To determine the prevalence, clinical and radiological risk factors, and surgical management of post-traumatic syringomyelia (PTS) in a 19-year cohort study of Spinal Cord Injury (SCI) patients treated at a SCI rehabilitation center.
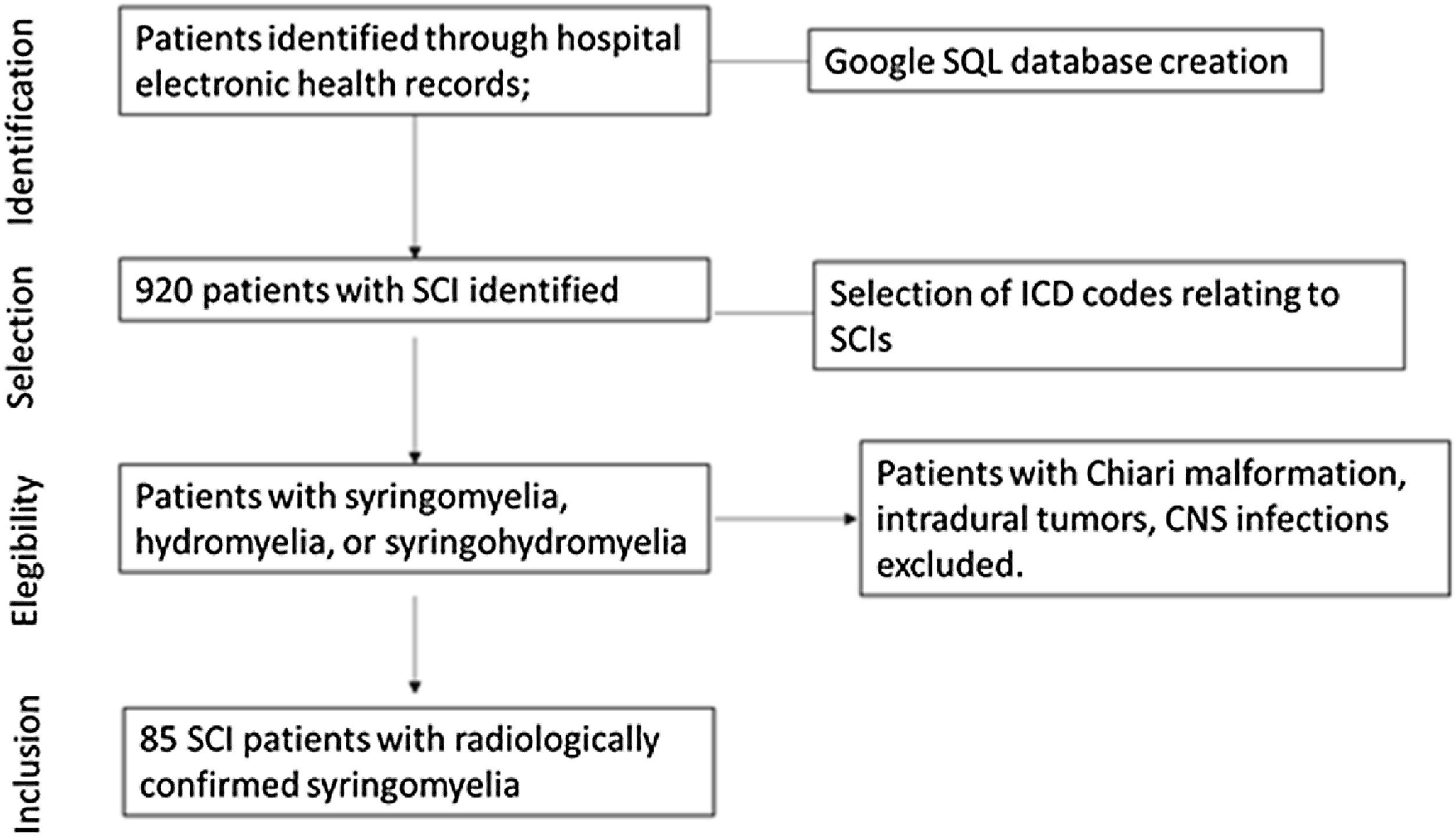
MethodsRetrospective study of SCI patients in whom PTS was radiologically confirmed between January 2000 and December 2018. Protocols for assessing signs and symptoms of PTS were applied prior to PTS diagnosis and treatment and later at neurosurgical and rehabilitation reviews. The variables analyzed were prevalence, demographic data, trauma event, clinical and radiological risk factors, location and size of the syrinx, and effectiveness of the surgical procedures.
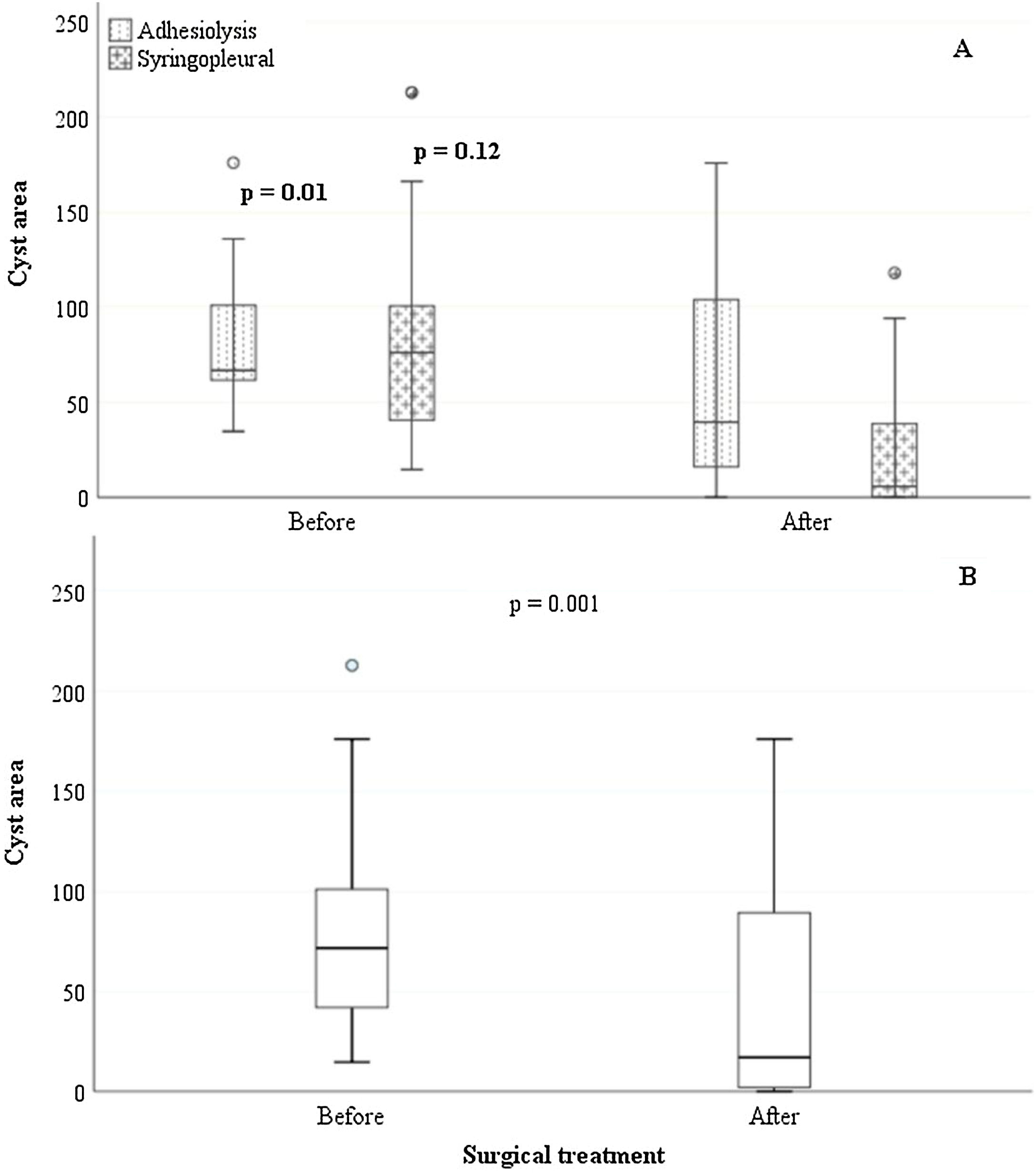
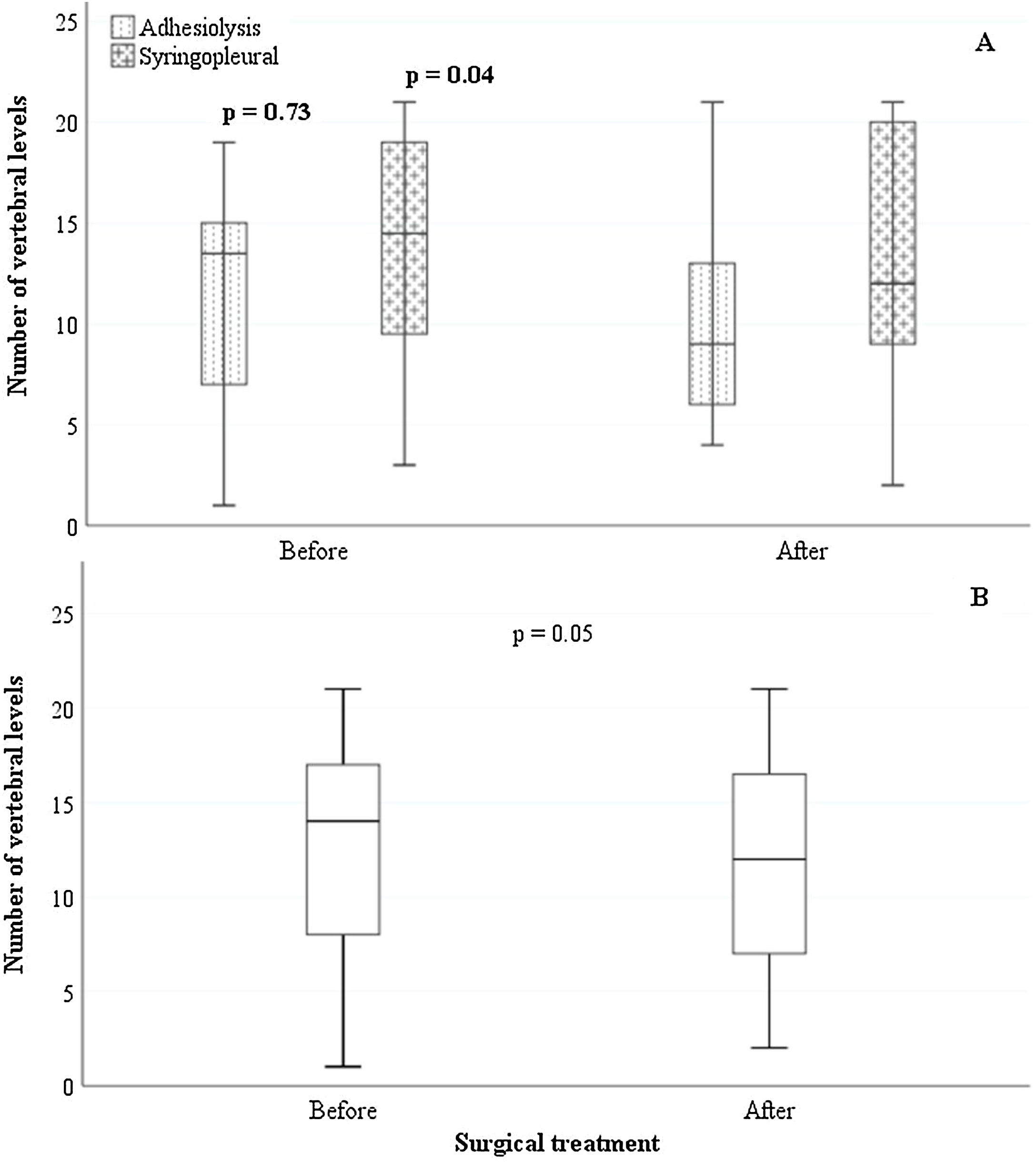
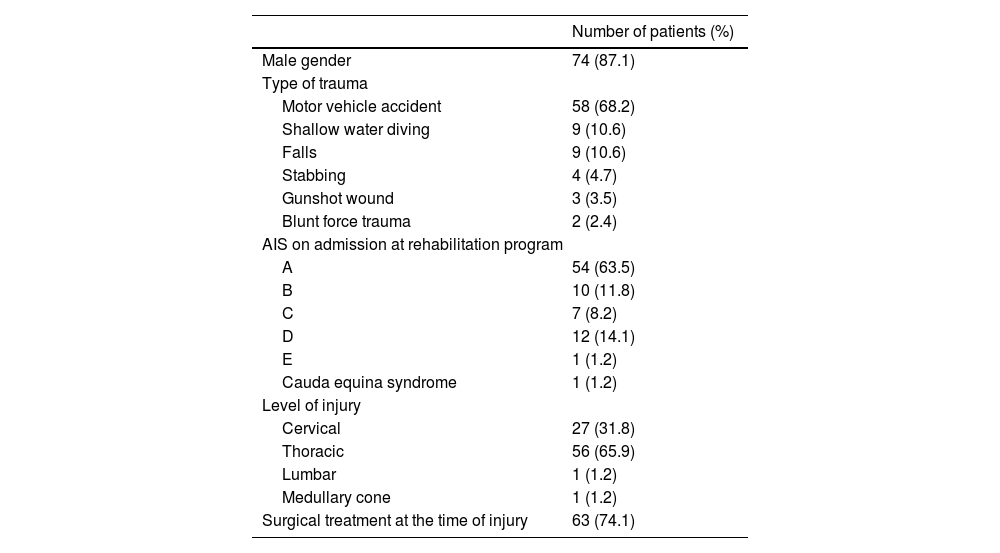
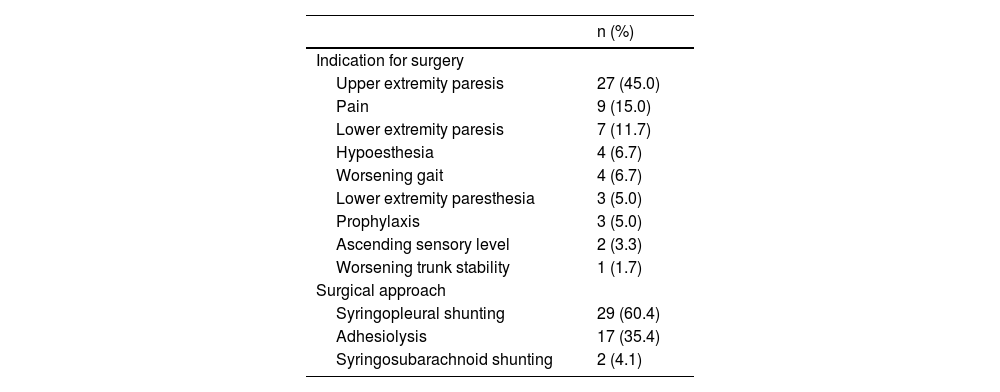
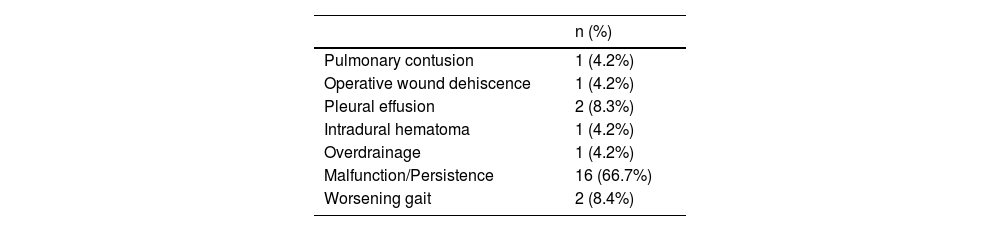
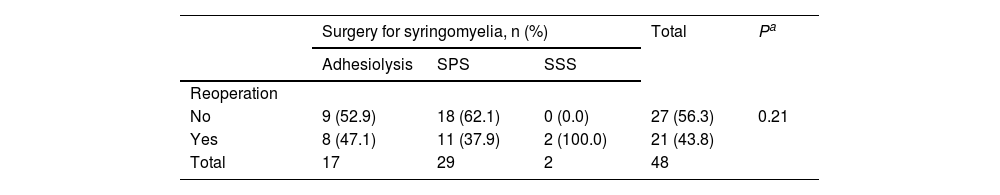
ResultsOver the 19-year period, review of 920 SCI patients revealed 85 patients who met the clinical and neuroradiological criteria for the diagnosis of PTS and who were prospectively followed. Road traffic accidents were the leading cause of injury (n = 58; 68.2%), syringomyelia was most commonly observed in the thoracic spine (n = 56; 65.9%), and upper extremity paresis was the most common indication for surgical treatment (n = 27; 45%). Surgical treatment was indicated in 48 patients and the operative procedures included 29 syringopleural shunts (60.4%), 17 adhesiolysis (35.4%), and two syringosubarachnoid shunts (4.1%). The prevalence of PTS was 9% and was higher in patients with ASIA impairment scale grade A injuries. Most patients with PTS (63/85, 74.1%) were treated surgically at the time of injury. There was a significant reduction both in the extent (p = 0.05) and largest area (p = 0.001) of the syrinx after surgical treatment. Reoperation rates were 47% and 37.9% for adhesiolysis and syringopleural shunting, respectively.
ConclusionFollow-up and routine clinical examination of SCI patients is critical for the diagnosis of PTS in patients with late neurological deterioration. Surgical treatment has a positive impact in reducing the size of the syrinx as seen on postoperative MRI.
Determinar la prevalencia, los factores de riesgo clínicos y radiológicos y el tratamiento quirúrgico de la siringomielia postraumática (SPT) en un estudio de cohorte de 19 años de pacientes con Lesion medular Espinal (LME) tratados en un centro de rehabilitación de LME.
MétodosEstudio retrospectivo de pacientes con LME en quienes se confirmó radiológicamente el SPT entre enero de 2000 y diciembre de 2018. Se aplicaron protocolos para evaluar los signos y síntomas del SPT antes del diagnóstico y tratamiento del SPT y posteriormente en las revisiones neuroquirúrgicas y de rehabilitación. Las variables analizadas fueron prevalencia, datos demográficos, evento traumático, factores de riesgo clínicos y radiológicos, ubicación y tamaño de la siringe y efectividad de los procedimientos quirúrgicos.
ResultadosDurante el período de 19 años, la revisión de 920 pacientes con LME reveló que 85 pacientes cumplían con los criterios clínicos y neurorradiológicos para el diagnóstico de SPT y que fueron seguidos prospectivamente. Los accidentes de tráfico fueron la principal causa de lesiones (n = 58; 68,2%), la siringomielia se observó con mayor frecuencia en la columna torácica (n = 56; 65,9%) y la paresia de las extremidades superiores fue la indicación más común de tratamiento quirúrgico (n = 27; 45%). Se indicó tratamiento quirúrgico en 48 pacientes y los procedimientos quirúrgicos incluyeron 29 derivaciones siringopleurales (60,4%), 17 adhesiolisis (35,4%) y dos derivaciones siringosubaracnoideas (4,1%). La prevalencia de SPT fue del 9% y fue mayor en pacientes con lesiones de grado A en la escala de deterioro de ASIA. La mayoría de los pacientes con SPT (63/85, 74,1%) fueron tratados quirúrgicamente en el momento de la lesión. Hubo una reducción significativa tanto en la extensión (p = 0,05) como en el área más grande (p = 0,001) de la siringe después del tratamiento quirúrgico. Las tasas de reoperación fueron del 47% y del 37,9% para adhesiolisis y derivación siringopleural, respectivamente.
ConclusionesEl seguimiento y el examen clínico de rutina de los pacientes con LME es fundamental para el diagnóstico de SPT en pacientes con deterioro neurológico tardío. El tratamiento quirúrgico tiene un impacto positivo en la reducción del tamaño de la siringe, como se observa en la resonancia magnética posoperatoria.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.