To perform a score with early clinical and radiological findings after a TBI that identifies the patients who in their subsequent evolution are going to undergo DC.
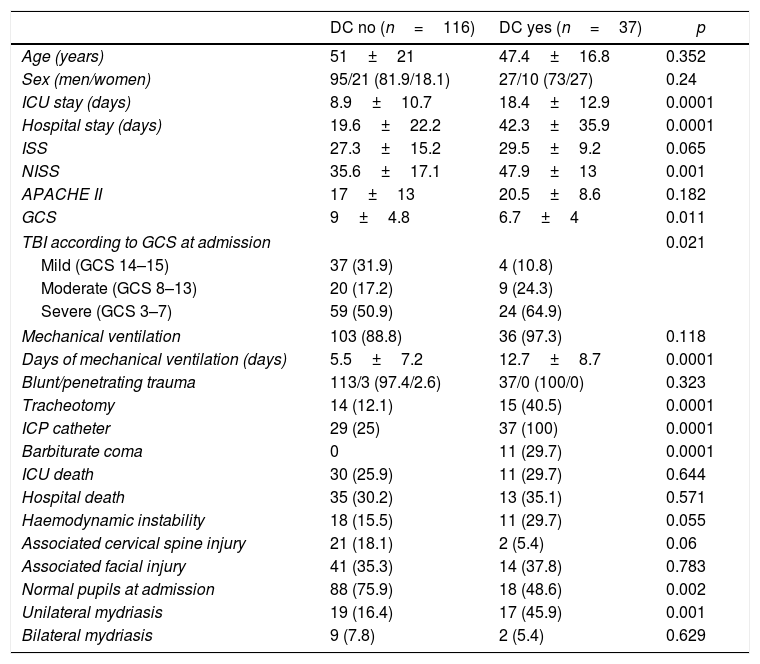
MethodObservational study of a retrospective cohort of patients who, after a TBI, enter the Neurocritical Section of the Intensive Care Unit of our hospital for a period of 5 years (2014–2018). Detection of clinical and radiological criteria and generation of all possible models with significant, clinically relevant and easy to detect early variables. Selection of the one with the lowest Bayesian Information Criterion and Akaike Information Criterion values for the creation of the score. Calibration and internal validation of the score using the Hosmer–Lemeshow and a bootstrapping analysis with 1000 re-samples respectively.
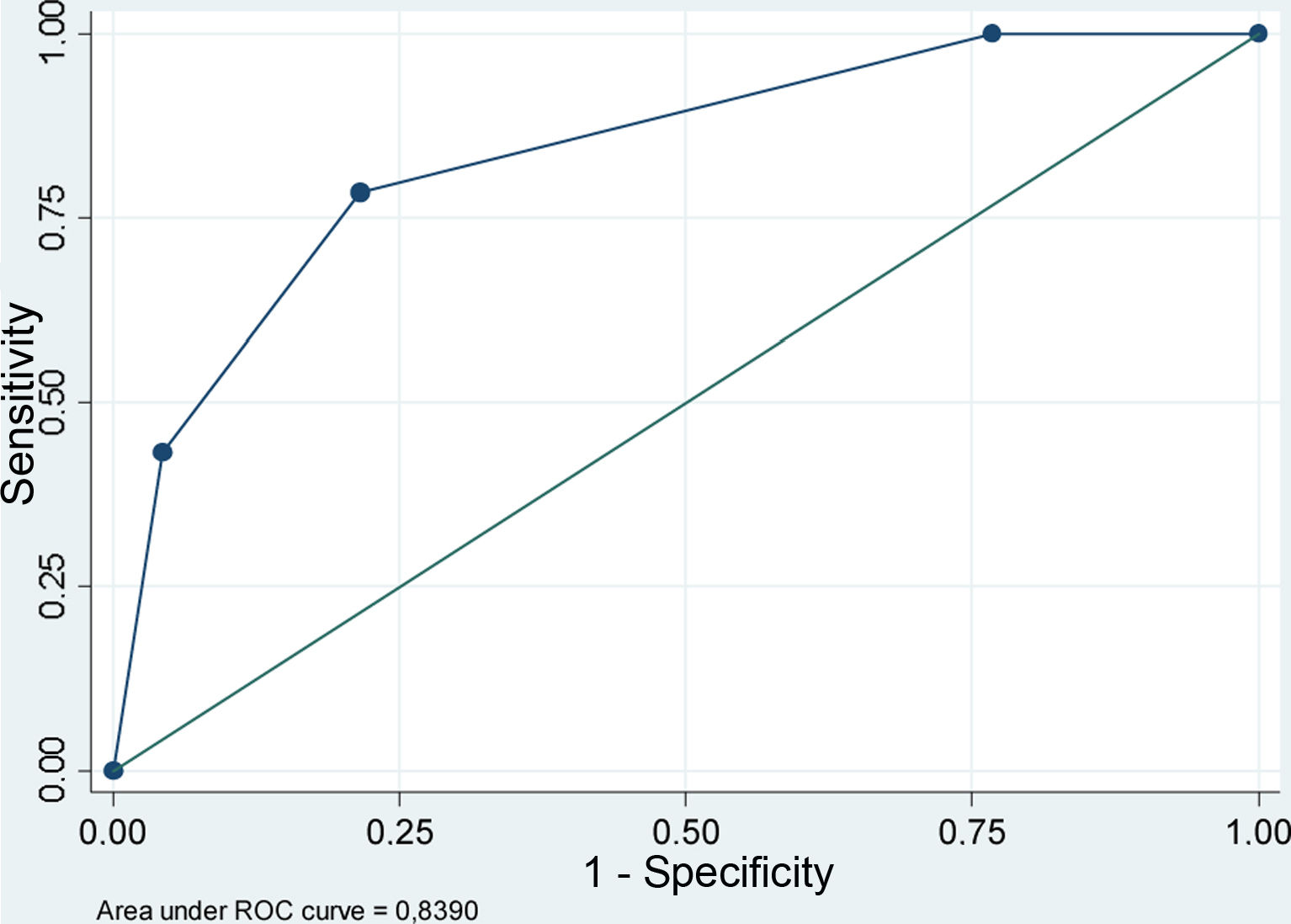
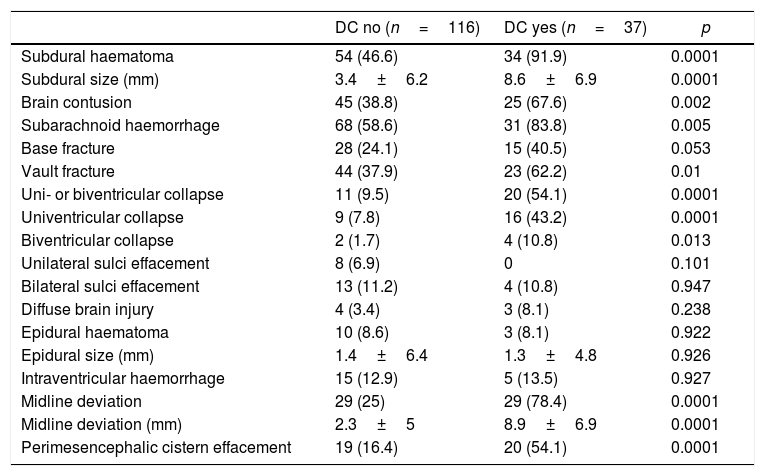
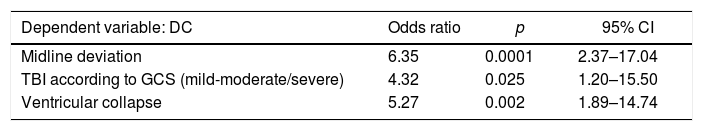
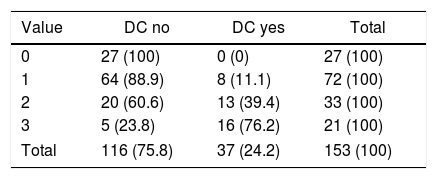
Results37 DC were performed in 153 patients who were admitted after a TBI. The resulting final model included Cerebral Midline Deviation, GCS and Ventricular Collapse with an Area under ROC Curve: 0.84 (95% IC 0.78–0.91) and Hosmer–Lemeshow p=0.71. The developed score detected well those patients who were going to need an early DC (first 24h) after a TBI (2.5±0.5) but not those who would need it in a later stage of their disease (1.7±0.8). However, it seems to advice us about the patients who, although not requiring an early DC are likely to need it later in their evolution (DC after 24h vs. do not require DC, 1.7±0.8 vs. 1±0.7; p=0.002).
ConclusionWe have developed a prognostic score using early clinical-radiological criteria that, in our environment, detects with good sensitivity and specificity those patients who, after a TBI, will require a DC.
Realizar una escala con parámetros clínicos y radiológicos precoces tras un TCE que identifique a los enfermos que en su evolución posterior van a someterse a una CD.
MétodoEstudio observacional de una cohorte retrospectiva de pacientes que tras un TCE ingresan en la Sección de Neurocríticos del Servicio de Medicina Intensiva de nuestro hospital durante un periodo de 5 años (2014-2018). Detección de variables clínicas y radiológicas y creación de todos los modelos posibles con las variables significativas, clínicamente relevantes y de fácil detección precoz. Selección del que presentaba valores más bajos de criterios de información bayesiano y de Akaike para la creación de la escala. Calibración y validación interna mediante la prueba de bondad de ajuste de Hosmer-Lemeshow y análisis bootstrapping con 1.000 re-muestreos.
ResultadosSe realizaron 37 CD en 153 enfermos que ingresaron tras un TCE. El modelo final resultante incluía desviación de línea media, GCS y colapso ventricular con un área bajo la curva ROC de 0,84 (IC95% 0,78-0,91) y Hosmer-Lemeshow p=0,71. La escala desarrollada detectaba bien a los enfermos que iban a precisar una CD precoz (en las primeras 24horas) tras un TCE (2,5±0,5) pero no a aquellos que la necesitarían en una fase más tardía de su enfermedad (1,7±0,8). Sin embargo, parece prevenirnos sobre los enfermos que si bien no precisan inicialmente una CD sí tienen probabilidades de necesitarla posteriormente en su evolución (CD tardía vs. no precisan CD, 1,7±0,8 vs. 1±0,7; p=0,002).
ConclusiónHemos desarrollado una escala pronóstica que permite detectar en nuestro medio, con una buena sensibilidad y especificidad y usando criterios clínico-radiológicos precoces, aquellos pacientes que tras un TCE van a precisar una CD.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.