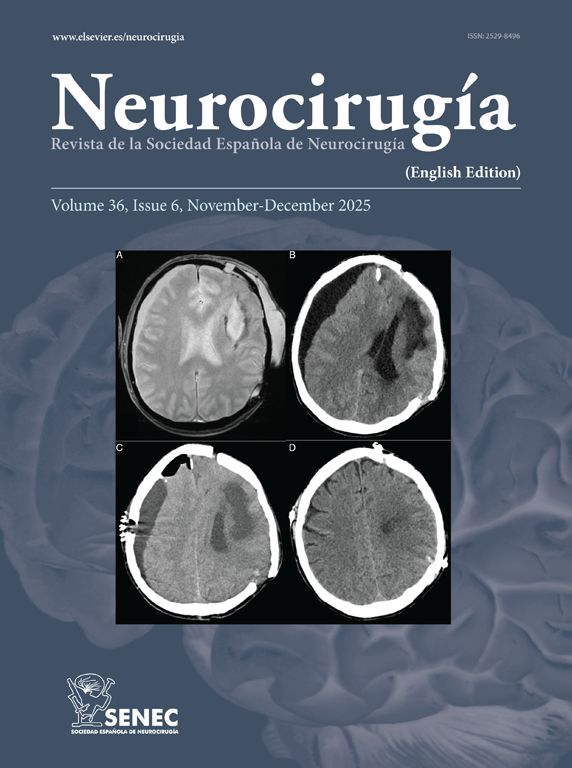
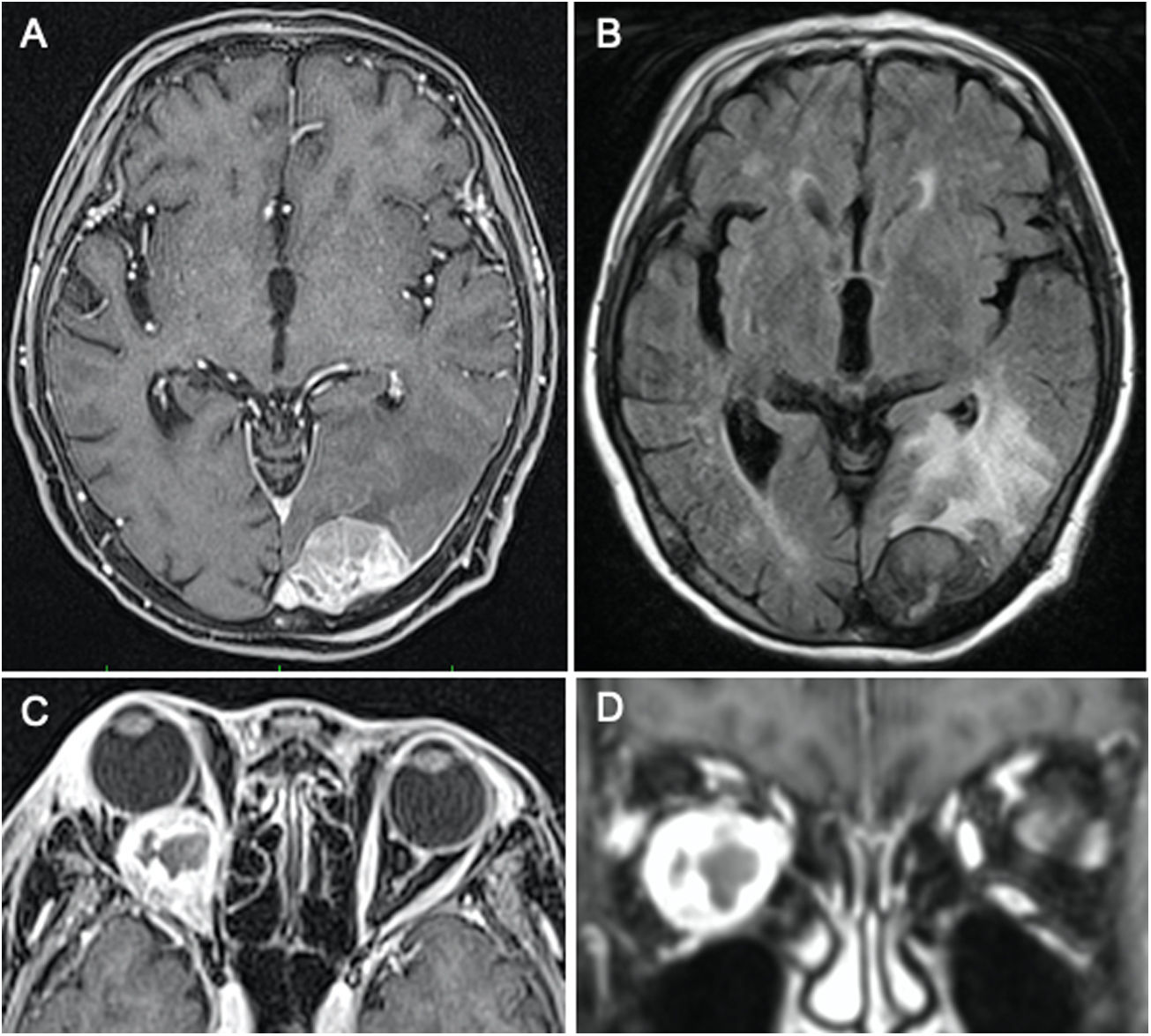
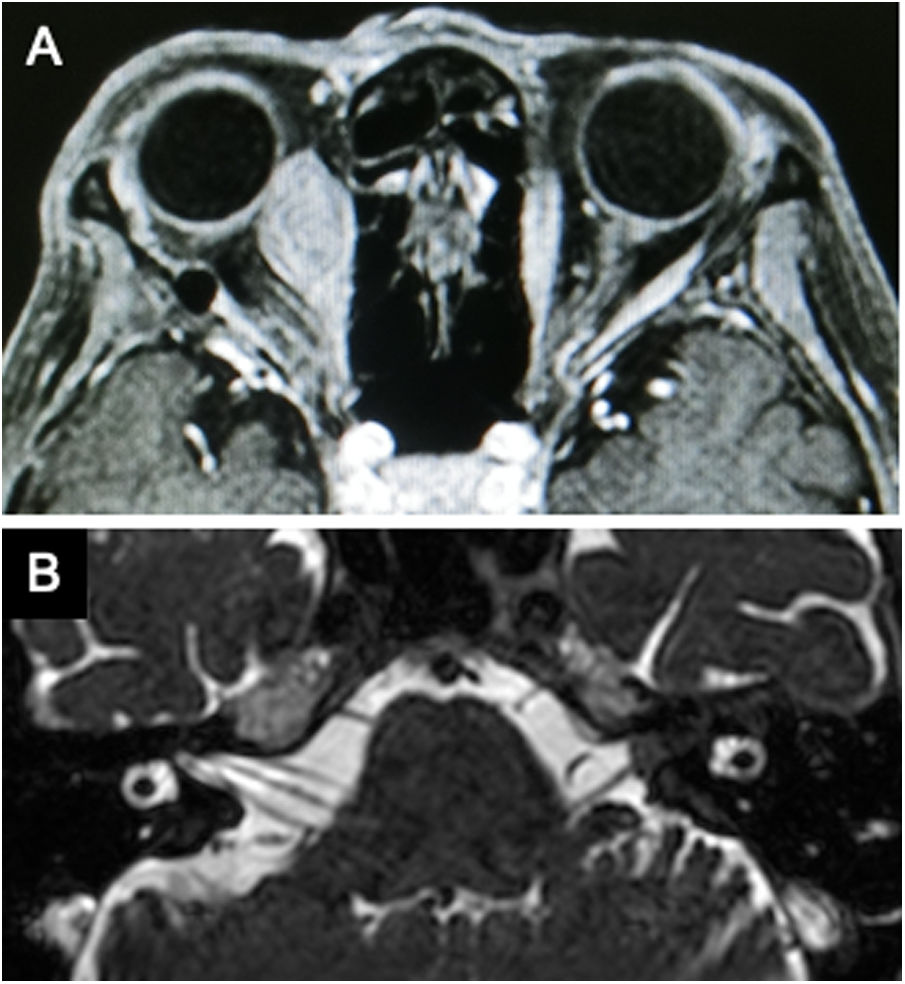
Proliferative activity examined by Ki67 labeling index (LI) plays pivotal role for managing gastrointestinal neuroendocrine tumor (GI-NET). Few reports indicated the intra-patient heterogeneity of Ki67-LI among metastatic tumor sites. We report a case of brain and orbital metastases from GI-NET that showed discrepancy of the Ki67-LI. A 71 year-old woman who was diagnosed as GI-NET with liver and bone metastases and performed medical therapy, had headache, right exophthalmos, and pain of right eye and was referred to our department. Magnetic resonance image revealed that tumors in the left occipital region and right orbit. We diagnosed as metastatic brain and orbital tumors from GI-NET. Surgical removal of both symptomatic lesions was performed and the diagnosis was pathologically confirmed. Immunohistochemical studies revealed the discrepancy of the Ki67-LI of the lesions (brain tumor: 8% versus orbital tumor: 22%). Sampling of multiple metastatic sites may prevent underestimate tumor proliferative activity.
La actividad proliferativa examinada por el índice de etiquetado Ki67 (LI) desempeña un papel fundamental en el tratamiento del tumor neuroendocrino gastrointestinal (GI-NET). Pocos informes indican la heterogeneidad intrapaciente del Ki67-LI entre las localizaciones de los tumores metastásicos. Presentamos un caso de metástasis cerebrales y orbitales de GI-NET que mostró discrepancia del Ki67-LI. Una mujer de 71 años a la que se le diagnosticó un GI-NET con metástasis hepáticas y óseas y que realizó tratamiento médico, presentó cefalea, exoftalmos derecho y dolor de ojo derecho, y fue remitida a nuestro departamento. La imagen de resonancia magnética reveló que los tumores en la región occipital izquierda y la órbita derecha. Diagnosticamos como metástasis tumores cerebrales y orbitales de GI-NET. Se realizó la extirpación quirúrgica de ambas lesiones sintomáticas y se confirmó patológicamente el diagnóstico. Los estudios inmunohistoquímicos revelaron la discrepancia del Ki67-LI de las lesiones (tumor cerebral: 8% frente a tumor orbitario: 22%). El muestreo de múltiples focos metastásicos puede evitar que se subestime la actividad proliferativa del tumor.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.