The prognosis of one hemisphere malignant infarction creates doubt among neurosurgeons about decompressive hemicraniectomy indication. What results are achieved in the short to medium term? Are families satisfied with the surgery once the patient is at home? In the present study, we analyze our experience in this matter during the last thirteen years.
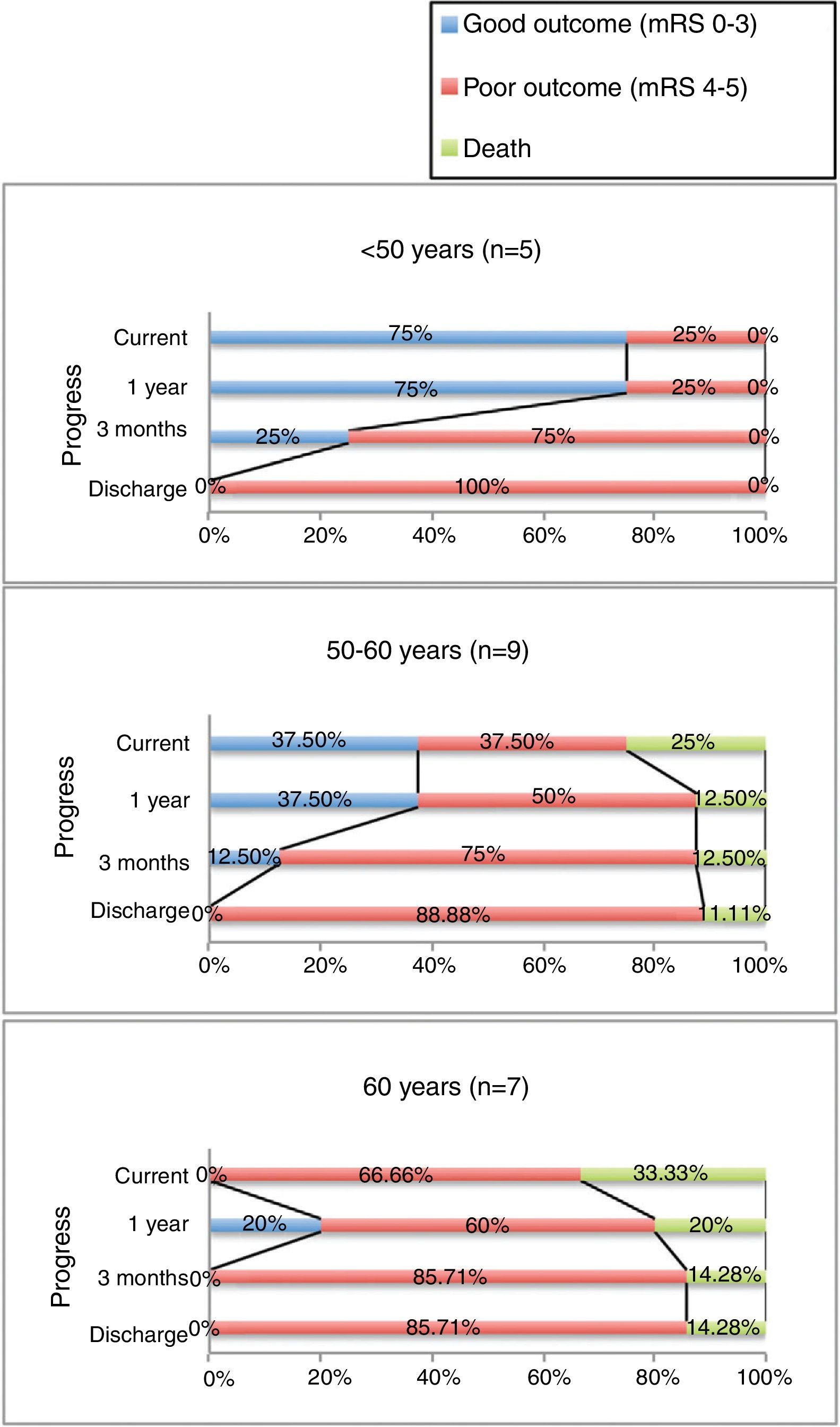
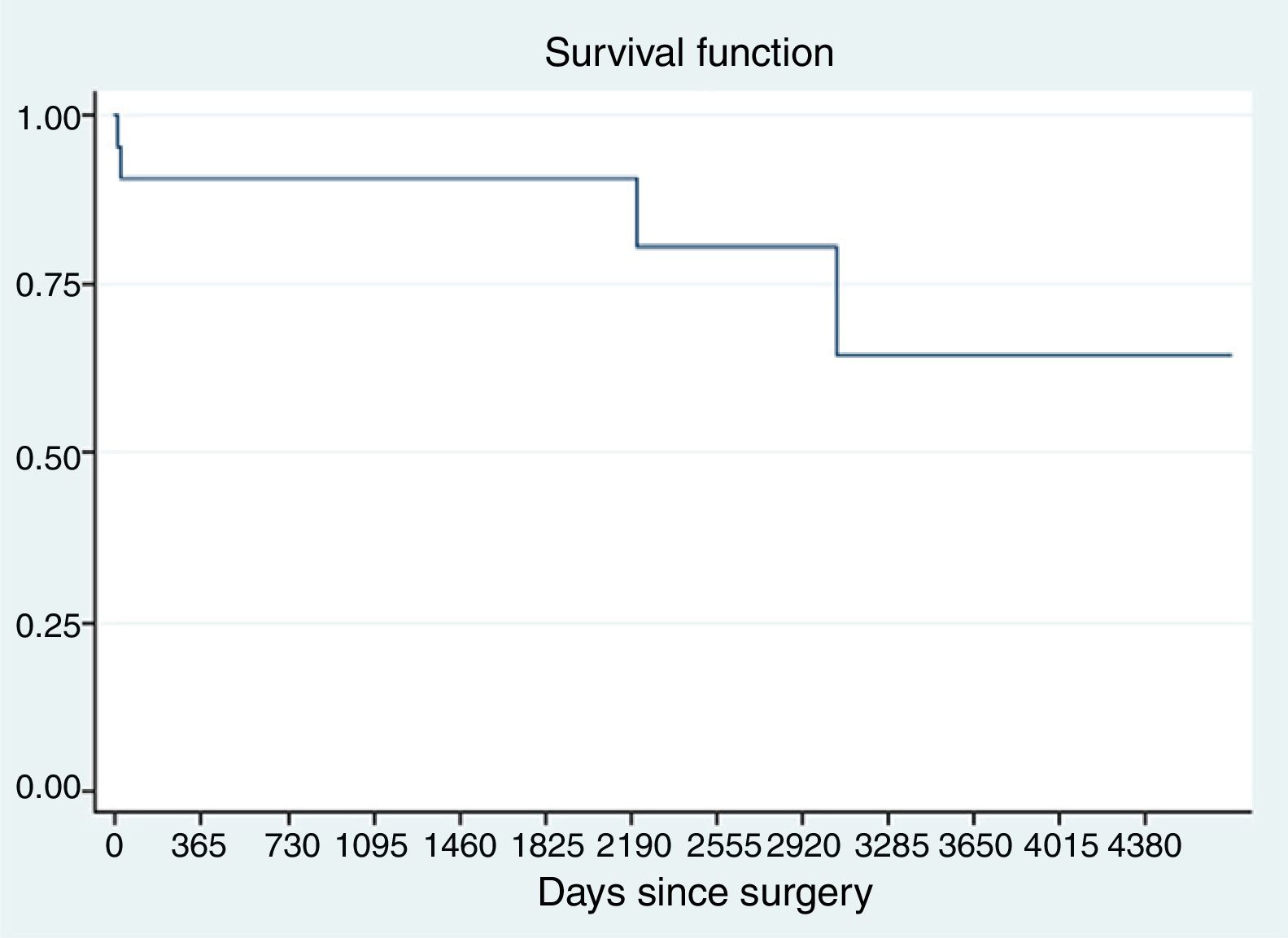
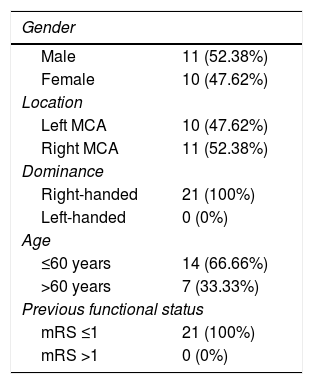
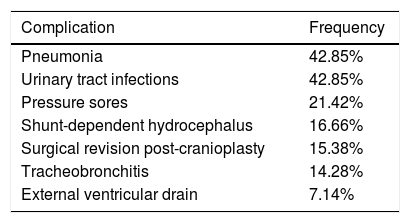
MethodsIn our review, twenty-one patients were included from 2004 to 2017, according to the protocol for the management of ischaemic stroke that is implemented in our institution. The relatives were interviewed by telephone. The functional outcome at discharge, 3 months, 1year, and at present was measured using the modified Rankin scale (mRS).
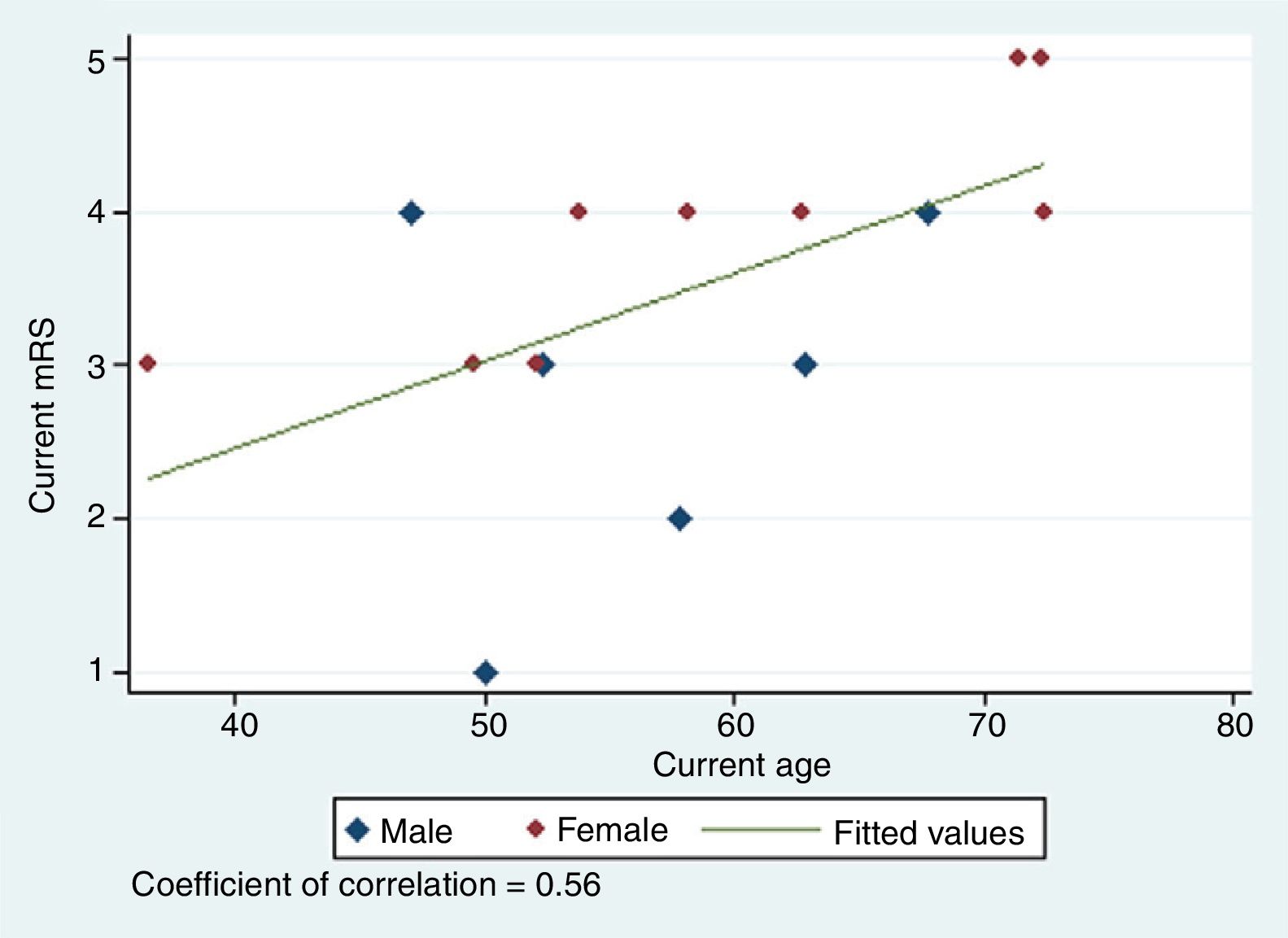
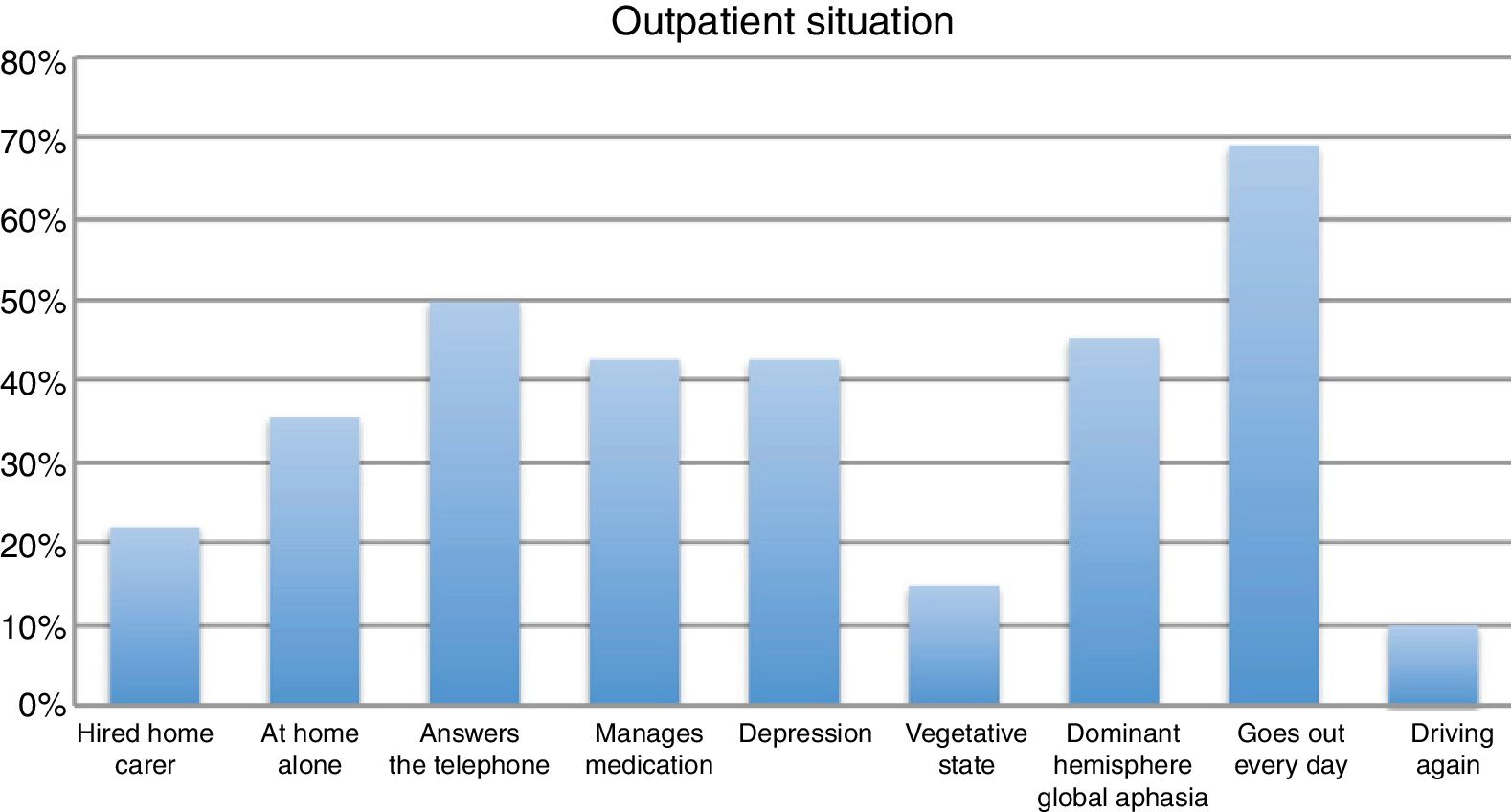
ResultsPatient age was shown to be directly related to the mRS (r=0.56; p=0.035) and 37.5% achieved a good outcome (mRS≤3). 78.9% of the interviewed relatives would repeat the surgical decision.
ConclusionWe present a 21 patients group where the best outcome was achieved in patients ≤60 years old. The severe neurological sequelae in patients with malignant infarction subjected to decompressive hemicraniectomy are tolerated and accepted by most families to the benefit of survival. We must not let this family satisfaction hide the prognosis, having to contextualize it within the real ambulatory situation of the patients.
El pronóstico en los infartos malignos de un hemisferio siembra dudas entre los neurocirujanos a la hora de indicar una hemicraniectomía descompresiva. ¿Qué resultados a corto y medio plazo se obtienen? ¿están las familias satisfechas con la cirugía una vez con el enfermo en su domicilio?. En el presente trabajo analizamos nuestra experiencia en esta materia en los últimos 13 años.
Material y métodosIncluimos en nuestra revisión a 21 pacientes intervenidos entre 2004 y 2017 siguiendo la vía clínica de nuestro centro para el ictus. Se entrevistó a los familiares vía telefónica. Se midió el resultado funcional al alta, 3 meses, 1 año y actual con la escala modificada de Rankin (mRS).
ResultadosLa edad demostró estar directamente relacionada con la mRS (r=0.56; p=0.035) y en el 37.5% se obtuvo un buen resultado (mRS≤3). El 78.9% de los familiares entrevistados repetiría la decisión quirúrgica tomada.
ConclusionesAportamos un grupo de 21 pacientes sometidos a craniectomía descompresiva por infarto maligno donde los mejores resultados funcionales se han dado entre los <60 años. Las graves secuelas neurológicas en pacientes con infarto maligno sometidos a hemicraniectomía descompresiva fueron toleradas y aceptadas por la mayoría de familias a favor de su supervivencia. No debemos dejar que esta satisfacción familiar camufle el pronóstico, teniendo que contextualizarla dentro de la situación real ambulatoria de los pacientes.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.