Compartir
array:22 [
"pii" => "S2529849624000340"
"issn" => "25298496"
"doi" => "10.1016/j.neucie.2024.06.002"
"estado" => "S200"
"fechaPublicacion" => "2024-07-22"
"aid" => "614"
"copyright" => "Sociedad Española de Neurocirugía"
"copyrightAnyo" => "2024"
"documento" => "simple-article"
"crossmark" => 0
"subdocumento" => "crp"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"itemSiguiente" => array:18 [
"pii" => "S2529849624000443"
"issn" => "25298496"
"doi" => "10.1016/j.neucie.2024.07.005"
"estado" => "S200"
"fechaPublicacion" => "2024-08-01"
"aid" => "616"
"copyright" => "Sociedad Española de Neurocirugía"
"documento" => "simple-article"
"crossmark" => 0
"subdocumento" => "crp"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"en" => array:12 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Case Report</span>"
"titulo" => "Giant solitary fibrous tumor of the olfactory groove. An unusual simulator in an unusual location"
"tienePdf" => "en"
"tieneTextoCompleto" => "en"
"tieneResumen" => array:2 [
0 => "en"
1 => "es"
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Tumor fibroso solitario gigante del surco olfatorio. Un simulador inusual en una localización inusual"
]
]
"contieneResumen" => array:2 [
"en" => true
"es" => true
]
"contieneTextoCompleto" => array:1 [
"en" => true
]
"contienePdf" => array:1 [
"en" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:8 [
"identificador" => "fig0015"
"etiqueta" => "Fig. 3"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr3.jpeg"
"Alto" => 1739
"Ancho" => 1650
"Tamanyo" => 1069824
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0015"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Postoperative phase. Pathology study. (a) Haematoxylin-eosin stain 10×. Mesenchymal proliferation arranged in a swirling growth pattern, consisting of spindle cells and occasional interspersed thin bands of collagenous tissue. They are accompanied by frequent branching blood vessels with perivascular hyalinisation. (b) Haematoxylin-eosin stain 40×. Spindle-shaped tumour cells (predominant), ovoid and round, with elongated nuclei and few atypical nuclei. No significant mitotic activity or areas of necrosis are evident. (c) CD34 immunohistochemistry 20×. Positive diffuse cytoplasmic CD34 immunoreactivity. (d) STAT6 immunohistochemistry 20×. Highly-specific and sensitive STAT6 nuclear staining of solitary fibrous tumour.</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "Fernando García Pérez, Ascensión Contreras Jiménez, Beatriz Agredano Ávila, José Masegosa González"
"autores" => array:4 [
0 => array:2 [
"nombre" => "Fernando"
"apellidos" => "García Pérez"
]
1 => array:2 [
"nombre" => "Ascensión"
"apellidos" => "Contreras Jiménez"
]
2 => array:2 [
"nombre" => "Beatriz"
"apellidos" => "Agredano Ávila"
]
3 => array:2 [
"nombre" => "José"
"apellidos" => "Masegosa González"
]
]
]
]
]
"idiomaDefecto" => "en"
"Traduccion" => array:1 [
"es" => array:9 [
"pii" => "S1130147324000770"
"doi" => "10.1016/j.neucir.2024.07.001"
"estado" => "S200"
"subdocumento" => ""
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"idiomaDefecto" => "es"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S1130147324000770?idApp=UINPBA00004B"
]
]
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849624000443?idApp=UINPBA00004B"
"url" => "/25298496/unassign/S2529849624000443/v1_202408010420/en/main.assets"
]
"itemAnterior" => array:16 [
"pii" => "S2529849624000352"
"issn" => "25298496"
"doi" => "10.1016/j.neucie.2024.06.003"
"estado" => "S200"
"fechaPublicacion" => "2024-07-11"
"aid" => "615"
"documento" => "article"
"crossmark" => 0
"subdocumento" => "fla"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"en" => array:12 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Clinical Research</span>"
"titulo" => "Integrating endovascular techniques into established open neurosurgery practice: a temporal analysis of treatment evolution in a dual-trained neurosurgical unit"
"tienePdf" => "en"
"tieneTextoCompleto" => "en"
"tieneResumen" => array:2 [
0 => "en"
1 => "es"
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Integración de técnicas endovasculares en la práctica de la neurocirugía abierta: análisis temporal de la evolución del tratamiento en una unidad de neurocirugía vascular dual"
]
]
"contieneResumen" => array:2 [
"en" => true
"es" => true
]
"contieneTextoCompleto" => array:1 [
"en" => true
]
"contienePdf" => array:1 [
"en" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:8 [
"identificador" => "fig0005"
"etiqueta" => "Fig. 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 1526
"Ancho" => 2508
"Tamanyo" => 226263
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0005"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">The graph illustrates the evolution of treatment modality preferences over time, as represented by the rolling average proportion of EN (ENDO) and ON (OPEN) neurosurgical procedures. The navy blue line indicates the proportion of OPEN procedures, while the crimson line represents the ENDO procedures.</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "Ignacio Arrese, Sergio García-García, Santiago Cepeda, Rosario Sarabia"
"autores" => array:4 [
0 => array:2 [
"nombre" => "Ignacio"
"apellidos" => "Arrese"
]
1 => array:2 [
"nombre" => "Sergio"
"apellidos" => "García-García"
]
2 => array:2 [
"nombre" => "Santiago"
"apellidos" => "Cepeda"
]
3 => array:2 [
"nombre" => "Rosario"
"apellidos" => "Sarabia"
]
]
]
]
]
"idiomaDefecto" => "en"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849624000352?idApp=UINPBA00004B"
"url" => "/25298496/unassign/S2529849624000352/v1_202407110420/en/main.assets"
]
"en" => array:18 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Case Report</span>"
"titulo" => "Chiari malformation presenting with subarachnoid hemorrhage: a case report"
"tieneTextoCompleto" => true
"autores" => array:1 [
0 => array:4 [
"autoresLista" => "Samantha Schimmel, Molly Monsour, Davide Marco Croci"
"autores" => array:3 [
0 => array:3 [
"nombre" => "Samantha"
"apellidos" => "Schimmel"
"referencia" => array:1 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">a</span>"
"identificador" => "aff0005"
]
]
]
1 => array:3 [
"nombre" => "Molly"
"apellidos" => "Monsour"
"referencia" => array:1 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">a</span>"
"identificador" => "aff0005"
]
]
]
2 => array:4 [
"nombre" => "Davide Marco"
"apellidos" => "Croci"
"email" => array:1 [
0 => "davidecroci@usf.edu"
]
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">b</span>"
"identificador" => "aff0010"
]
1 => array:2 [
"etiqueta" => "*"
"identificador" => "cor0005"
]
]
]
]
"afiliaciones" => array:2 [
0 => array:3 [
"entidad" => "University of South Florida Morsani College of Medicine, Tampa, FL, USA"
"etiqueta" => "a"
"identificador" => "aff0005"
]
1 => array:3 [
"entidad" => "Department of Neurosurgery and Brain Repair, University of South Florida, Morsani College of Medicine, Tampa, Florida, USA"
"etiqueta" => "b"
"identificador" => "aff0010"
]
]
"correspondencia" => array:1 [
0 => array:3 [
"identificador" => "cor0005"
"etiqueta" => "⁎"
"correspondencia" => "<span class="elsevierStyleItalic">Corresponding author</span>."
]
]
]
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "La malformación de Chiari que presenta como una hemorragia subaracnoideo: caso clínico"
]
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:8 [
"identificador" => "fig0005"
"etiqueta" => "Fig. 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 2511
"Ancho" => 2508
"Tamanyo" => 475300
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0005"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
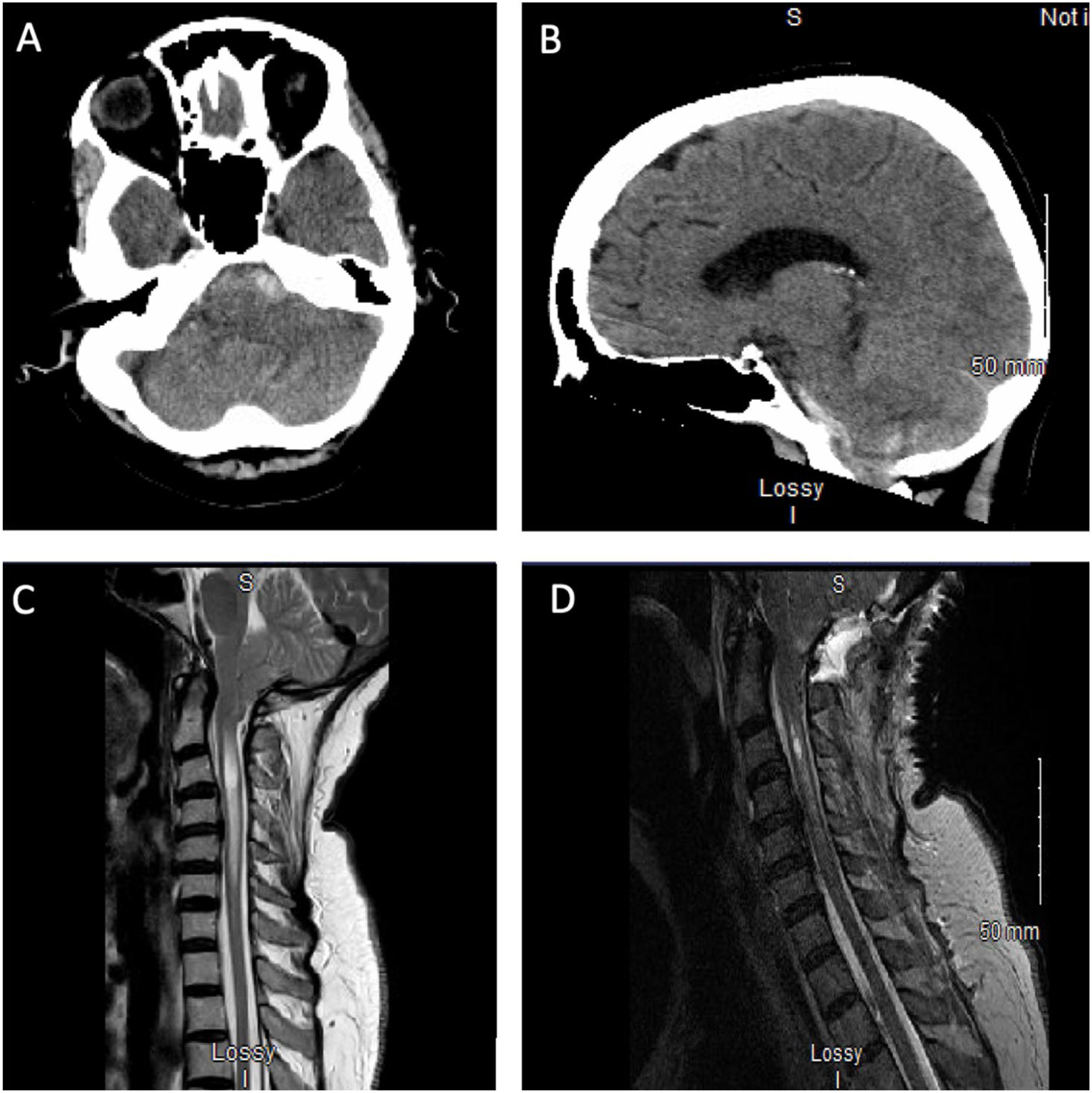
"en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Both the axial (A) and sagittal (B) pre-operative CT images show SAH in the upper cervical spine, anterior to the medulla and lower pons with extension into the left cerebellopontine angle. There is cisterna magna crowding and acute blood products in the posterior fossa and bilateral sylvian fissures. The patient’s pre-operative (C) and post-operative (D) T2 sagittal MRIs demonstrate a CM and syrinx. The preoperative image (C) shows a CM with tonsillar descent below the foramen magnum and a syrinx extending from C2 to C6. 2 days post-operatively (D), tonsillar descent and the syrinx were notably improved.</p>"
]
]
]
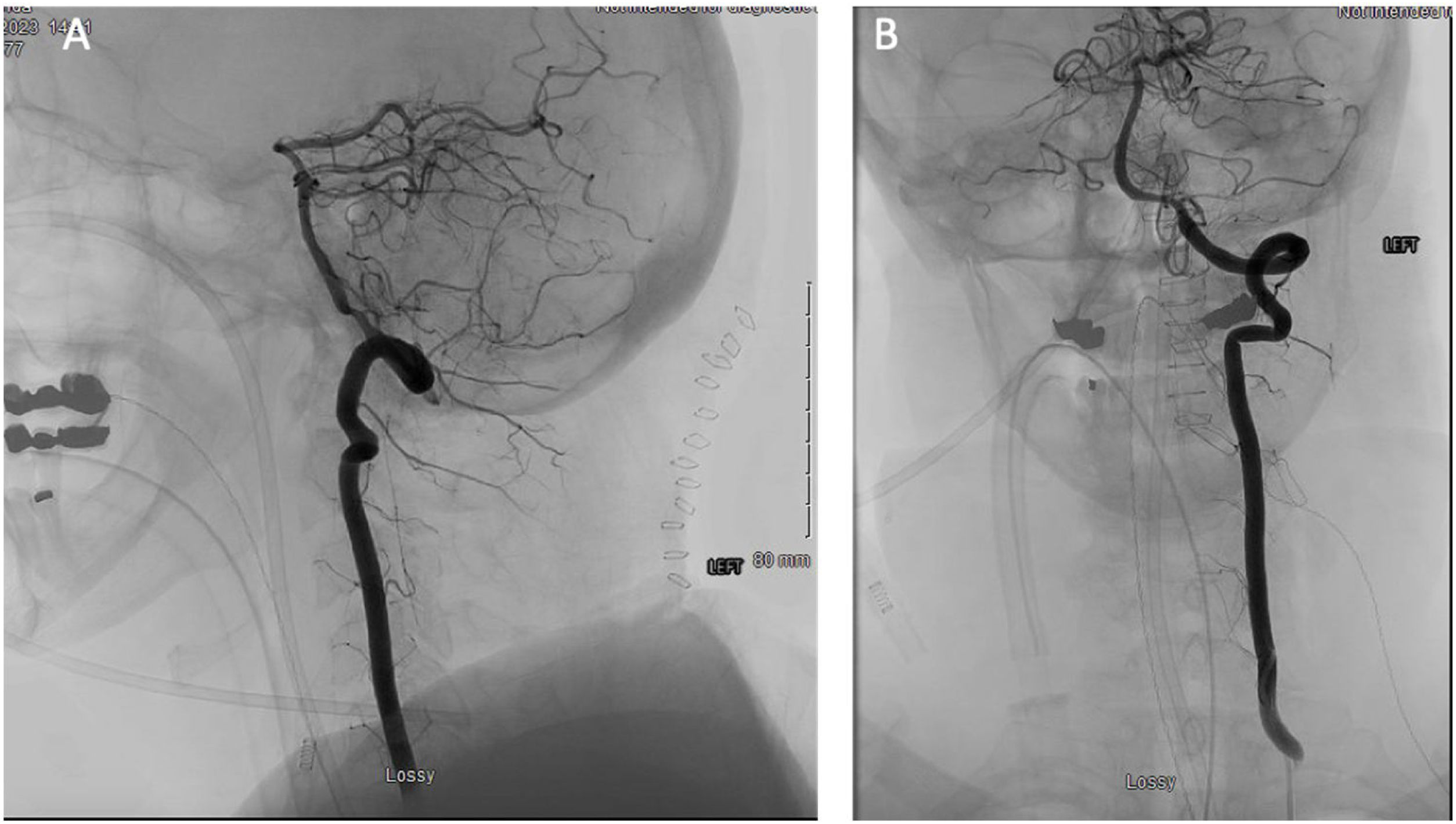
"textoCompleto" => "<span class="elsevierStyleSections"><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0020">Introduction</span><p id="par0005" class="elsevierStylePara elsevierViewall">Chiari malformations (CM) are structural defects characterized by the caudal herniation of the cerebellar tonsils through the foramen magnum.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> Cerebellar tonsil descent may cause overcrowding at and/or below the level of the cervicomedullary junction, increasing the risk of brainstem and spinal cord injury.<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a> CMs are often diagnosed in childhood, with an incidence of only 0.77% in adults.<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a> While they can be asymptomatic, patients with CM may develop syringomyelia and increased intracranial pressure (ICP).<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a> The pathophysiology of CMs and their complications is not yet fully elucidated, but one possibility involves the obstruction of cerebrospinal fluid (CSF) at the cervicomedullary junction.<a class="elsevierStyleCrossRefs" href="#bib0005"><span class="elsevierStyleSup">1,3</span></a> Cerebellar tonsil descent into the central canal can cause repeated trauma to cerebral and spinal arteries, increasing the risk of vascular complications and implicating CM in cerebrovascular events.<a class="elsevierStyleCrossRef" href="#bib0015"><span class="elsevierStyleSup">3</span></a> While symptomatic CMs are typically treated surgically, surgical complications can be as high as 22% and leave patients with significant impairments.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a></p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0025">Case report</span><p id="par0010" class="elsevierStylePara elsevierViewall">A 65-year-old female arrived at the emergency room with the “worst headache of her life”, neck pain, nausea, vomiting, and imbalance for the past six months. Upon arrival, a CT was ordered and showed an intracranial hemorrhage (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). A CT angiogram (CTA) revealed an acute subarachnoid hemorrhage (SAH) in the upper cervical spine, anterior to the medulla and lower pons with extension into the left cerebellopontine angle. No aneurysm or vascular malformation were notable. CTA and a six-vessel cerebral angiogram elucidated a 2 mm aneurysm arising from the cavernous/supraclinoid left internal carotid artery which was far from the bleeding location and not the cause of the hemorrhage. Suspicion of CM was seen on CT and confirmed with C-spine MRI, which also showed a syrinx (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). After multiple discussions between the endovascular and neurosurgical teams, indication for suboccipital craniectomy for a Chiari decompression with a C1 laminectomy was made. Given the patient’s symptoms and especially the imaging findings demonstrating a severe Chiari malformation with syringomyelia, and cervical spinal cord edema, it was decided to perform a decompressive suboccipital craniectomy craniotomy with the potential of tonsillar decompression uncovering the bleeding source, such as en eventual arteriovenous malformation or venous anomaly that was “compressed” due to the bleeding and the Chiari, in a post-operative angiogram. It was also necessary to decompress the spinal cord as early as possible considering the severe edema. Due to the concern of vasospasm, the mean arterial pressure was kept above 90 mmHg during the procedure to maintain cerebral perfusion.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0015" class="elsevierStylePara elsevierViewall">In the operating room, the patient was positioned prone using neuro-monitoring and the mayfield clamp. A skin incision was made using bovie subcutaneous dissection along the linea nuchae in the avascular plane. The C1 vertebral body, foramen magnum, and occipital bone were visualized. Subsequently, the microscope was used to perform a suboccipital craniectomy and C1 laminectomy. The dura under the occipital bone was highly vascularized, necessitating careful opening with a 15 Blade. Approaching the midline, the suboccipital sinus was broad with multiple branches along the dura bilaterally. Continuous hemostasis with hemoclips and 4.0 sutures were used while progressing caudally until below the C1 arch. All encountered dura was thick and rich with sinusoidal "venous lakes". Following dura opening and hemostasis, an arachnoid knife was used to perform an arachnoidolysis and free the herniated tonsils. The left dominant posterior inferior cerebellar artery was visualized and protected. The tonsils were partially shrunk with the bipolar. The surgical site was closed appropriately without procedural complications.</p><p id="par0020" class="elsevierStylePara elsevierViewall">The post-operative angiography showed a 50% stenosis of the left V4 segment, likely related to vasospasm, and no bleeding cause was identified (<a class="elsevierStyleCrossRef" href="#fig0010">Fig. 2</a>). Postoperative MRI demonstrated a well decompressed foramen magnum and improvement of the syringomyelia (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). At three-month follow-up, the patient reported no new headaches, improved balance, and some residual dizziness. An additional angiogram at 3 months follow-up confirmed the absence of a bleeding source (<a class="elsevierStyleCrossRef" href="#fig0010">Fig. 2</a>). At 18 months follow-up, angiogram continued to be negative and the patient remained neurologically intact and without headache.</p><elsevierMultimedia ident="fig0010"></elsevierMultimedia></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0030">Discussion</span><p id="par0025" class="elsevierStylePara elsevierViewall">SAH is rarely associated with CM, but limited literature indicates that patients with CM may be at risk of developing vascular pathology. To our knowledge, this is the first case of CM presenting with an angionegative SAH. Our patient presented with a severe headache, neck pain, nausea, and vomiting and CT revealed an acute SAH and possible CM. MRI confirmed the CM, and the patient was successfully treated with a suboccipital craniectomy for a Chiari decompression with a C1 laminectomy.</p><p id="par0030" class="elsevierStylePara elsevierViewall">While many patients with CM are asymptomatic, some present with symptoms related to increased ICP or neural structure compression, including headaches, nausea, vomiting, and signs of brainstem and cerebellar dysfunction (i.e., cranial nerve palsies, sensory deficits, and motor deficits). Surgical management of CM often involves reducing cerebellar tonsil herniation with posterior fossa decompression.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> During posterior fossa decompression, the neurosurgeon performs a suboccipital craniectomy to widen the foramen magnum and reduce posterior fossa overcrowding.</p><p id="par0035" class="elsevierStylePara elsevierViewall">Angionegative SAH, occurring in 15% of SAH, describes an SAH with initially negative findings on non-invasive vascular imaging and digital subtraction angiography.<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a> While our patient’s angionegative SAH could have occurred spontaneously and independently from her CM, the extreme overcrowding at her foramen magnum may have resulted in the hemorrhage. While further research is needed to establish an association between CM and SAH, overcrowding at the foramen magnum and concurrent decreased subarachnoid space indicate that these two conditions may share pathological features.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> For example, Mascitelli et al., described a patient who presented with SAH and was later diagnosed with CM, demonstrating that CM may increase the risk of SAH.<a class="elsevierStyleCrossRef" href="#bib0015"><span class="elsevierStyleSup">3</span></a> Additionally, a retrospective study of 21 adults with CM found that surgical management of CM related to decreased CSF obstruction at the foramen magnum and tonsillar pulsatility, both of which predispose patients to symptomatic disease and vascular dissection.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a></p><p id="par0040" class="elsevierStylePara elsevierViewall">Our patient’s venous drainage pattern was not notably abnormal based on CT angiograms, suggesting anatomical cerebral venous drainage impairment did not play a role in their presentation. It is important to consider, however, venous drainage impairment as a cause for angionegative SAH.<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a> Considering the severity of tonsillar herniation, venous drainage at level of the foramen magnum/inferior fossa might have been obstructed. Especially in Chiari malformations, venous drainage impairment can occur due to the obstructive nature of the pathology.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> In an analysis of hemodynamics in 21 patients with Chiari malformations,<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> the presence of a syrinx, as in our patient, increased the vitality of accessory venous pathways, or non-internal jugular vein pathways. This venous drainage pattern may result in higher flow through smaller veins, increasing the risk of an impaired venous drainage pattern.</p><p id="par0045" class="elsevierStylePara elsevierViewall">Ehlers-Danlos Syndrome (EDS), a connective tissue disorder causing joint hypermobility and tissue fragility, has also been postulated to increase the risk for hemorrhages and structural brain diseases like CM.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">6</span></a> The underlying mechanism may involve defective blood vessel collagen, dysfunctional ligaments, and abnormal mechanics at the craniocervical junction.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">6</span></a> While our patient lacked a family history and typical EDS symptomatology, a concurrent diagnosis of EDS cannot be ruled out due to a lack of genetic testing.</p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0035">Conclusion</span><p id="par0050" class="elsevierStylePara elsevierViewall">CMs rarely present with SAH. Clinical management necessitates multidisciplinary collaboration to manage both the SAH and tonsillar herniation. Decreased posterior fossa crowding following CM resolution may have implications for the management of cerebrovascular events.</p></span><span id="sec1020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect1035">Conflict of interest</span><p id="par1050" class="elsevierStylePara elsevierViewall">No conflict of interest.</p></span></span>"
"textoCompletoSecciones" => array:1 [
"secciones" => array:10 [
0 => array:3 [
"identificador" => "xres2206343"
"titulo" => "Abstract"
"secciones" => array:1 [
0 => array:1 [
"identificador" => "abst0005"
]
]
]
1 => array:2 [
"identificador" => "xpalclavsec1850963"
"titulo" => "Keywords"
]
2 => array:3 [
"identificador" => "xres2206344"
"titulo" => "Resumen"
"secciones" => array:1 [
0 => array:1 [
"identificador" => "abst0010"
]
]
]
3 => array:2 [
"identificador" => "xpalclavsec1850964"
"titulo" => "Palabras claves"
]
4 => array:2 [
"identificador" => "sec0005"
"titulo" => "Introduction"
]
5 => array:2 [
"identificador" => "sec0010"
"titulo" => "Case report"
]
6 => array:2 [
"identificador" => "sec0015"
"titulo" => "Discussion"
]
7 => array:2 [
"identificador" => "sec0020"
"titulo" => "Conclusion"
]
8 => array:2 [
"identificador" => "sec1020"
"titulo" => "Conflict of interest"
]
9 => array:1 [
"titulo" => "References"
]
]
]
"pdfFichero" => "main.pdf"
"tienePdf" => true
"fechaRecibido" => "2024-04-02"
"fechaAceptado" => "2024-06-19"
"PalabrasClave" => array:2 [
"en" => array:1 [
0 => array:4 [
"clase" => "keyword"
"titulo" => "Keywords"
"identificador" => "xpalclavsec1850963"
"palabras" => array:4 [
0 => "Chiari malformation"
1 => "Subarachnoid hemorrhage"
2 => "Syrinx"
3 => "C1 laminectomy"
]
]
]
"es" => array:1 [
0 => array:4 [
"clase" => "keyword"
"titulo" => "Palabras claves"
"identificador" => "xpalclavsec1850964"
"palabras" => array:4 [
0 => "Malformación de Chiari"
1 => "Hemorragia subaracnoideo"
2 => "Syrinx"
3 => "Laminectomía de C1"
]
]
]
]
"tieneResumen" => true
"resumen" => array:2 [
"en" => array:2 [
"titulo" => "Abstract"
"resumen" => "<span id="abst0005" class="elsevierStyleSection elsevierViewall"><p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Chiari malformations (CM) are often diagnosed in childhood and younger adults, with an incidence of only 0.77% in adult populations. Patients with CM may develop syringomyelia and increased intracranial pressure (ICP) due to cerebrospinal fluid (CSF) obstruction and altered fluid dynamics at the cervicomedullary junction. We describe the case of a 65-year-old female presenting with an angionegative subarachnoid hemorrhage (SAH) with concomitant new diagnosis of CM type I with syringomyelia. After ruling out any aneurysm or vascular malformations, she underwent a suboccipital craniectomy for a Chiari decompression with a C1 laminectomy. There were no complications with the surgery and her symptoms improved. This case report highlights the unusual presentation of a CM.</p></span>"
]
"es" => array:2 [
"titulo" => "Resumen"
"resumen" => "<span id="abst0010" class="elsevierStyleSection elsevierViewall"><p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">A menudo, las malformaciones de Chiari (CM) son diagnosticadas en los niños y los adultos jóvenes, y la incidencia en la populación adulto es solamente 0.77%. A veces, los pacientes con CM desarrollan una siringomielia y la hipertensión intracraneal debido a la obstrucción del líquido cefalorraquídeo y los cambios a los dinámicos del fluido a la unión craneocervical. Nosotros describimos el caso de una mujer de 65-años que presentó con una hemorragia subaracnoideo, que no apareció en el angiograma, y con un nuevo diagnóstico de CM 1 con una siringomielia. Después de nosotros excluimos cualquier aneurisma o malformación vascular, hicimos una craneotomía suboccipital para una descompresión de Chiari con una laminectomía de C1. No fue otras complicaciones con la cirugía y sus síntomas mejoraron. Este caso clínico recalca una presentación anormal de una CM.</p></span>"
]
]
"multimedia" => array:2 [
0 => array:8 [
"identificador" => "fig0005"
"etiqueta" => "Fig. 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 2511
"Ancho" => 2508
"Tamanyo" => 475300
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0005"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Both the axial (A) and sagittal (B) pre-operative CT images show SAH in the upper cervical spine, anterior to the medulla and lower pons with extension into the left cerebellopontine angle. There is cisterna magna crowding and acute blood products in the posterior fossa and bilateral sylvian fissures. The patient’s pre-operative (C) and post-operative (D) T2 sagittal MRIs demonstrate a CM and syrinx. The preoperative image (C) shows a CM with tonsillar descent below the foramen magnum and a syrinx extending from C2 to C6. 2 days post-operatively (D), tonsillar descent and the syrinx were notably improved.</p>"
]
]
1 => array:8 [
"identificador" => "fig0010"
"etiqueta" => "Fig. 2"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr2.jpeg"
"Alto" => 1419
"Ancho" => 2508
"Tamanyo" => 242277
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0010"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">These sagittal (A) and coronal (B) CT angiogram images show normal posterior circulation with 50% stenosis of the left V4 segment and no identifiable aneurysm, arteriovenous malformation, or dural arteriovenous fistula.</p>"
]
]
]
"bibliografia" => array:2 [
"titulo" => "References"
"seccion" => array:1 [
0 => array:2 [
"identificador" => "bibs0005"
"bibliografiaReferencia" => array:6 [
0 => array:3 [
"identificador" => "bib0005"
"etiqueta" => "1"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Insights on the hydrodynamics of chiari malformation"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:6 [
0 => "C. Capel"
1 => "P. Padovani"
2 => "P.H. Launois"
3 => "S. Metanbou"
4 => "O. Baledent"
5 => "J. Peltier"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3390/jcm11185343"
"Revista" => array:4 [
"tituloSerie" => "J Clin Med"
"fecha" => "2022"
"volumen" => "11"
"numero" => "18"
]
]
]
]
]
]
1 => array:3 [
"identificador" => "bib0010"
"etiqueta" => "2"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Chiari I malformation with acute neurological deficit after craniocervical trauma: case report, imaging, and anatomic considerations"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:2 [
0 => "J.A. Woodward"
1 => "D.E. Adler"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.4103/sni.sni_304_16"
"Revista" => array:4 [
"tituloSerie" => "Surg Neurol Int"
"fecha" => "2018"
"volumen" => "9"
"paginaInicial" => "88"
]
]
]
]
]
]
2 => array:3 [
"identificador" => "bib0015"
"etiqueta" => "3"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Association of a distal intradural-extracranial posterior inferior cerebellar artery aneurysm with chiari type I malformation: case report"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:6 [
0 => "J.R. Mascitelli"
1 => "S. Ben-Haim"
2 => "S. Paramasivam"
3 => "H.K. Zarzour"
4 => "R.J. Rothrock"
5 => "J.B. Bederson"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1227/NEU.0000000000000870"
"Revista" => array:7 [
"tituloSerie" => "Neurosurgery"
"fecha" => "2015"
"volumen" => "77"
"numero" => "4"
"paginaInicial" => "E660"
"paginaFinal" => "665"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/26308644"
"web" => "Medline"
]
]
]
]
]
]
]
]
3 => array:3 [
"identificador" => "bib0020"
"etiqueta" => "4"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Angiogram-negative subarachnoid hemorrhage: relationship between bleeding pattern and clinical outcome"
"autores" => array:1 [
0 => array:2 [
"etal" => true
"autores" => array:3 [
0 => "N. Lin"
1 => "G. Zenonos"
2 => "A.H. Kim"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s12028-012-9680-6"
"Revista" => array:7 [
"tituloSerie" => "Neurocrit Care"
"fecha" => "2012"
"volumen" => "16"
"numero" => "3"
"paginaInicial" => "389"
"paginaFinal" => "398"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/22350856"
"web" => "Medline"
]
]
]
]
]
]
]
]
4 => array:3 [
"identificador" => "bib0025"
"etiqueta" => "5"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Idiopathic subarachnoid hemorrhage and venous drainage: are they related?"
"autores" => array:1 [
0 => array:2 [
"etal" => true
"autores" => array:3 [
0 => "J.F. Alen"
1 => "A. Lagares"
2 => "J. Campollo"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1227/01.NEU.0000335777.14055.71"
"Revista" => array:7 [
"tituloSerie" => "Neurosurgery"
"fecha" => "2008"
"volumen" => "63"
"numero" => "6"
"paginaInicial" => "1106"
"paginaFinal" => "1111"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/19057322"
"web" => "Medline"
]
]
]
]
]
]
]
]
5 => array:3 [
"identificador" => "bib0030"
"etiqueta" => "6"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Neurosurgical management of patients with Ehlers-Danlos syndrome: a descriptive case series"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:4 [
0 => "M.B. Rock"
1 => "D.Y. Zhao"
2 => "D.R. Felbaum"
3 => "F.A. Sandhu"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.4103/jcvjs.jcvjs_127_22"
"Revista" => array:7 [
"tituloSerie" => "J Craniovertebr Junction Spine"
"fecha" => "2023"
"volumen" => "14"
"numero" => "1"
"paginaInicial" => "24"
"paginaFinal" => "34"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/37213579"
"web" => "Medline"
]
]
]
]
]
]
]
]
]
]
]
]
]
"idiomaDefecto" => "en"
"url" => "/25298496/unassign/S2529849624000340/v1_202407220410/en/main.assets"
"Apartado" => null
"PDF" => "https://static.elsevier.es/multimedia/25298496/unassign/S2529849624000340/v1_202407220410/en/main.pdf?idApp=UINPBA00004B&text.app=https://revistaneurocirugia.com/"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849624000340?idApp=UINPBA00004B"
]