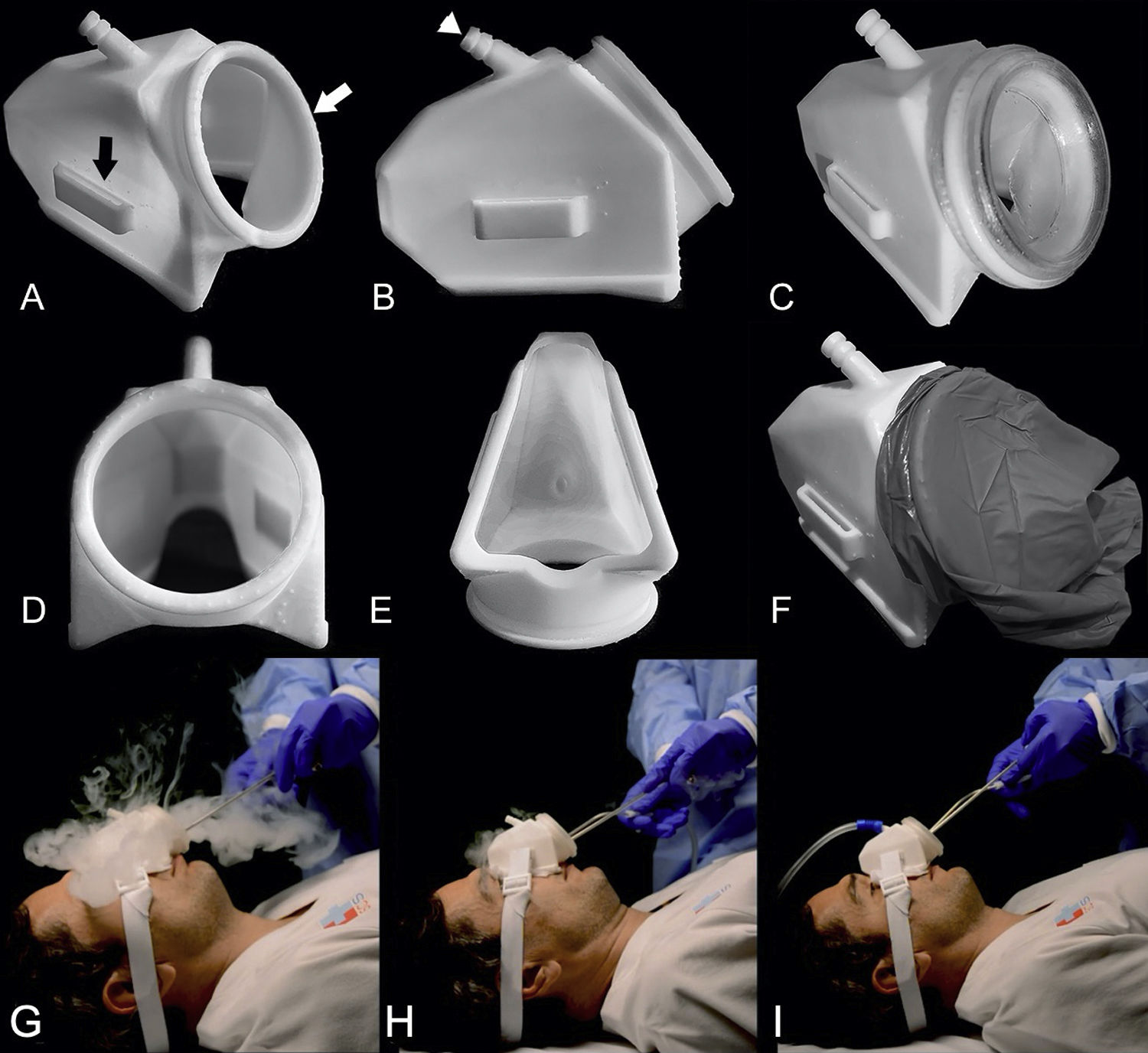
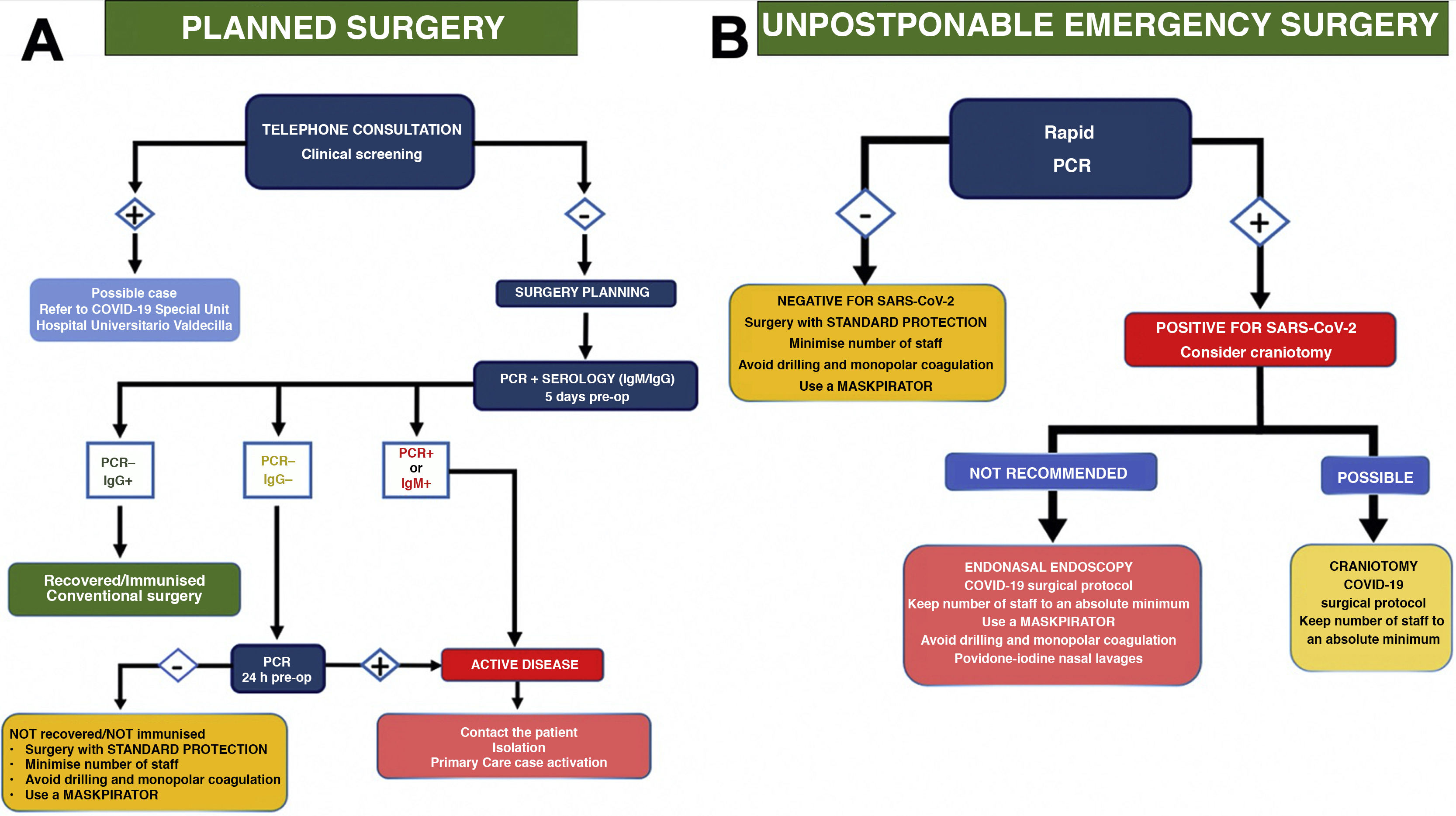
Current SARS-CoV-2 coronavirus pandemic is challenging medical and surgical activities. Specifically, within neurosurgery, endoscopic endonasal approaches pose a high risk of contagion for healthcare personnel involved in it. Initially, the recommendation was to avoid such surgeries. However, the pandemic has dragged on and new solutions must be proposed to continue carrying out these approaches safely. Given the lack of established protocols, we propose the following one, which concisely establishes the measures to be taken in both urgent and scheduled surgery. In addition, a new protection-aspiration device (Maskpirator) is described.
La actual pandemia por coronavirus SARS-CoV-2 está planteando una serie de desafíos al modo en que ejercemos la actividad médica y quirúrgica. En concreto, dentro de la neurocirugía se ha visto que los abordajes endoscópicos endonasales suponen un elevado riesgo de contagio para el personal sanitario que interviene en la misma, por lo que, inicialmente, la recomendación fue evitar dichas cirugías. Dado que la pandemia se ha extendido en el tiempo y desconocemos cuándo se podrá controlar, se deben proponer nuevas soluciones para continuar con la realización de dichos abordajes de manera segura. Ante la falta de protocolos establecidos, planteamos el siguiente, en el que se establecen, de modo conciso, las medidas a tomar tanto en cirugía urgente como programada, además de la descripción de un nuevo dispositivo de protección-aspirado (Maskpirator).
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.