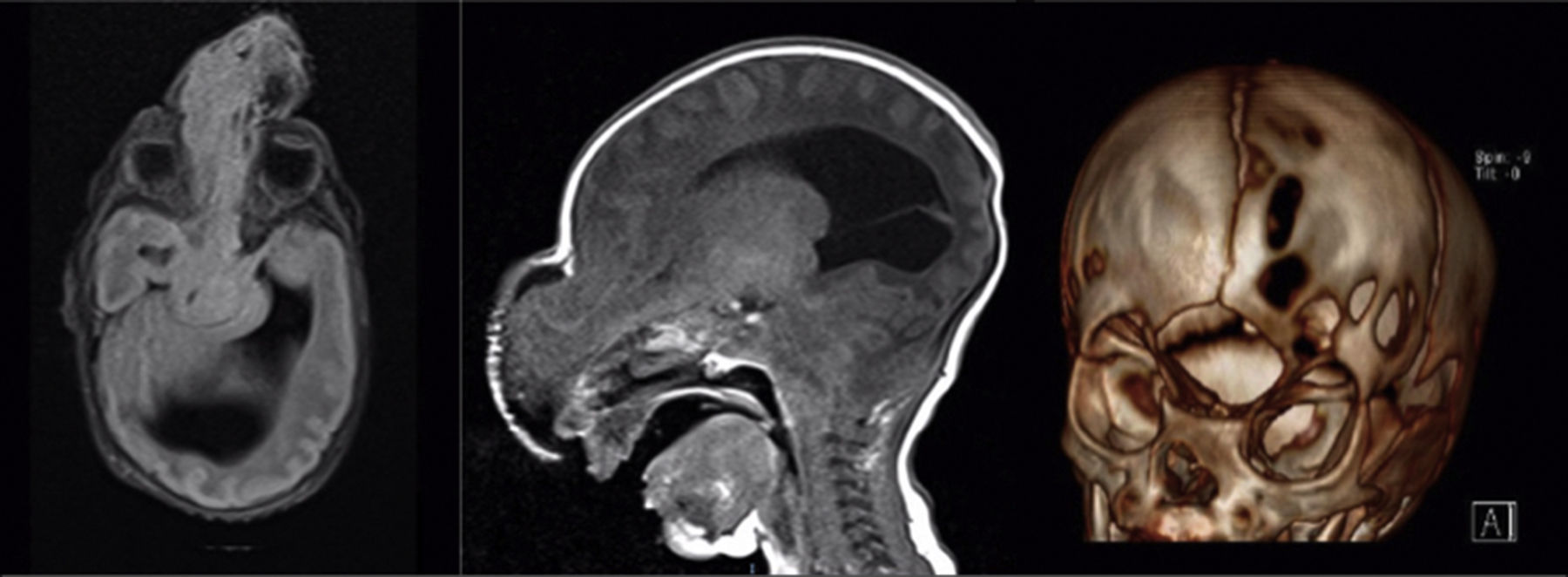
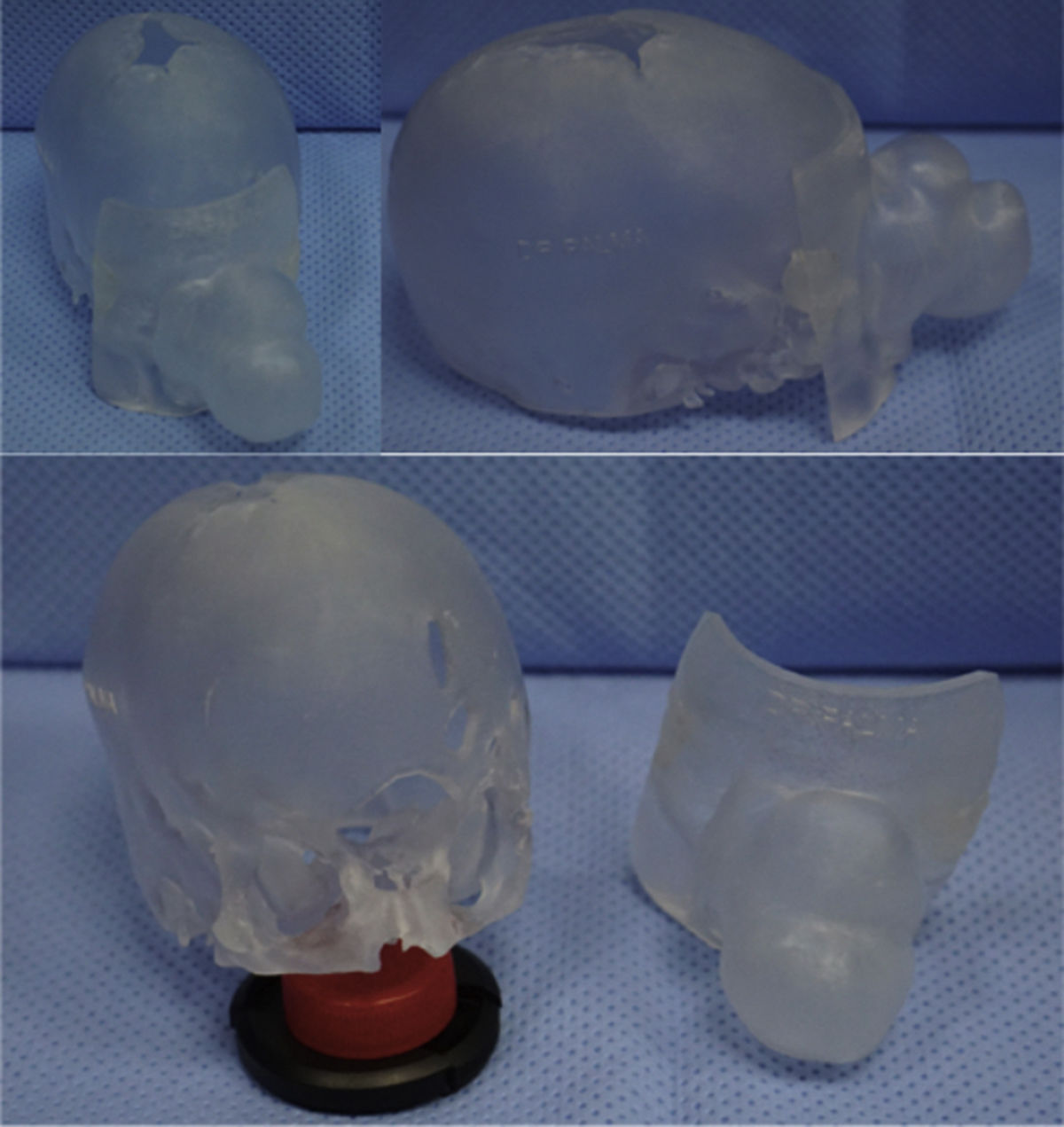
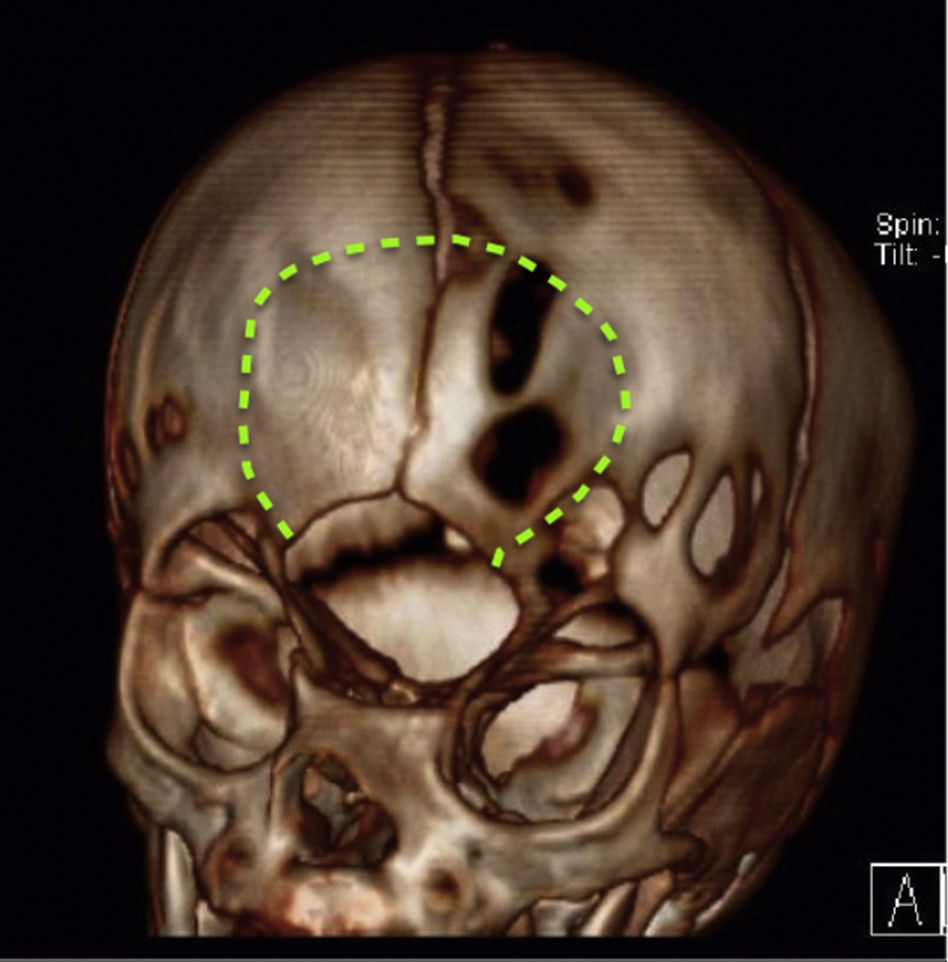
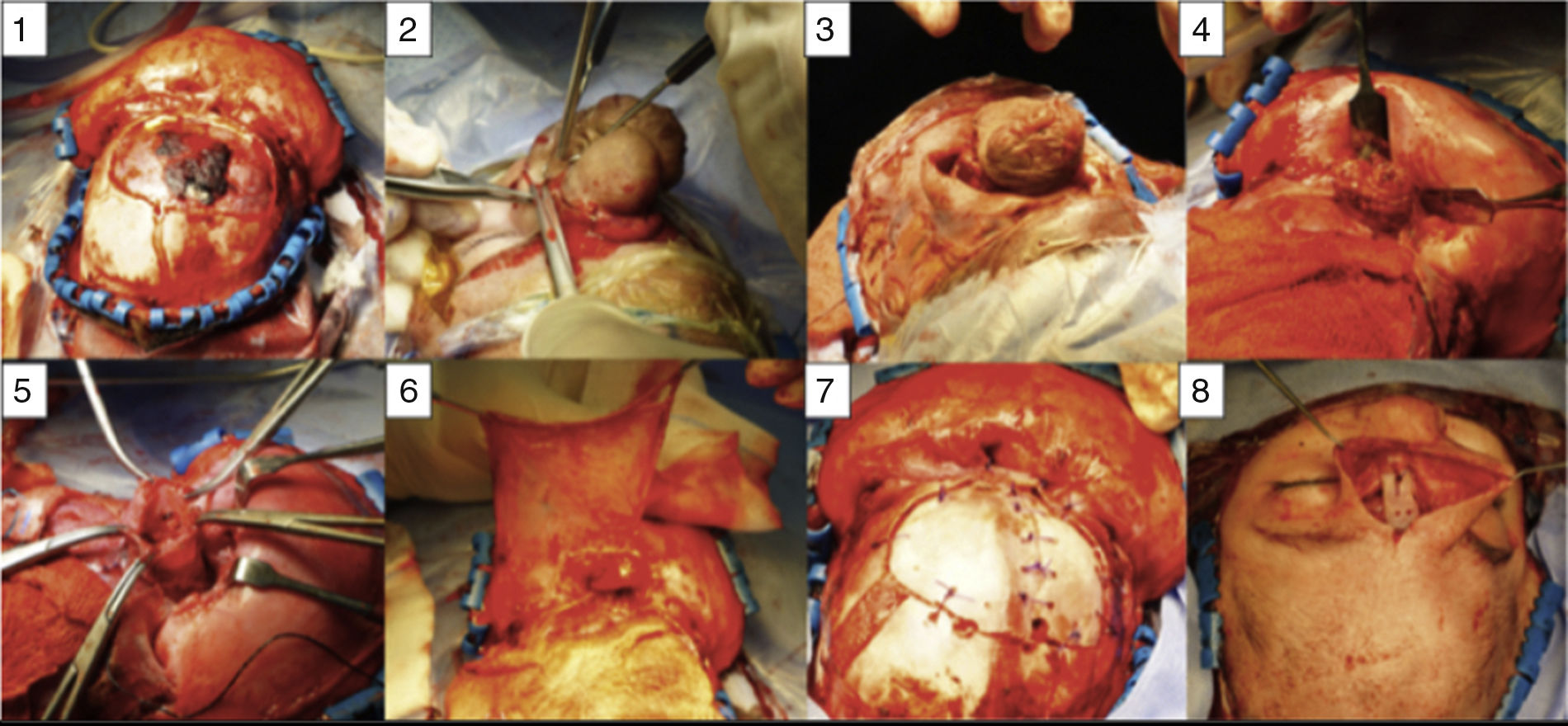
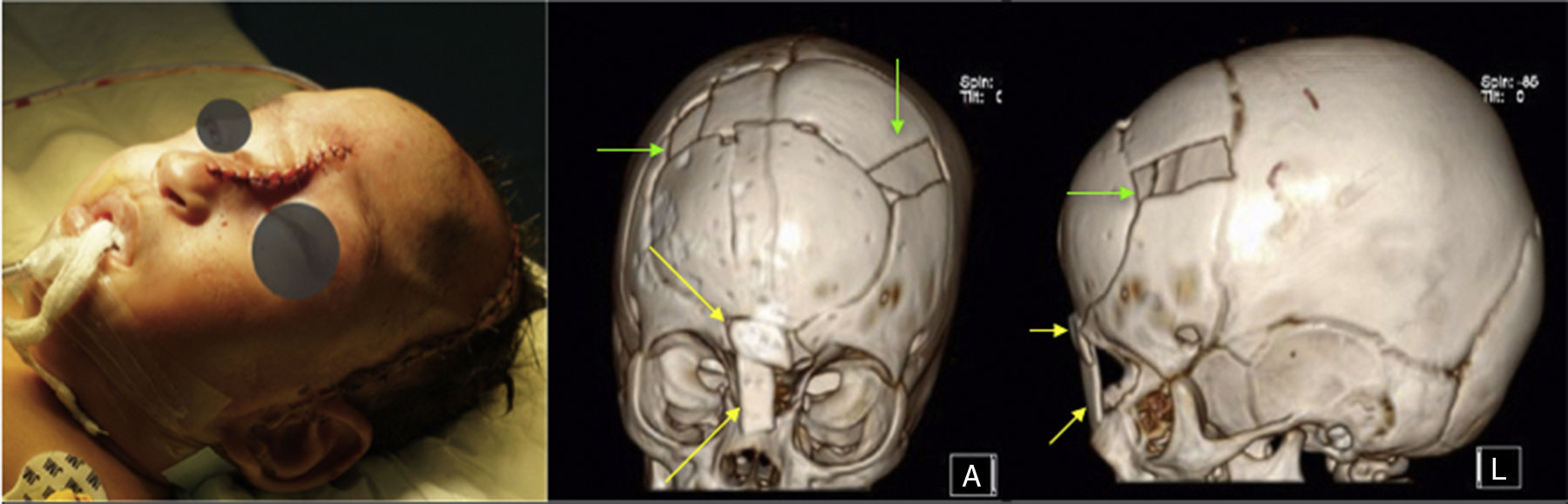
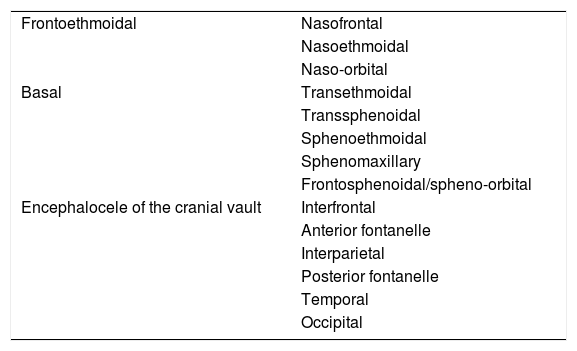
Encephaloceles are uncommon in western countries and most cases are located in the occipital bone. Frontal encephaloceles may involve the ethmoid bone, nasal bones and/or the orbits. Surgical repair is complex and usually requires a multidisciplinary approach. The goal of the surgery is to reconstruct the normal anatomy, to achieve a good cosmetic repair and to avoid a cerebrospinal fluid leak. We present a case of a patient with a large congenital frontoethmoidal encephalocele. Autologous calvarian bone grafts were used to repair of encephalocele defect and for the reconstruction of the frontonasal area. The defect closure and the cosmetic result were satisfactory, and the only complication detected was the infection of a previously performed ventriculoperitoneal shunt. A description of the technique and a review of the literature are presented.
Los encefaloceles son infrecuentes en los países occidentales y su localización más frecuente es occipital. Los encefaloceles frontales pueden afectar hueso etmoidal, frontal y/o órbitas. La reparación quirúrgica es compleja y habitualmente precisa de un abordaje multidisciplinar. El objetivo de la cirugía es reconstruir la anatomía del paciente con un buen resultado estético, y evitar la fístula de líquido cefalorraquídeo. Se presenta un caso de un gran encefalocele frontoetmoidal. El encefalocele fue reparado y la reconstrucción ósea se realizó con hueso autólogo de la capota craneal. El cierre y el resultado cosmético fueron buenos y la única complicación fue una infección posquirúrgica. Se describe la técnica y se revisa la literatura publicada al respecto.
Artículo

Si es la primera vez que accede a la web puede obtener sus claves de acceso poniéndose en contacto con Elsevier España en suscripciones@elsevier.com o a través de su teléfono de Atención al Cliente 902 88 87 40 si llama desde territorio español o del +34 932 418 800 (de 9 a 18h., GMT + 1) si lo hace desde el extranjero.
Si ya tiene sus datos de acceso, clique aquí.
Si olvidó su clave de acceso puede recuperarla clicando aquí y seleccionando la opción "He olvidado mi contraseña".