Chronic subdural hematoma is a frequent neurosurgical illness, and current treatment options mostly include subdural trepanation and drainage alone, as well as middle meningeal artery embolization in conjunction with subdural trepanation and drainage. However, there is currently a lack of extensive study and data support for comparing the clinical results of the two surgical treatment techniques.
ObjectiveThe goal of this study is to compare the clinical effects of middle meningeal artery embolization combined with subdural trepanation and drainage versus simple subdural trepanation and drainage in the treatment of chronic subdural hematoma, in order to provide a reliable foundation for clinical selection of appropriate surgical treatment methods.
MethodsThis study included 71 patients with chronic subdural hematoma, who were divided into two groups according to the procedure: observation group (n = 25) and control group (n = 46). The control group received only basic subdural drilling and drainage.
ConclusionsThis study found that MMA embolization combined with subdural trepanation and drainage provides a greater therapeutic benefit in the treatment of chronic subdural hematoma. The observation group outperformed the control group in terms of postoperative CT results, Barthel index, and clinical effect, as well as operating time. Furthermore, the observation group's complications and recurrence rate were much lower than the control group’s.
El hematoma subdural crónico es una enfermedad neuroquirúrgica frecuente.Las opciones de tratamiento actuales incluyen principalmente el drenaje de perforación subdural solo, así como la embolización de la arteria media meningeal combinada con el drenaje de perforación subdural.Sin embargo, actualmente hay una falta de estudio exhaustivo y apoyo de datos para comparar los resultados clínicos de las dos técnicas de tratamiento quirúrgico.
ObjetivoComparar los efectos clínicos de la embolización de la arteria media meningeal combinada con el drenaje de perforación subdural frente al drenaje de perforación subdural solo en el tratamiento del hematoma subdural crónico.Proporcione una base confiable para la selección clínica de métodos de tratamiento quirúrgico adecuados.
MétodosEste estudio incluyó 71 pacientes con hematoma subdural crónico.Los sujetos de investigación fueron divididos en dos grupos según los métodos quirúrgicos:grupo de observación (n = 25) y grupo de control (n = 46).El grupo de control solo recibió drenaje de perforación subdural.
ConclusionesEste estudio encontró que la embolización de la arteria media meningeal combinada con el drenaje de perforación subdural ofrece un mayor beneficio terapéutico en el tratamiento del hematoma subdural crónico.El grupo de observación superó el grupo de control en cuanto a los resultados de la TC postoperatoria, el índice de Barthel y el efecto clínico, así como el tiempo de operación.Además, las complicaciones y la tasa de recurrencia del grupo de observación fueron mucho más bajas que las del grupo de control.
Chronic subdural hematoma (CSDH) therapy approaches have been consistently explored and improved in recent years. The combination of Middle meningeal artery embolization (MMA) and subdural trepanation and drainage is a new therapy approach. It has received a lot of attention in clinical practice when compared to the traditional basic subdural trepanation and drainage.1–3 Chronic subdural hematoma is a common neurosurgical emergency defined by the progressive development of chronic subdural hematoma after head trauma.4,5 Patients frequently experience headaches, nausea, vomiting, and other symptoms, which can progress to neurological dysfunction in severe cases. Early detection and prompt treatment of chronic subdural hematomas are critical for patient rehabilitation.6,7 Simple subdural trepanation and drainage8,9 can reduce intracranial pressure and relieve symptoms by drilling on the head and draining the hematoma are the most common traditional therapeutic approaches. However, this approach has numerous drawbacks, including significant surgical stress and a high risk of bleeding.10,11 Middle meningeal artery embolization (MMA) combined with subdural trepanation and drainage as a new treatment method,12,13 the embolic material is inserted into the arterial vessel through interventional means to block the blood supply, reducing the risk of bleeding. The hematoma can be cleared more efficiently when paired with subdural drilling and drainage. A meta-analysis of the literature revealed that MMA embolization has a lower rate of postoperative recurrence compared to subdural perforation drainage, with no difference in postoperative complication rates.14 However, rigorous study on the therapeutic benefit of MMA Embolization combined with subdural perforation drainage in the treatment of chronic subdural hematoma is still lacking. As a result, the goal of this study is to compare and contrast the therapeutic effects of middle meningeal artery embolization (MMA) combined with subdural trepanation and drainage and simple subdural trepanation and drainage in order to provide a more scientific and accurate treatment plan for clinical practice. We anticipate that the growth of this study will result in a more thorough understanding of the treatment of chronic subdural hematoma, a reference for clinicians when selecting treatment approaches, and a better contribution to patient rehabilitation.
Materials and methodsGeneral informationThis was a single-center retrospective continuous clinical cohort research. The research subjects were 71 patients with chronic subdural hematoma diagnosed and treated at Chengdu University's Affiliated Hospital from January 2022 to October 2023. The patients were separated into two groups based on the differences in treatment modalities. The control group (n = 25) had trepanation and drainage along with middle dural artery embolization. All patients who took part in this study did so willingly and gave informed permission. Our hospital's Medical Ethics Committee approved this investigation.We confirmed that all methods have been performed in accordance with the Declaration of Helsinki. Inclusion and exclusion criteria
Inclusion criteria: ① all patients met the diagnostic criteria of chronic subdural hematoma (Chinese Guidelines for craniocerebral trauma Surgery); ② all patients were diagnosed by CT or MRI; ③ no surgical contraindications15; ④ age > 18 years old; ⑤ unilateral hematoma. Exclusion criteria: ① patients with serious heart, kidney, liver and other important organ diseases; ② coagulopathy; ③ patients with incomplete follow-up data; ④ death occurred.
Research methodsControl groupThe operation is performed by subdural perforation drainage. The anesthesia method is local anesthesia; if the patient is unable to cooperate with local anesthesia, intravenous anesthesia or general anesthesia with tracheal intubation is used.The patient was placed in the supine position and the puncture placement point was localised by CT. The middle and posterior 1/3 of the largest level of the haematoma and the scalp were taken as the puncture point. Avoid important blood vessels and functional areas during puncture. A 2−3 cm incision was made at the puncture location, followed by a cut to the skull, the periosteum was peeled off, a drilling device (1–1.5 cm in diameter) was used to drill through the skull, electrocoagulation around the dura mater, and the bleeding was completely stopped. The dura mater was sliced in a "cross" shape, and a No. 10 silicone tubing was introduced to access the subdural space, resulting in bloody drainage. In the same manner, the drainage tube was rinsed to the temporoparietal and occipital areas. Finally, the surgical incision was sutured layer by layer, and the drainage tube and drainage device were secured. The remaining condition of subdural hematoma was examined by CT scan after the procedure. On the third day following the operation, the drainage tube was withdrawn when there was no bleeding or the hematoma was less than 10 ml. If there is rebleeding or residual hematoma, the indwelling time of the drainage tube can be reduced to less than one week. Changes in vital signs of patients were routinely monitored after operation, and symptomatic treatment such as conventional anti-infection treatment was performed.
Observation groupThe patients were supine on the angiography table after local anesthetic (intravenous anesthesia or general anesthesia for tracheal intubation if they were unable to work together). The puncture site was routinely cleaned and toweled. Following success, the Seldinger technique was applied, an 8 F sheath was placed, and systemic heparin (40 mg bolus injection) was administered. Through a 0.035 in. guide wire +5F 125 cm angiography guide, the guide was superselected to the external carotid artery. By microguide wire, the Marathon and Apollo microcatheters were superselected to the frontal, parietal, and occipital branches of the middle meningeal artery, respectively. Following microcatheter hand push angiography confirmation, Onyx was progressively injected into the branches in turn for a total of 1.8 ml. After satisfactory angiography and embolization, the puncture point was occluded by vascular occluder to stop bleeding. Continue drilling and drainage as in Section “Control group”.
Indicators of observationBaseline characteristics (age, gender, history of hypertension, diabetes, coronary heart disease, myocardial infarction, cerebral infarction, asthma, cancer, etc.), use of anticoagulant drugs (aspirin, warfarin, etc.), history of head trauma), clinical operation indicators (intraoperative blood loss, operation time, drainage volume, drainage time, length of hospital stay), clinical effect, stroke mRs Score, neurological deficit score (Markwalder). Chronic subdural hematoma progression and recurrence16 was defined as new high-density hematoma, increased hematoma thickness, and the presentation or exacerbation of clinical symptoms. The hematoma thickness: on CT image, the diameter from the inner plate of skull to the place with the largest hematoma width on the brain surface (unit: mm).
Clinical effect17The clinical symptoms and signs of the patients were greatly reduced, and the subdural hematoma almost completely gone. Effective: the patients' clinical symptoms and signs improved, and the subdural hematoma was reduced. Ineffective: none of the following indicators were met, and they even tended to worsen. Total effective rate = (marked effective + effective)/total cases 100%.
The CT was evaluated periodically after operation, and the imaging outcomes at 3 months after operation, Markwalder Score at 1 week after operation and mRs Score at 3 months after operation were recordedPostoperative CT results: cured, CT examination showed that there was no hematoma. CT examination showed that the clearance rate was more than 90%. CT examination showed that the clearance rate was 75%–90%. Effective, 60%–75%; ineffective, less than 60%.
Barthel index18: cure, symptoms disappear completely; Obviously improved, symptoms basically disappeared, slight neurological dysfunction; The symptoms were partially improved, and the patient was basically self-care. The symptoms were slightly improved, and the patient could live independently with help. Ineffective, completely unable to take care of themselves.
mRs Score19: 0: no symptoms; Score 1: symptomatic but without significant neurological impairment, able to perform all daily activities; Score 2: mild disability, unable to complete all pre-illness activities, but able to live independently; Score 3: moderate disability requiring partial assistance but able to walk independently; Score 4: moderate to severe disability, unable to walk independently, requiring partial care for daily life; Score 5: severe disability, bedridden, incontinence, total dependence on others for daily life; Score 6: Death. The mRS Score of 0–2 was defined as good prognosis, and the mRS Score of 3–6 was defined as poor prognosis.
Statistical methodsThe data was analyzed using SPSS25.0 statistical software. Mean standard deviation was used to communicate measurement data, while count (%) was used to convey categorical variables. The median (M), interquartile range (Q), and rank sum test were utilized when the measurement data did not follow the normal distribution. The important indicators of comprehensive collaborative scheduling and quantitative scoring assessment were analyzed using descriptive statistical analysis and one-way analysis of variance. The Chi square test was used to assess the utility of thorough collaborative scheduling and quantitative scoring in increasing operating room efficiency and patient, surgeon, and nurse satisfaction. P < 0.05 was regarded as statistically significant.
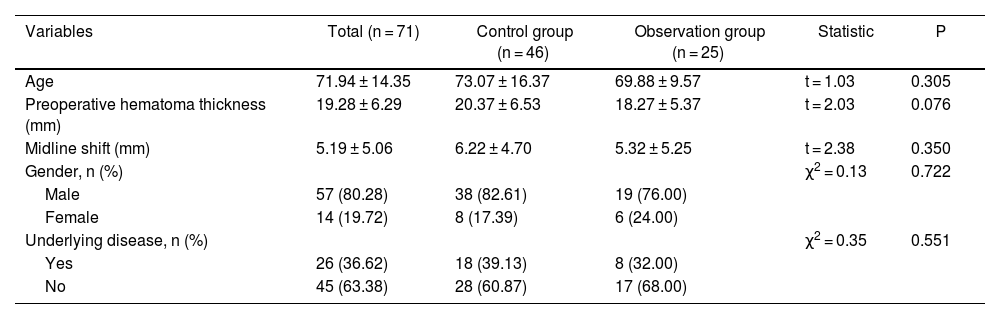
ResultsComparison of general data between the two groupsThere were 38 males and 8 females in the control group. The average age was (73.07 ± 16.37) years (range, 27–96 years). There were 19 males and 6 females in the observation group. The mean age was (69.88 ± 9.57) years (range, 52–95 years). There were no significant differences in age, gender, underlying disease, history of craniocerebral trauma, preoperative hematoma thickness and midline shift between the two groups (P < 0.05), which were comparable, the specific results are shown in Table 1.
Comparison of general information between the two groups.
| Variables | Total (n = 71) | Control group (n = 46) | Observation group (n = 25) | Statistic | P |
|---|---|---|---|---|---|
| Age | 71.94 ± 14.35 | 73.07 ± 16.37 | 69.88 ± 9.57 | t = 1.03 | 0.305 |
| Preoperative hematoma thickness (mm) | 19.28 ± 6.29 | 20.37 ± 6.53 | 18.27 ± 5.37 | t = 2.03 | 0.076 |
| Midline shift (mm) | 5.19 ± 5.06 | 6.22 ± 4.70 | 5.32 ± 5.25 | t = 2.38 | 0.350 |
| Gender, n (%) | χ2 = 0.13 | 0.722 | |||
| Male | 57 (80.28) | 38 (82.61) | 19 (76.00) | ||
| Female | 14 (19.72) | 8 (17.39) | 6 (24.00) | ||
| Underlying disease, n (%) | χ2 = 0.35 | 0.551 | |||
| Yes | 26 (36.62) | 18 (39.13) | 8 (32.00) | ||
| No | 45 (63.38) | 28 (60.87) | 17 (68.00) |
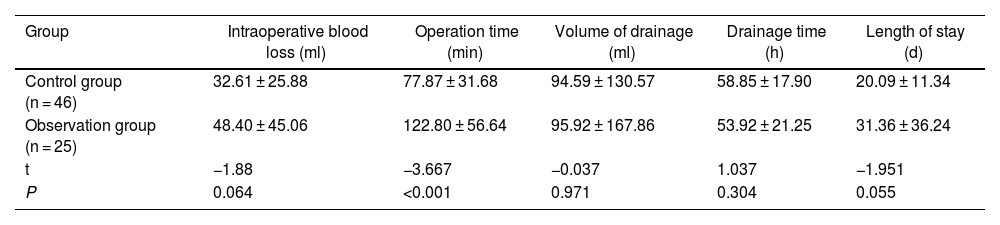
The observation group's operation time was longer than the control group's, while the drainage time and hospitalization time were shorter. The intraoperative blood loss and volume of drainage were lower in the observation group than in the control group (P < 0.05), and the specific data are provided in Table 2.
Comparison of clinical surgical indexes between the two groups.
| Group | Intraoperative blood loss (ml) | Operation time (min) | Volume of drainage (ml) | Drainage time (h) | Length of stay (d) |
|---|---|---|---|---|---|
| Control group (n = 46) | 32.61 ± 25.88 | 77.87 ± 31.68 | 94.59 ± 130.57 | 58.85 ± 17.90 | 20.09 ± 11.34 |
| Observation group (n = 25) | 48.40 ± 45.06 | 122.80 ± 56.64 | 95.92 ± 167.86 | 53.92 ± 21.25 | 31.36 ± 36.24 |
| t | −1.88 | −3.667 | −0.037 | 1.037 | −1.951 |
| P | 0.064 | <0.001 | 0.971 | 0.304 | 0.055 |
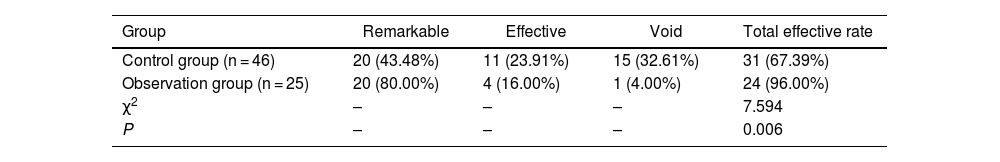
The total effective rate of the observation group was higher than that of the control group, the total effective rate of the observation group was 67.39%, and the total effective rate of the control group was 96.00% (P < 0.05). The specific results are shown in Table 3.
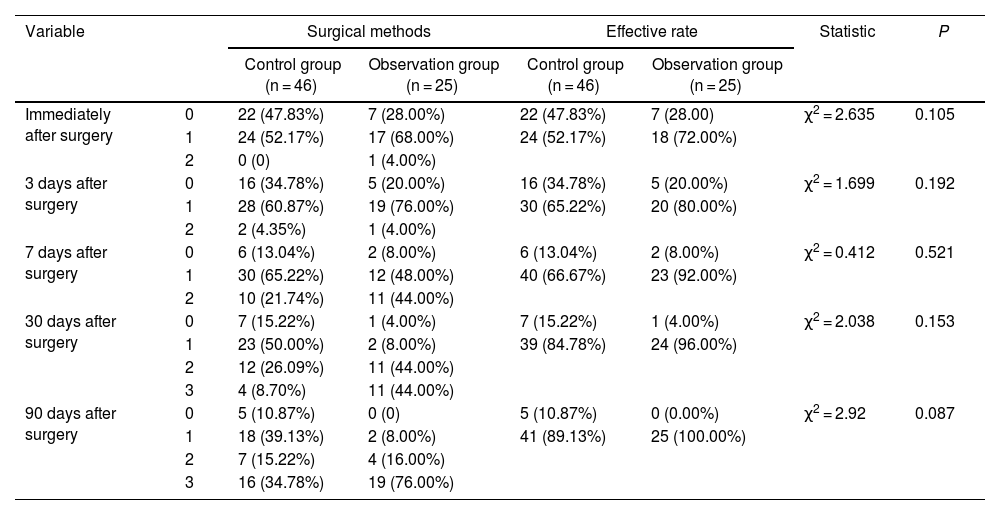
Comparison of CT results immediately, 3d, 7d, 30d and 90d after operation between the two groupsBy comparing we can find that efficient observation group were higher than the same period in different periods in control group (P < 0.05), the observation group 90 days after operation efficiency is as high as 100%. Specific results are shown in Table 4.
Comparison of CT results between the two groups (%).
| Variable | Surgical methods | Effective rate | Statistic | P | |||
|---|---|---|---|---|---|---|---|
| Control group (n = 46) | Observation group (n = 25) | Control group (n = 46) | Observation group (n = 25) | ||||
| Immediately after surgery | 0 | 22 (47.83%) | 7 (28.00%) | 22 (47.83%) | 7 (28.00) | χ2 = 2.635 | 0.105 |
| 1 | 24 (52.17%) | 17 (68.00%) | 24 (52.17%) | 18 (72.00%) | |||
| 2 | 0 (0) | 1 (4.00%) | |||||
| 3 days after surgery | 0 | 16 (34.78%) | 5 (20.00%) | 16 (34.78%) | 5 (20.00%) | χ2 = 1.699 | 0.192 |
| 1 | 28 (60.87%) | 19 (76.00%) | 30 (65.22%) | 20 (80.00%) | |||
| 2 | 2 (4.35%) | 1 (4.00%) | |||||
| 7 days after surgery | 0 | 6 (13.04%) | 2 (8.00%) | 6 (13.04%) | 2 (8.00%) | χ2 = 0.412 | 0.521 |
| 1 | 30 (65.22%) | 12 (48.00%) | 40 (66.67%) | 23 (92.00%) | |||
| 2 | 10 (21.74%) | 11 (44.00%) | |||||
| 30 days after surgery | 0 | 7 (15.22%) | 1 (4.00%) | 7 (15.22%) | 1 (4.00%) | χ2 = 2.038 | 0.153 |
| 1 | 23 (50.00%) | 2 (8.00%) | 39 (84.78%) | 24 (96.00%) | |||
| 2 | 12 (26.09%) | 11 (44.00%) | |||||
| 3 | 4 (8.70%) | 11 (44.00%) | |||||
| 90 days after surgery | 0 | 5 (10.87%) | 0 (0) | 5 (10.87%) | 0 (0.00%) | χ2 = 2.92 | 0.087 |
| 1 | 18 (39.13%) | 2 (8.00%) | 41 (89.13%) | 25 (100.00%) | |||
| 2 | 7 (15.22%) | 4 (16.00%) | |||||
| 3 | 16 (34.78%) | 19 (76.00%) | |||||
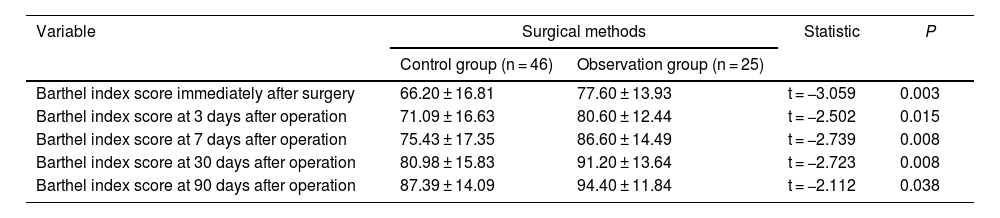
Observation group Barthel index in different periods were compared with the control group (P < 0.05), the specific results are shown in Table 5.
Comparison of Barthel index results between the two groups.
| Variable | Surgical methods | Statistic | P | |
|---|---|---|---|---|
| Control group (n = 46) | Observation group (n = 25) | |||
| Barthel index score immediately after surgery | 66.20 ± 16.81 | 77.60 ± 13.93 | t = −3.059 | 0.003 |
| Barthel index score at 3 days after operation | 71.09 ± 16.63 | 80.60 ± 12.44 | t = −2.502 | 0.015 |
| Barthel index score at 7 days after operation | 75.43 ± 17.35 | 86.60 ± 14.49 | t = −2.739 | 0.008 |
| Barthel index score at 30 days after operation | 80.98 ± 15.83 | 91.20 ± 13.64 | t = −2.723 | 0.008 |
| Barthel index score at 90 days after operation | 87.39 ± 14.09 | 94.40 ± 11.84 | t = −2.112 | 0.038 |
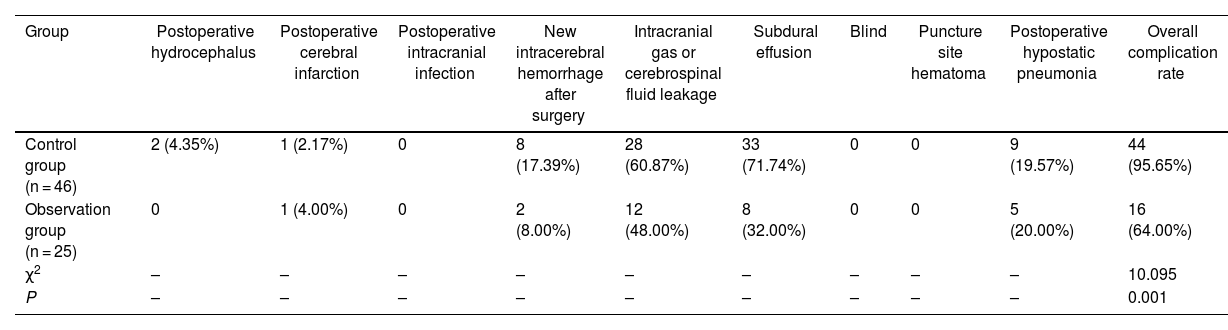
The incidence of complications in the observation group was lower than that in the control group (P < 0.05). The postoperative hematoma thickness, incidence of subdural effusion and mRs Score of the patients were followed up for 3 months after surgery. The incidence of hematoma and subdural effusion and mRs Score in the observation group were lower than those in the control group: the specific results are shown in Table 6.
Comparison of postoperative complications between the two groups.
| Group | Postoperative hydrocephalus | Postoperative cerebral infarction | Postoperative intracranial infection | New intracerebral hemorrhage after surgery | Intracranial gas or cerebrospinal fluid leakage | Subdural effusion | Blind | Puncture site hematoma | Postoperative hypostatic pneumonia | Overall complication rate |
|---|---|---|---|---|---|---|---|---|---|---|
| Control group (n = 46) | 2 (4.35%) | 1 (2.17%) | 0 | 8 (17.39%) | 28 (60.87%) | 33 (71.74%) | 0 | 0 | 9 (19.57%) | 44 (95.65%) |
| Observation group (n = 25) | 0 | 1 (4.00%) | 0 | 2 (8.00%) | 12 (48.00%) | 8 (32.00%) | 0 | 0 | 5 (20.00%) | 16 (64.00%) |
| χ2 | – | – | – | – | – | – | – | – | – | 10.095 |
| P | – | – | – | – | – | – | – | – | – | 0.001 |
After 6 months of follow-up, the recurrence rate of the observation group was 0 (0/25), which was lower than 39.13% (18/46) of the control group, and the difference was statistically significant (χ2 = 13.105, P < 0.001).
DiscussionChronic subdural hematoma (CSDH) is a frequent neurosurgical illness defined by hematoma accumulation between the dura mater and the pia mater. CSDH is typically caused by head trauma, brain contusion, vascular lesions, or hemorrhagic illness. Treatments for CSDH include middle meningeal artery embolization (MMA) in conjunction with subdural trepanation and drainage, as well as simple subdural trepanation and drainage. These two surgical procedures have distinct advantages and disadvantages, as well as differing short- and long-term clinical outcomes. MMA combined with subdural drilling and drainage is a relatively recent therapy procedure that limits blood supply by embolizing the arteries in the dura mater, limiting the creation of new blood vessels and the rate of hematoma recurrence. Subdural drilling and drainage, on the other hand, can successfully drain the blood and fluid in the hematoma and relieve the symptoms of increased intracranial pressure. In contrast, simple subdural perforation drainage is the traditional treatment.In this method, a drilling device is used to drill through the skull, the dura is incised with a ‘cross’ and a 10-gauge silicone hose is placed into the subdural space to drain the haematoma.This approach is straightforward and quick to employ, but because it cannot properly control the creation of new blood vessels, the hematoma recurrence rate is significant, necessitating numerous surgical treatments.
The results of this study showed that during the operation, the operation time of the observation group was significantly longer than that of the control group, which may be due to the increase in the operation time of middle meningeal artery embolization (MMA). However, compared with previous studies,20 we observed no statistically significant differences in drainage time and drainage volume between the observation group and the control group. In addition, the intraoperative blood loss and hospitalization time of the observation group were longer than those of the control group, which was consistent with the results of previous studies,21,22 but these differences did not reach statistical significance, and the specific reasons will be analyzed in the limitations of the article later.It should be highlighted that, while a longer procedure duration may increase surgical risk and patient discomfort, the differences we found may be related only to the increased MMA operation time and have no effect on the performance of other surgical measures. As a result, in actual clinical practice, an increase in operation duration may not have a substantial impact on patient recovery and prognosis. Overall, while the observation group showed some patterns that differed from the control group in several ways, these changes were not statistically significant. Further research with a larger sample size may be required to corroborate these findings and assess the real influence of surgery scheduling on patient recovery.
This study delves deeper into the clinical effect; the clinical effect of the observation group was clearly superior to that of the control group. Only 67.39% of the 46 patients in the control group received significant therapeutic response, but 96.00% of the 25 patients in the observation group did. The difference is statistically significant when compared to previous research, and our findings confirm the therapeutic effectiveness of middle meningeal artery embolization (MMA) joint draining.23 Furthermore, The observation group outperformed the control group in terms of CT results at the immediate postoperative period, days 3, 7, 30 and 90, as well as Barthel Index results, and these differences were statistically significant. The improvement of the CT results reflect the effectiveness of the operation, while the Barthel index used to assess the patient's quality of life. The quality of life in the observation group was significantly better than that in the control group at different time points after surgery, which further verified the advantages of middle meningeal artery embolization (MMA) combined with subdural drilling and drainage in improving the quality of life of patients.Finally, the findings of this study revealed that the observation group fared substantially better than the control group in terms of complications and recurrence rates, with statistically significant differences. This suggests that, when compared to pure subdural drilling drainage, middle meningeal artery embolization (MMA) subdural drilling drainage is more effective in minimising complications and recurrence rate. In comparison to the results always,21,24,25 our investigation adds to this conclusion.The reason for this analysis is that middle meningeal artery embolisation is a minimally invasive procedure designed to address the main pathological mechanisms involved in the formation and recurrence of chronic subdural haematomas, and can be used as an adjunctive treatment after subdural perforation drainage. Middle meningeal artery embolisation embolises the middle meningeal artery, persistently blocking the local blood supply and minimising blood leakage.
It is important to note that the conclusion of this study is based on the analysis of the existing literature and finishing, although the results have a certain reliability, but there are still some limitations. From the perspective of a retrospective study, firstly, the observation group was not paired with the control group in a 1:1 ratio, which may have led to potential baseline differences between the two groups. For example, the observation group may have had more severe disease or other unpredictable factors that may have had an effect on the treatment effect. Therefore, the results need to be interpreted with caution. Secondly, the preoperative hematoma thickness and midline deviation of the observation group were larger, which may indicate that the condition of the observation group was relatively more serious.Furthermore, in the selection of the study population, patients with bilateral haematomas, severe cardiac and renal diseases, and coagulation disorders were excluded. This may have introduced bias, resulting in the group of MMA Embolization combined with subdural perforation drainage being more likely to have a favourable outcome.In addition,the recurrence rate of the control group was 39.13% (18/46). However, nearly 40% of recurrences is very high. This may have been influenced by bias, for example, the patients in control group had more severe underlying diseases, which affected the patients' postoperative recovery and led to postoperative recurrence.Meanwhile, our study is single-centered with a relatively small sample size, therefore, there may be biases in the selection of research subjects.
This selective tendency is likely to skew research conclusions, and other possible intervention treatment effect factors on the observation group cannot be ruled out. As a result, when discussing the study's findings, this issue should be considered as it may create variance. Furthermore, this study is divided into fewer groups and is a single-center study, which limits the popularization and trustworthiness of the results. Small sample sizes may result in statistical underestimation, exposing the findings to random error. The single-center study, on the other hand, may have regional and institute-specific constraints. As a result, more large-scale investigations from many centers are required to validate and corroborate the findings of this study. Therefore, more high-quality, large-sample, multi-center prospective studies should be carried out in the future to further verify this finding and provide more reliable clinical guidance.
In conclusion, middle meningeal artery (MMA) embolisation combined with subdural perforation drainage demonstrated significant advantages in terms of surgical outcome, improvement in quality of life, and reduction in complications and recurrence rates. These findings will help to guide clinical practice and provide a better therapy alternative for patients. However, bigger sample sizes and longer follow-up investigations are required to demonstrate the stability and longevity of these findings. Furthermore, the treatment for chronic subdural hematoma should be dependent on the patient's individual condition, the severity of the disease, and the doctor's experience. Because each patient's situation is unique, the treatment approach should be tailored to them.
ConclusionsThis study demonstrates that middle meningeal artery embolisation (MMA) combined with subdural perforation drainage has better clinical outcomes in the treatment of CSDH. In addition to the lengthier operation time, the observation group outperformed the control group in terms of postoperative CT results, Barthel index, and clinical outcomes. Furthermore, the observation group had much reduced complications and recurrence rates than the control group. As a result, doctors may consider using middle meningeal artery embolization (MMA) in conjunction with subdural trepanation and drainage in the treatment of chronic subdural hematoma. This study offers a novel concept and point of reference for the treatment of chronic subdural hematoma.
CRediT authorship contribution statementWen Cheng participated in case collection; Jiangbin Wu and Quanlong Yang wrote the manuscript and raised idea; Quanlong Yang and Xiaodong Yuan revised the manuscript and raised critical editing. All authors have read and approved the manuscript.
Ethics statementWritten informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article. Approval number: PJ2023-058-03.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. If you need to ask us for the data of this study, please contact Wen Cheng, chengwen2002112@163.com.