systematic review of the literature"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s10143-020-01362-8"
"Revista" => array:6 [
"tituloSerie" => "Neurosurg Rev"
"fecha" => "2021"
"volumen" => "44"
"paginaInicial" => "1371"
"paginaFinal" => "1389"
"link" => array:1 [ …1]
]
]
]
]
]
]
34 => array:3 [
"identificador" => "bib0175"
"etiqueta" => "35"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Spontaneous and therapeutic prognostic factors in adult hemispheric World Health Organization Grade II gliomas: a series of 1097 cases: clinical article"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/2013.1.JNS121"
"Revista" => array:6 [
"tituloSerie" => "J Neurosurg"
"fecha" => "2013"
"volumen" => "118"
"paginaInicial" => "1157"
"paginaFinal" => "1168"
"link" => array:1 [ …1]
]
]
]
]
]
]
35 => array:3 [
"identificador" => "bib0180"
"etiqueta" => "36"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "The role of biopsy in the management of patients with presumed diffuse low grade glioma: A systematic review and evidence-based clinical practice guideline"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-015-1866-2"
"Revista" => array:6 [
"tituloSerie" => "J Neurooncol"
"fecha" => "2015"
"volumen" => "125"
"paginaInicial" => "481"
"paginaFinal" => "501"
"link" => array:1 [ …1]
]
]
]
]
]
]
36 => array:3 [
"identificador" => "bib0185"
"etiqueta" => "37"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Limitations of stereotactic biopsy in the initial management of gliomas"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuonc/3.3.193"
"Revista" => array:6 [
"tituloSerie" => "Neuro Oncol"
"fecha" => "2001"
"volumen" => "3"
"paginaInicial" => "193"
"paginaFinal" => "200"
"link" => array:1 [ …1]
]
]
]
]
]
]
37 => array:3 [
"identificador" => "bib0190"
"etiqueta" => "38"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma: comparison of biopsy and open resection specimen"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1179/016164105X40057"
"Revista" => array:6 [
"tituloSerie" => "Neurol Res"
"fecha" => "2005"
"volumen" => "27"
"paginaInicial" => "358"
"paginaFinal" => "362"
"link" => array:1 [ …1]
]
]
]
]
]
]
38 => array:3 [
"identificador" => "bib0195"
"etiqueta" => "39"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "The effect of extent of resection on recurrence in patients with low grade cerebral hemisphere gliomas"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1002/1097-0142(19940915)74:6<1784::aid-cncr2820740622>3.0.co;2-d"
"Revista" => array:6 [
"tituloSerie" => "Cancer"
"fecha" => "1994"
"volumen" => "74"
"paginaInicial" => "1784"
"paginaFinal" => "1791"
"link" => array:1 [ …1]
]
]
]
]
]
]
39 => array:3 [
"identificador" => "bib0200"
"etiqueta" => "40"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas"
"autores" => array:1 [
0 => array:2 [ …2]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1200/JCO.2007.13.9337"
"Revista" => array:6 [
"tituloSerie" => "J Clin Oncol"
…5
]
]
]
]
]
]
40 => array:3 [
"identificador" => "bib0205"
"etiqueta" => "41"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Surgery for Diffuse WHO Grade II Gliomas: Volumetric Analysis of a Multicenter Retrospective Cohort From the German Study Group for Intraoperative Magnetic Resonance Imaging"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuros/nyz397"
"Revista" => array:6 [ …6]
]
]
]
]
]
41 => array:3 [
"identificador" => "bib0210"
"etiqueta" => "42"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Residual Tumor Volume as Best Outcome Predictor in Low Grade Glioma - A Nine-Years Near-Randomized Survey of Surgery vs"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1038/srep32286"
"Revista" => array:5 [ …5]
]
]
]
]
]
42 => array:3 [
"identificador" => "bib0215"
"etiqueta" => "43"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "An extent of resection threshold for seizure freedom in patients with low-grade gliomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/2016.12.JNS161682"
"Revista" => array:6 [ …6]
]
]
]
]
]
43 => array:3 [
"identificador" => "bib0220"
"etiqueta" => "44"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Extent of Resection and Residual Tumor Thresholds for Postoperative Total Seizure Freedom in Epileptic Adult Patients Harboring a Supratentorial Diffuse Low-Grade Glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuros/nyy481"
"Revista" => array:6 [ …6]
]
]
]
]
]
44 => array:3 [
"identificador" => "bib0225"
"etiqueta" => "45"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Diffuse low-grade oligodendrogliomas extend beyond MRI-defined abnormalities"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1212/WNL.0b013e3181e04264"
"Revista" => array:6 [ …6]
]
]
]
]
]
45 => array:3 [
"identificador" => "bib0230"
"etiqueta" => "46"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Awake surgery for WHO Grade II gliomas within ‘noneloquent’ areas in the left dominant hemisphere: toward a ‘supratotal’ resection. Clinical article"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/2011.3.JNS101333"
"Revista" => array:6 [ …6]
]
]
]
]
]
46 => array:3 [
"identificador" => "bib0235"
"etiqueta" => "47"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Association of supratotal resection with progression-free survival, malignant transformation, and overall survival in lower-grade gliomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuonc/noaa225"
"Revista" => array:6 [ …6]
]
]
]
]
]
47 => array:3 [
"identificador" => "bib0240"
"etiqueta" => "48"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Long-term outcomes after supratotal resection of diffuse low-grade gliomas: a consecutive series with 11-year follow-up"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s00701-015-2621-3"
"Revista" => array:6 [ …6]
]
]
]
]
]
48 => array:3 [
"identificador" => "bib0245"
"etiqueta" => "49"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Supratotal resection in glioma: a systematic review"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuonc/noy166"
"Revista" => array:6 [ …6]
]
]
]
]
]
49 => array:3 [
"identificador" => "bib0250"
"etiqueta" => "50"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Extent of Surgical Resection in Lower-Grade Gliomas: Differential Impact Based on Molecular Subtype"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3174/ajnr.A6102"
"Revista" => array:6 [ …6]
]
]
]
]
]
50 => array:3 [
"identificador" => "bib0255"
"etiqueta" => "51"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Contemporary assessment of extent of resection in molecularly defined categories of diffuse low-grade glioma: a volumetric analysis"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:4 [ …4]
]
]
]
]
]
51 => array:3 [
"identificador" => "bib0260"
"etiqueta" => "52"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Comparative volumetric analysis of the extent of resection of molecularly and histologically distinct low grade gliomas and its role on survival"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-017-2486-9"
"Revista" => array:6 [ …6]
]
]
]
]
]
52 => array:3 [
"identificador" => "bib0265"
"etiqueta" => "53"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Extent of resection and molecular pathologic subtype are potent prognostic factors of adult WHO grade II glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1038/s41598-020-59089-x"
"Revista" => array:5 [ …5]
]
]
]
]
]
53 => array:3 [
"identificador" => "bib0270"
"etiqueta" => "54"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Impact of gross total resection in patients with WHO grade III glioma harboring the IDH 1/2 mutation without the 1p/19q co-deletion"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-016-2201-2"
"Revista" => array:6 [ …6]
]
]
]
]
]
54 => array:3 [
"identificador" => "bib0275"
"etiqueta" => "55"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Extent of resection, molecular signature, and survival in 1p19q-codeleted gliomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/2020.2.JNS192767"
"Revista" => array:6 [ …6]
]
]
]
]
]
55 => array:3 [
"identificador" => "bib0280"
"etiqueta" => "56"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Impact of 1p/19q codeletion status on extent of resection in WHO grade II glioma: Insights from a national cancer registry"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.clineuro.2019.04.027"
"Revista" => array:6 [ …6]
]
]
]
]
]
56 => array:3 [
"identificador" => "bib0285"
"etiqueta" => "57"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Radiation plus Procarbazine, CCNU, and Vincristine in Low-Grade Glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1056/NEJMoa1500925"
"Revista" => array:6 [ …6]
]
]
]
]
]
57 => array:3 [
"identificador" => "bib0290"
"etiqueta" => "58"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Randomized trial of radiation therapy plus procarbazine, lomustine, and vincristine chemotherapy for supratentorial adult low-grade glioma: initial results of RTOG 9802"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1200/JCO.2011.35.8598"
"Revista" => array:6 [ …6]
]
]
]
]
]
58 => array:3 [
"identificador" => "bib0295"
"etiqueta" => "59"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "The Role of Extent of Resection in IDH1 Wild-Type or Mutant Low-Grade Gliomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuros/nyx265"
"Revista" => array:6 [ …6]
]
]
]
]
]
59 => array:3 [
"identificador" => "bib0300"
"etiqueta" => "60"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "IDH wild-type WHO grade II diffuse low-grade gliomas. A heterogeneous family with different outcomes. Systematic review and meta-analysis"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s10143-018-0996-3"
"Revista" => array:6 [ …6]
]
]
]
]
]
60 => array:3 [
"identificador" => "bib0305"
"etiqueta" => "61"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Huge heterogeneity in survival in a subset of adult patients with resected, wild-type isocitrate dehydrogenase status, WHO grade II astrocytomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:4 [ …4]
]
]
]
]
]
61 => array:3 [
"identificador" => "bib0310"
"etiqueta" => "62"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Survival of diffuse astrocytic glioma, IDH1/2 wildtype, with molecular features of glioblastoma, WHO grade IV: a confirmation of the cIMPACT-NOW criteria"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuonc/noz200"
"Revista" => array:6 [ …6]
]
]
]
]
]
62 => array:3 [
"identificador" => "bib0315"
"etiqueta" => "63"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Adult IDH wild-type lower-grade gliomas should be further stratified"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuonc/nox078"
"Revista" => array:6 [ …6]
]
]
]
]
]
63 => array:3 [
"identificador" => "bib0320"
"etiqueta" => "64"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/jns.1978.49.3.0333"
"Revista" => array:6 [ …6]
]
]
]
]
]
64 => array:3 [
"identificador" => "bib0325"
"etiqueta" => "65"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Radiotherapy for glioblastoma in the elderly"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1056/NEJMoa065901"
"Revista" => array:6 [ …6]
]
]
]
]
]
65 => array:3 [
"identificador" => "bib0330"
"etiqueta" => "66"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Prospective randomized trial of low- versus high-dose radiation therapy in adults with supratentorial low-grade glioma: initial report of a North Central Cancer Treatment Group/Radiation Therapy Oncology Group/Eastern Cooperative Oncology Group study"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1200/JCO.2002.09.126"
"Revista" => array:6 [ …6]
]
]
]
]
]
66 => array:3 [
"identificador" => "bib0335"
"etiqueta" => "67"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "A randomized trial on dose-response in radiation therapy of low-grade cerebral glioma: European Organization for Research and Treatment of Cancer (EORTC) Study 22844"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/s0360-3016(96)00352-5"
"Revista" => array:6 [ …6]
]
]
]
]
]
67 => array:3 [
"identificador" => "bib0340"
"etiqueta" => "68"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Final report from Intergroup NCCTG 86-72-51 (Alliance): a phase III randomized clinical trial of high-dose versus low-dose radiation for adult low-grade glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuonc/noaa021"
"Revista" => array:6 [ …6]
]
]
]
]
]
68 => array:3 [
"identificador" => "bib0345"
"etiqueta" => "69"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1200/JCO.2004.06.082"
"Revista" => array:6 [ …6]
]
]
]
]
]
69 => array:3 [
"identificador" => "bib0350"
"etiqueta" => "70"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "ESTRO-ACROP guideline ‘target delineation of glioblastomas’"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:5 [ …5]
]
]
]
]
]
70 => array:3 [
"identificador" => "bib0355"
"etiqueta" => "71"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Long-term neurocognitive and other side effects of radiotherapy, with or without chemotherapy, for glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1002/14651858.CD013047.pub2"
"Revista" => array:5 [ …5]
]
]
]
]
]
71 => array:3 [
"identificador" => "bib0360"
"etiqueta" => "72"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: the EORTC 22845 randomised trial"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/S0140-6736(05)67070-5"
"Revista" => array:6 [ …6]
]
]
]
]
]
72 => array:3 [
"identificador" => "bib0365"
"etiqueta" => "73"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Early versus delayed postoperative radiotherapy for treatment of low-grade gliomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1002/14651858.CD009229.pub3"
"Revista" => array:5 [ …5]
]
]
]
]
]
73 => array:3 [
"identificador" => "bib0370"
"etiqueta" => "74"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Prognostic factors for survival in adult patients with cerebral low-grade glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1200/JCO.2002.08.121"
"Revista" => array:6 [ …6]
]
]
]
]
]
74 => array:3 [
"identificador" => "bib0375"
"etiqueta" => "75"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Dosimetric advantages of proton therapy over conventional radiotherapy with photons in young patients and adults with low-grade glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s00066-016-1005-9"
"Revista" => array:6 [ …6]
]
]
]
]
]
75 => array:3 [
"identificador" => "bib0380"
"etiqueta" => "76"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Carbon ion radiotherapy in the treatment of gliomas: a review"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-019-03303-y"
"Revista" => array:6 [ …6]
]
]
]
]
]
76 => array:3 [
"identificador" => "bib0385"
"etiqueta" => "77"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Chemotherapy with vincristine (VCR) and etoposide (VP-16) in children with low-grade astrocytoma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/BF00177619"
"Revista" => array:6 [ …6]
]
]
]
]
]
77 => array:3 [
"identificador" => "bib0390"
"etiqueta" => "78"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Carboplatin and vincristine chemotherapy for children with newly diagnosed progressive low-grade gliomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/jns.1997.86.5.0747"
"Revista" => array:6 [ …6]
]
]
]
]
]
78 => array:3 [
"identificador" => "bib0395"
"etiqueta" => "79"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Central Nervous System Cancers, Version 3.2020, NCCN Clinical Practice Guidelines in Oncology"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.6004/jnccn.2020.0052"
"Revista" => array:6 [ …6]
]
]
]
]
]
79 => array:3 [
"identificador" => "bib0400"
"etiqueta" => "80"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Radiation and chemotherapy for high-risk lower grade gliomas: Choosing between temozolomide and PCV"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1002/cam4.2686"
"Revista" => array:6 [ …6]
]
]
]
]
]
80 => array:3 [
"identificador" => "bib0405"
"etiqueta" => "81"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Comprehensive Genomic Analysis in NRG Oncology/RTOG 9802: A Phase III Trial of Radiation Versus Radiation Plus Procarbazine, Lomustine (CCNU), and Vincristine in High-Risk Low-Grade Glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1200/JCO.19.02983"
"Revista" => array:6 [ …6]
]
]
]
]
]
81 => array:3 [
"identificador" => "bib0410"
"etiqueta" => "82"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Temozolomide chemotherapy versus radiotherapy in high-risk low-grade glioma (EORTC 22033-26033): a randomised, open-label, phase 3 intergroup study"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/S1470-2045(16)30313-8"
"Revista" => array:6 [ …6]
]
]
]
]
]
82 => array:3 [
"identificador" => "bib0415"
"etiqueta" => "83"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Recurrence following neurosurgeon-determined gross-total resection of adult supratentorial low-grade glioma: results of a prospective clinical trial"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/JNS/2008/109/11/0835"
"Revista" => array:6 [ …6]
]
]
]
]
]
83 => array:3 [
"identificador" => "bib0420"
"etiqueta" => "84"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Management of patients with recurrence of diffuse low grade glioma: A systematic review and evidence-based clinical practice guideline"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-015-1910-2"
"Revista" => array:6 [ …6]
]
]
]
]
]
84 => array:3 [
"identificador" => "bib0425"
"etiqueta" => "85"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Repeat surgery for recurrent low-grade gliomas should be standard of care"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.clineuro.2016.09.013"
"Revista" => array:6 [ …6]
]
]
]
]
]
85 => array:3 [
"identificador" => "bib0430"
"etiqueta" => "86"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Spatial distribution of malignant transformation in patients with low-grade glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-020-03391-1"
"Revista" => array:6 [ …6]
]
]
]
]
]
86 => array:3 [
"identificador" => "bib0435"
"etiqueta" => "87"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Quantitative morphological magnetic resonance imaging follow-up of low-grade glioma: a plea for systematic measurement of growth rates"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1227/NEU.0b013e31826213de"
"Revista" => array:6 [ …6]
]
]
]
]
]
87 => array:3 [
"identificador" => "bib0440"
"etiqueta" => "88"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Radiology reporting of low-grade glioma growth underestimates tumor expansion"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s00701-018-03783-3"
"Revista" => array:6 [ …6]
]
]
]
]
]
88 => array:3 [
"identificador" => "bib0445"
"etiqueta" => "89"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Cognitive and radiological effects of radiotherapy in patients with low-grade glioma: long-term follow-up"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/S1474-4422(09)70204-2"
"Revista" => array:6 [ …6]
]
]
]
]
]
89 => array:3 [
"identificador" => "bib0450"
"etiqueta" => "90"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Stereotactic Radiosurgery for Low-Grade Gliomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1159/000493063"
"Revista" => array:6 [ …6]
]
]
]
]
]
90 => array:3 [
"identificador" => "bib0455"
"etiqueta" => "91"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Gamma knife radiosurgery for recurrent gliomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-018-2988-0"
"Revista" => array:6 [ …6]
]
]
]
]
]
91 => array:3 [
"identificador" => "bib0460"
"etiqueta" => "92"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Outcomes Following Proton Therapy for Pediatric Low-Grade Glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.ijrobp.2019.01.078"
"Revista" => array:6 [ …6]
]
]
]
]
]
92 => array:3 [
"identificador" => "bib0465"
"etiqueta" => "93"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Long-term outcomes and late adverse effects of a prospective study on proton radiotherapy for patients with low-grade glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:1 [
"Revista" => array:5 [ …5]
]
]
]
]
]
93 => array:3 [
"identificador" => "bib0470"
"etiqueta" => "94"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Proton therapy for low-grade gliomas: Results from a prospective trial"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1002/cncr.29237"
"Revista" => array:6 [ …6]
]
]
]
]
]
94 => array:3 [
"identificador" => "bib0475"
"etiqueta" => "95"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Neurocognitive effects of proton radiation therapy in adults with low-grade glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-015-1952-5"
"Revista" => array:6 [ …6]
]
]
]
]
]
95 => array:3 [
"identificador" => "bib0480"
"etiqueta" => "96"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Proton therapy for low-grade gliomas in adults: A systematic review"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.clineuro.2018.08.003"
"Revista" => array:6 [ …6]
]
]
]
]
]
96 => array:3 [
"identificador" => "bib0485"
"etiqueta" => "97"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "BRAF Inhibition in BRAF(V600)-Mutant Gliomas: Results From the VE-BASKET Study"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1200/JCO.2018.78.9990"
"Revista" => array:6 [ …6]
]
]
]
]
]
97 => array:3 [
"identificador" => "bib0490"
"etiqueta" => "98"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Dabrafenib and trametinib in BRAFV600E mutated glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.2217/cns-2017-0006"
"Revista" => array:6 [ …6]
]
]
]
]
]
98 => array:3 [
"identificador" => "bib0495"
"etiqueta" => "99"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Efficacy and safety of everolimus for subependymal giant cell astrocytomas associated with tuberous sclerosis complex (EXIST-1): a multicentre, randomised, placebo-controlled phase 3 trial"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/S0140-6736(12)61134-9"
"Revista" => array:6 [ …6]
]
]
]
]
]
99 => array:3 [
"identificador" => "bib0500"
"etiqueta" => "100"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Epidemiology of glioma: clinical characteristics, symptoms, and predictors of glioma patients grade I-IV in the the Danish Neuro-Oncology Registry"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-017-2607-5"
"Revista" => array:6 [ …6]
]
]
]
]
]
100 => array:3 [
"identificador" => "bib0505"
"etiqueta" => "101"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Supratentorial low-grade gliomas in older patients"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1212/WNL.0b013e3181c6781e"
"Revista" => array:6 [ …6]
]
]
]
]
]
101 => array:3 [
"identificador" => "bib0510"
"etiqueta" => "102"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Patterns of care and treatment outcomes in older adults with low grade glioma: a 50-year experience"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-017-2439-3"
"Revista" => array:6 [ …6]
]
]
]
]
]
102 => array:3 [
"identificador" => "bib0515"
"etiqueta" => "103"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Age and surgical outcome of low-grade glioma in Sweden"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1111/ane.12973"
"Revista" => array:6 [ …6]
]
]
]
]
]
103 => array:3 [
"identificador" => "bib0520"
"etiqueta" => "104"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Procarbazine, CCNU and vincristine (PCV) versus temozolomide chemotherapy for patients with low-grade glioma: a systematic review"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.18632/oncotarget.25890"
"Revista" => array:6 [ …6]
]
]
]
]
]
104 => array:3 [
"identificador" => "bib0525"
"etiqueta" => "105"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Molecular features and clinical outcomes in surgically treated low-grade diffuse gliomas in patients over the age of 60"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-018-03044-4"
"Revista" => array:6 [ …6]
]
]
]
]
]
105 => array:3 [
"identificador" => "bib0530"
"etiqueta" => "106"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Confocal scanning microscopy provides rapid, detailed intraoperative histological assessment of brain neoplasms: Experience with 106 cases"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.clineuro.2018.03.015"
"Revista" => array:6 [ …6]
]
]
]
]
]
106 => array:3 [
"identificador" => "bib0535"
"etiqueta" => "107"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Laser Interstitial Thermal Therapy as a Primary Treatment for Deep Inaccessible Gliomas"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuros/nyy238"
"Revista" => array:6 [ …6]
]
]
]
]
]
107 => array:3 [
"identificador" => "bib0540"
"etiqueta" => "108"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Maximizing safe resection of low- and high-grade glioma"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s11060-016-2110-4"
"Revista" => array:6 [ …6]
]
]
]
]
]
108 => array:3 [
"identificador" => "bib0545"
"etiqueta" => "109"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Launching Effectiveness Research to Guide Practice in Neurosurgery: A National Institute Neurological Disorders and Stroke Workshop Report"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuros/nyw133"
"Revista" => array:6 [ …6]
]
]
]
]
]
109 => array:3 [
"identificador" => "bib0550"
"etiqueta" => "110"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Three-Dimensional Printed Modeling of Diffuse Low-Grade Gliomas and Associated White Matter Tract Anatomy"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/neuros/nyx009"
"Revista" => array:6 [ …6]
]
]
]
]
]
110 => array:3 [
"identificador" => "bib0555"
"etiqueta" => "111"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Hybrid computed tomography and magnetic resonance imaging 3D printed models for neurosurgery planning"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.21037/atm.2019.10.109"
"Revista" => array:5 [ …5]
]
]
]
]
]
111 => array:3 [
"identificador" => "bib0560"
"etiqueta" => "112"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "3D Printing of Diffuse Low-Grade Gliomas Involving Eloquent Cortical Areas and Subcortical Functional Pathways: Technical Note"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.wneu.2020.12.082"
"Revista" => array:6 [ …6]
]
]
]
]
]
112 => array:3 [
"identificador" => "bib0565"
"etiqueta" => "113"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Frontal pathways in cognitive control: direct evidence from intraoperative stimulation and diffusion tractography"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/brain/awz178"
"Revista" => array:6 [ …6]
]
]
]
]
]
113 => array:3 [
"identificador" => "bib0570"
"etiqueta" => "114"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Challenging the Myth of Right Nondominant Hemisphere: Lessons from Corticosubcortical Stimulation Mapping in Awake Surgery and Surgical Implications"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.wneu.2017.04.021"
"Revista" => array:6 [ …6]
]
]
]
]
]
114 => array:3 [
"identificador" => "bib0575"
"etiqueta" => "115"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Patients with incidental WHO grade II glioma frequently suffer from neuropsychological disturbances"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s00701-015-2674-3"
"Revista" => array:6 [ …6]
]
]
]
]
]
115 => array:3 [
"identificador" => "bib0580"
"etiqueta" => "116"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "[An atlas of neuroplastic potential in brain-damaged patients]"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1051/medsci/20173301014"
"Revista" => array:6 [ …6]
]
]
]
]
]
116 => array:3 [
"identificador" => "bib0585"
"etiqueta" => "117"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Glioma surgery under awake condition can lead to good independence and functional outcome excluding deep sensation and visuospatial cognition"
"autores" => array:1 [ …1]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/nop/npy054"
"Revista" => array:6 [ …6]
]
]
]
]
]
]
]
]
]
]
"idiomaDefecto" => "en"
"url" => "/25298496/0000003400000003/v1_202305031136/S2529849622000764/v1_202305031136/en/main.assets"
"Apartado" => array:4 [
"identificador" => "63440"
"tipo" => "SECCION"
"en" => array:2 [
"titulo" => "Special article"
"idiomaDefecto" => true
]
"idiomaDefecto" => "en"
]
"PDF" => "https://static.elsevier.es/multimedia/25298496/0000003400000003/v1_202305031136/S2529849622000764/v1_202305031136/en/main.pdf?idApp=UINPBA00004B&text.app=https://revistaneurocirugia.com/"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849622000764?idApp=UINPBA00004B"
]