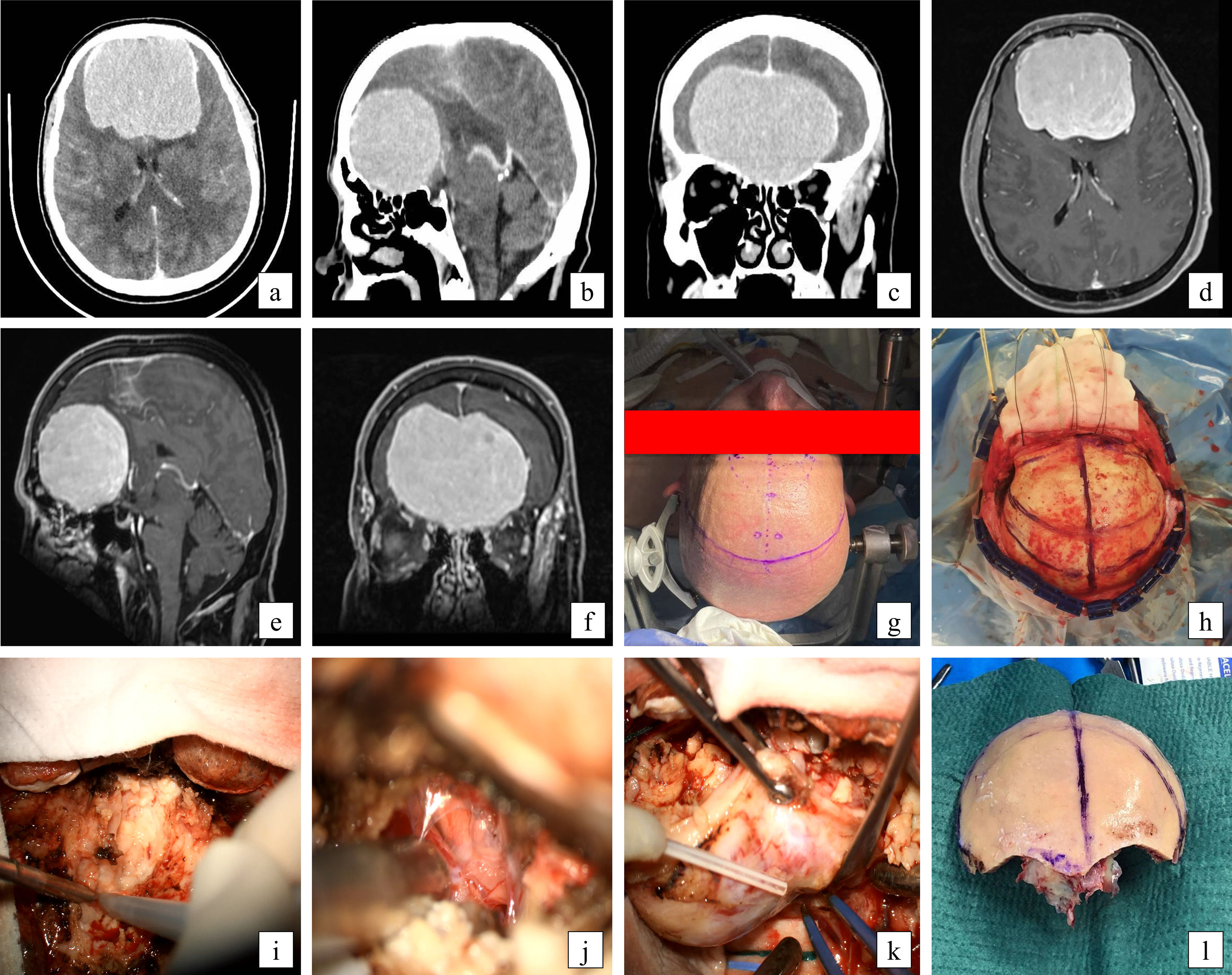
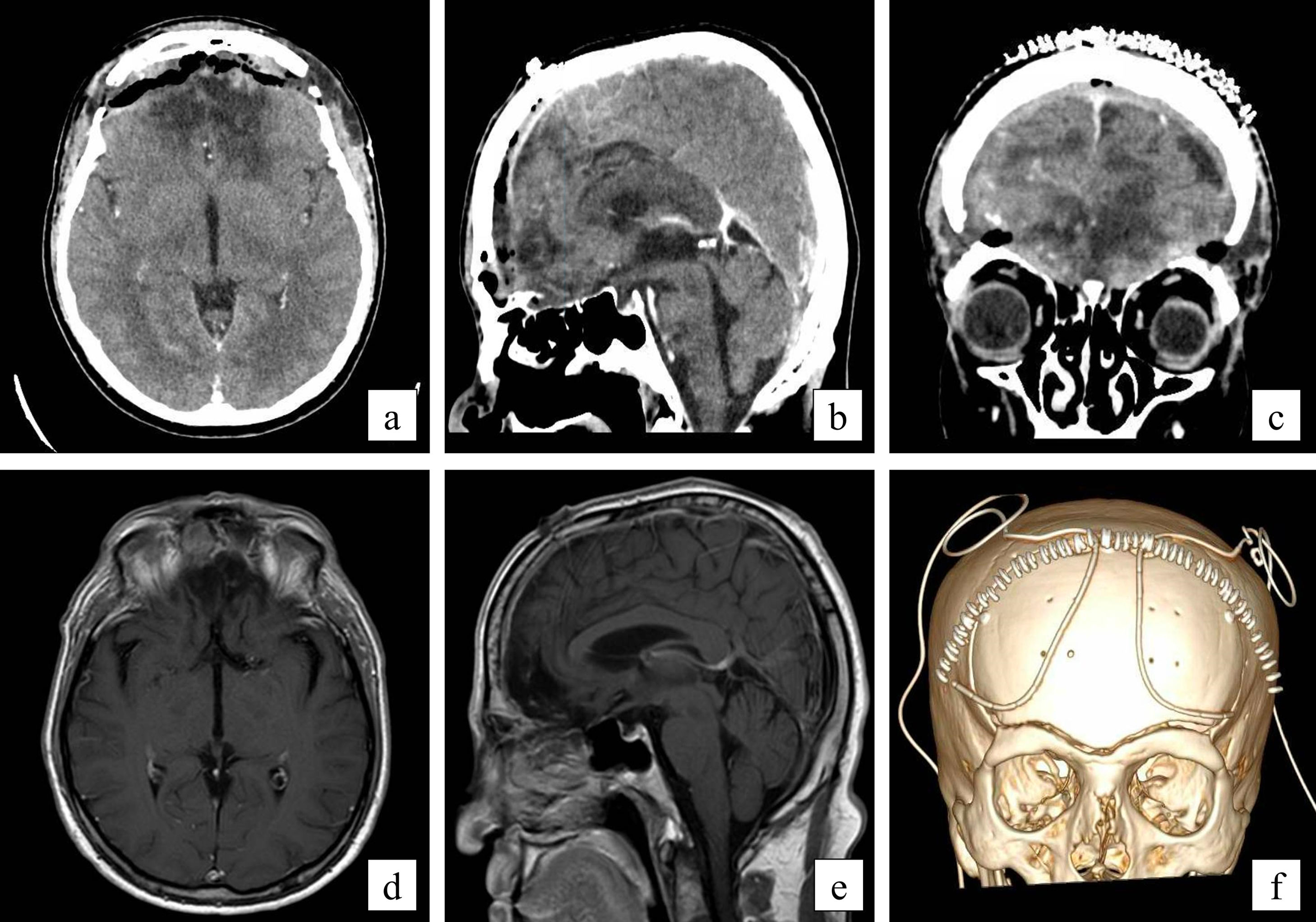
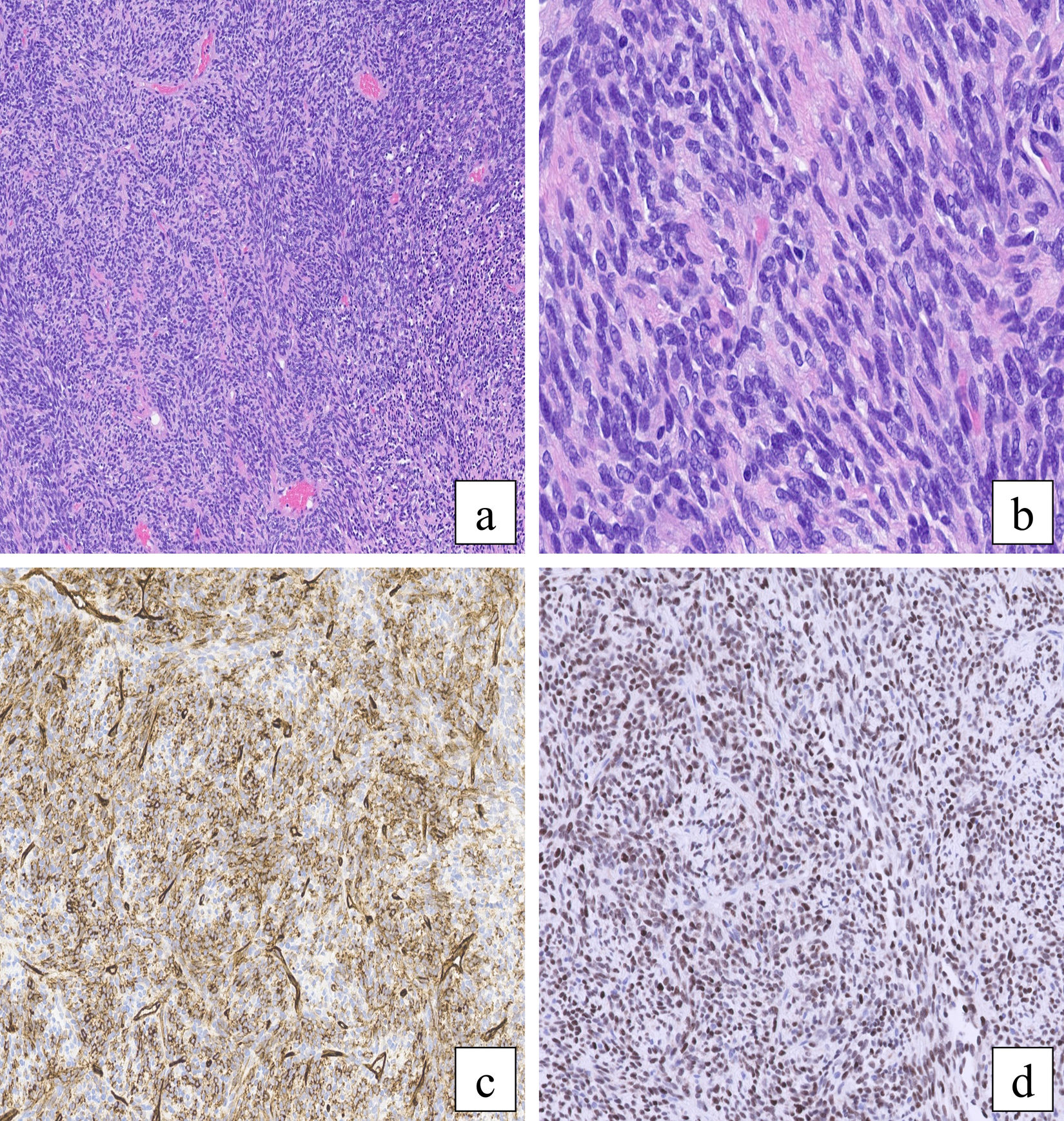
Solitary fibrous tumors are rare mesenchymal neoplasms that can develop in any part of the body, with those that settle intracranially being confused with meningiomas as a general rule. We present the case of a 57-year-old man referred to our hospital due to bifrontal headache, anosmia, and behavioral alterations of 6 months' duration. Radiological studies revealed the existence of a large tumor mass with an extra-axial appearance and location in the anterior cranial fossa, initially compatible with a giant meningioma of the olfactory groove. Gross total resection of the mass was carried out. The pathological diagnosis was unexpected: a solitary fibrous tumor (WHO grade 1, 2021). Given the aggressive nature of these lesions, with a tendency to recurrence, malignant transformation and even metastasis, surgery with macroscopically complete resection intention should constitute the first therapeutic option. Close clinical-radiological follow-up after the procedure is justified.
Los tumores fibrosos solitarios son neoplasias mesenquimales infrecuentes que pueden desarrollarse en cualquier parte del organismo, siendo aquellos que se asientan intracranealmente confundidos con meningiomas por norma general. Presentamos el caso de un varón de 57 años remitido a nuestro centro presentando cuadro de cefalea bifrontal, anosmia y alteración del comportamiento de 6 meses de evolución. Los estudios radiológicos revelaron la existencia de una gran masa tumoral de apariencia extra-axial y localización en fosa craneal anterior, inicialmente compatible con un meningioma gigante del surco olfatorio. Se llevó a cabo la resección quirúrgica radical de la lesión. El diagnóstico anatomopatológico resultó inesperado: un tumor fibroso solitario (grado 1 de la OMS, 2021). Dada la naturaleza agresiva de estas lesiones, con tendencia a la recidiva, transformación maligna e incluso metastatización, la cirugía con intención resectiva macroscópicamente completa debe constituir la primera opción terapeútica. El seguimiento clínico-radiológico estrecho tras el procedimiento está justificado.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.