In cases where adjacent segment disease (ASD) develops following lumbar fusion surgery, various surgical approaches can be employed. In such cases, removal of the instrumentation can positively impact lumbar pain syndrome. One frequently used method is short-segment fixation-decompression (SSFD). One of minimally invasive methods is microsurgical bilateral decompression via unilateral approach (MBDU). This study aims to determine which method is more effective and safe in cases that developed ASD following fusion surgery by comparing SSFD and MBDU after instrumentation removal.
MethodsA retrospective analysis was conducted on 47 cases treated with SSFD and 29 cases treated with MBDU. The groups were analyzed for gender, age, preoperative symptom duration, duration of hospitalization, and Visual Analogue Scale (VAS) scores and Oswestry Disability Index (ODI) scores during the preoperative and postoperative intermittent follow-up periods.
ResultsDuration of hospitalization was higher in the SSFD group compared to the MBDU group (p = <0.001 CI = 56,42–76,24 and 22,04–25,13 respectively), mean transverse canal diameter ratio in the decompressed segment was lower in the SSFD group (p = 0,03 IC = 0,24–0,31 for SSFD y 0,40–0,47 for MBDU), and ODI indices were higher in the SSFD group in all follow-ups (p = <0.001). During the follow-up period, symptomatic ASD was observed in 3 of 47 patients in the SSFD group, whereas no symptomatic ASD was observed in the MBDU group.
ConclusionIn selected patients who develop ASD after fusion surgery MBDU after instrumentation removal can be considered as a minimally invasive option that does not exacerbate postoperative lumbar pain syndrome or lead to the development of new ASD. To the best of our knowledge, this is the first comparison of these two techniques in literature after removal of spinal fixators in lumbar ASD cases.
En los casos en los que se desarrolla una enfermedad del segmento adyacente (ESA) después de una cirugía de fusión lumbar, se pueden emplear varios abordajes quirúrgicos. En tales casos, la eliminación de la instrumentación puede tener un impacto positivo en el síndrome de dolor lumbar. Un método utilizado con frecuencia es la fijación-descompresión de nivel corto (FJNC). Uno de los métodos mínimamente invasivos es la descompresión bilateral microquirúrgica mediante un abordaje unilateral (DBMAU). Este estudio tiene como objetivo determinar qué método es más eficaz y seguro en los casos que desarrollaron ESA después de una cirugía de fusión comparando FJNC y DBMAU después de la eliminación de la instrumentación.
MétodosSe realizó un análisis retrospectivo de 47 casos tratados con FJNC y 29 casos tratados con DBMAU. Se analizaron los grupos en cuanto a género, edad, duración de los síntomas preoperatorios, duración de la hospitalización y puntuaciones de la escala analógica visual (EVA) y del índice de discapacidad de Oswestry (ODI) durante los períodos de seguimiento intermitente preoperatorio y posoperatorio.
ResultadosLa duración de la hospitalización fue mayor en el grupo FJNC en comparación con el grupo DBMAU (p = <0,001 IC = 56,42–76,24 y 22,04–25,13 respectivamente), la relación del diámetro del canal transversal medio en el segmento descomprimido fue menor en el grupo FJNC (p = 0,03 IC = 0,24–0,31 para SSFD y 0,40–0,47 para MBDU) y los índices ODI fueron mayores en el grupo FJNC en todos los seguimientos (p = <0,001). Durante el período de seguimiento, se observó ESA sintomática en 3 de 47 pacientes en el grupo FJNC, mientras que no se observó ESA sintomática en el grupo DBMAU.
ConclusiónEn pacientes seleccionados que desarrollan ESA después de la cirugía de fusión, la DBMAU después de la extracción de la instrumentación puede considerarse una opción mínimamente invasiva que no exacerba el síndrome de dolor lumbar posoperatorio ni conduce al desarrollo de una nueva ESA. Hasta donde sabemos, ésta es la primera comparación de estas dos técnicas en la literatura tras la retirada de los fijadores espinales en casos de ESA lumbar.
Following fusion surgery, various surgical interventions can be performed in cases where adjacent segment disease (ASD) develops. These interventions include extending the instrumentation with decompression, performing short-level stabilization at the adjacent segment after instrumentation removal, conducting minimally invasive decompression after instrumentation removal, or performing minimally invasive decompression without removing the instrumentation.1–11
In cases with fusion, removal of the instrumentation may positively affect lumbar pain syndrome.12,13 Moreover, in cases where fusion is applied with pedicular screw fixation, the most commonly encountered causes of lumbar pain syndrome include pseudoarthrosis, flatback deformity, ASD, painful disc due to posterolateral fusion as well as implant loosening or fracture.12–14
There is no consensus in the literature regarding the surgical technique that should be used in these cases. However, a positive effect on lumbar pain syndrome following the removal of instrumentation has been reported.12–14 Additionally, there is debate regarding what the subsequent intervention should be after the removal of instrumentation. One commonly used method is short-segment fixation-decompression (SSFD) with extensive decompression (laminectomy) at the segment with ASD, and the use of endoscopic or microscopic minimally invasive techniques is also becoming more common.15,16
Regardless of these cases, microsurgical bilateral decompression via unilateral approach (MBDU)ok is also a minimally invasive technique used in degenerative spinal stenosis.17–21
This study aimed to determine which method is more effective and safe in patients who developed ASD following fusion surgery by comparing SSFD and MBDU after the removal of instrumentation.
Materials and methodsThe study was started with ethics committee approval with protocol number.2024-TBEK 2024/07/11.
A total of 47 cases who had previously undergone lumbar fusion and subsequently developed ASD and underwent instrumentation removal followed by SSFD at the Neurosurgery Clinic of Yüksek İhtisas Training and Research Hospital, and a total of 29 cases with a similar history that underwent instrumentation removal followed by MBDU at the Neurosurgery Clinic of Bursa VM Medical Park Hospital between 2017 and 2021 were retrospectively examined.
Surgical procedurePatients who had previously undergone lumbar fixation and developed ASD underwent posterior lumbar decompressive laminectomy and pedicle screw instrumentation at the single stenotic level after the removal of instrumentation under general anesthesia in the prone position.
MBDU; Patients who had previously undergone lumbar fixation and developed ASD underwent MBDU to decompress the central canal and bilateral lateral recesses under general anesthesia in the prone position. After the removal of instrumentation microscopic laminotomy was performed on the approach side using an air drill, Kerrison rongeur, and microcurette. Subsequently, decompression was performed on the contralateral side after rotating the operating table to the contralateral side.
While determining the effectiveness of the techniques, it was planned to make comparisons of radicular pain and low back pain in pre and postoperative follow-ups and to determine whether there was adequate decompression. Radicular Visual Analogue Scale (VAS), Owestry Disability Index (ODI) and ratios of canal diameters in pre and postoperative 3-month lumbar MRI imaging were used to make these comparisons.
In determining the safety of the techniques, we looked for complications that may develop secondary to instrumentation such as new ASD development, instability development in both groups; screw fracture-slippage, loosening in the SSFD group, which occurred in the follow-up after optimally performed surgery without perop complications; and radiologic examinations were used for this.
Patients with radiological evidence of instability, those with spinal deformities, those with ASD observed at the spinal transition zones and cases with peroperative complications were excluded from the study.
The surgical technique to be used for patients other than those excluded from the study was determined entirely according to the surgeons' preference.
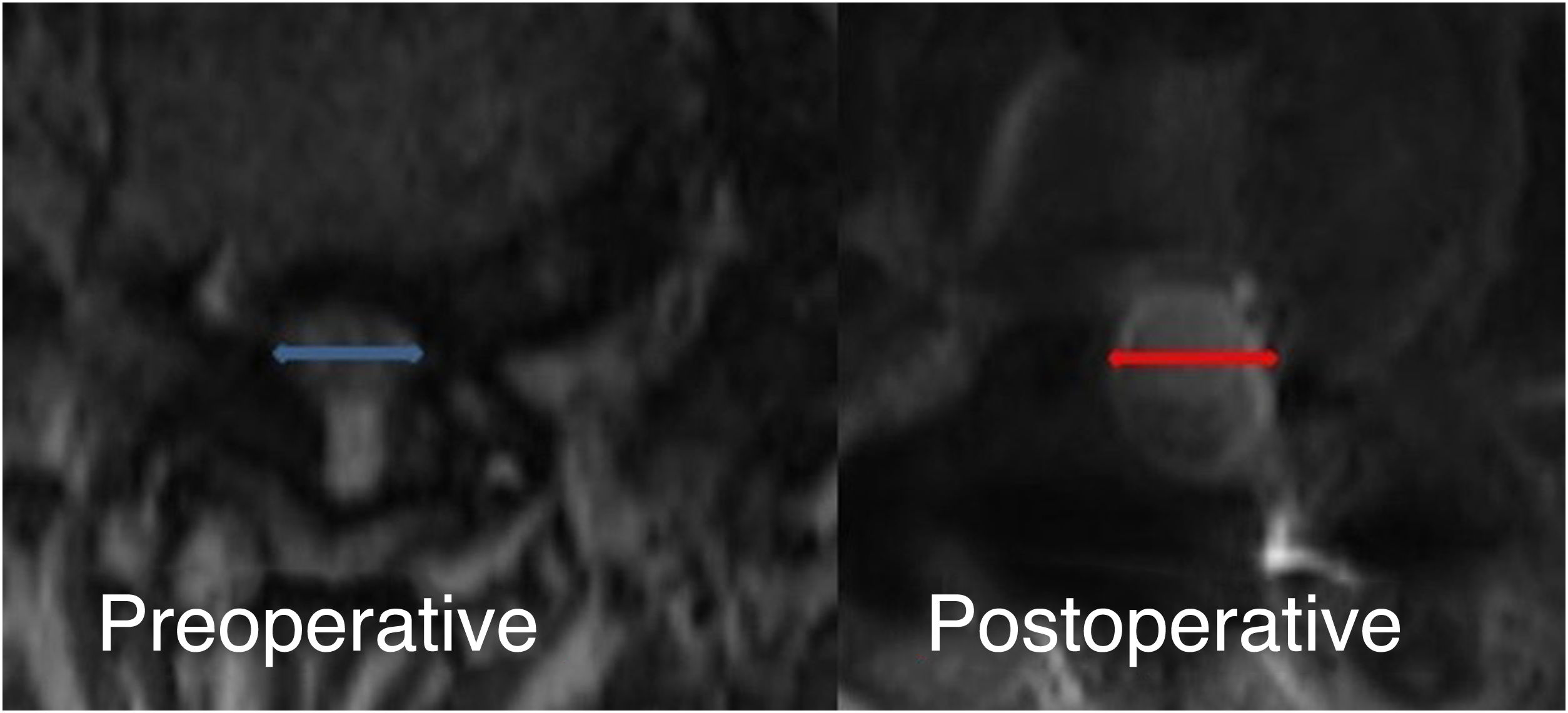
In both groups, gender; age; preoperative symptom duration; duration of hospitalization; preoperative and postoperative 1-h, 10-day, 3-month, 1-year, and final follow-up radicular VAS scores; ratios of canal diameters in preoperative and postoperative 3-month lumbar MRI imaging (Fig. 1); ODI indices during postoperative intermittent follow-up periods were determined and documented. At the same time, postoperative complications that may develop secondary to instrumentation such as new ASD development, instability development in both groups; screw fracture-slippage, loosening in the SSFD group were evaluated and radiologic examinations such as MRI, CT and radiographs were utilized for this purpose. Late complications were noted.
The data were compared statistically, and inferences were made based on data analysis. As the length of skin incision, amount of bleeding, and operation times may vary based on the type and length of previous instrumentation, these parameters were not included in the study.
Statistical analysisStatistical analyses were conducted using the SPSS 26 software. The normal distribution of the variables was assessed with the Kolmogorov-Smirnov test. Possible differences among categorical variables were examined through the Chi-square test. The Student's t-test was employed for the analysis of repeated measures involving two observations. In this analysis, a p-value less than 0.05 was considered that threshold for statistical significance. The descriptive analysis includes the mean, median, standard deviation, and interquartile range (25th-75th percentiles).
ResultsIn the SSFD group, 55.40% of the patients were women and 44.60% were men. The age range was 55–69 years (mean age 67.06 years). In the MBDU group, 51.80% of the patients were women and 48.20% were men. The age range was 48–71 years (mean age 60.37 years). Moreover, there was no significant difference between the two groups in terms of gender distribution and age range (p = 0.4 and 0.3, respectively).
The mean follow-up period was 38.89 months (24–60 months) in the SSFD group and 37.48 months (32–54 months) in the MBDU group.
Preoperative symptom duration ranged between 3 and 12 months in the SSFD group (mean 5.20 months) and 3 and 8 months in the MBDU group (mean 4.80 months). No significant difference was observed between the groups in terms of symptom duration (p = 0.15).
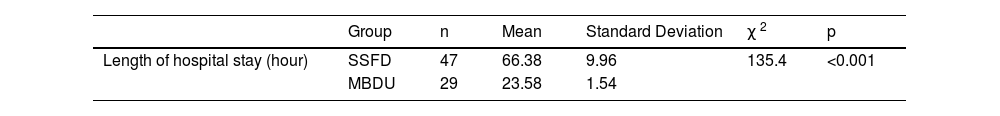
The mean hospitalization duration was 66.38 hours in the SSFD group and 23.58 hours in the MBDU group. Statistical comparison revealed a significant difference (p < 0.001) (Table 1).
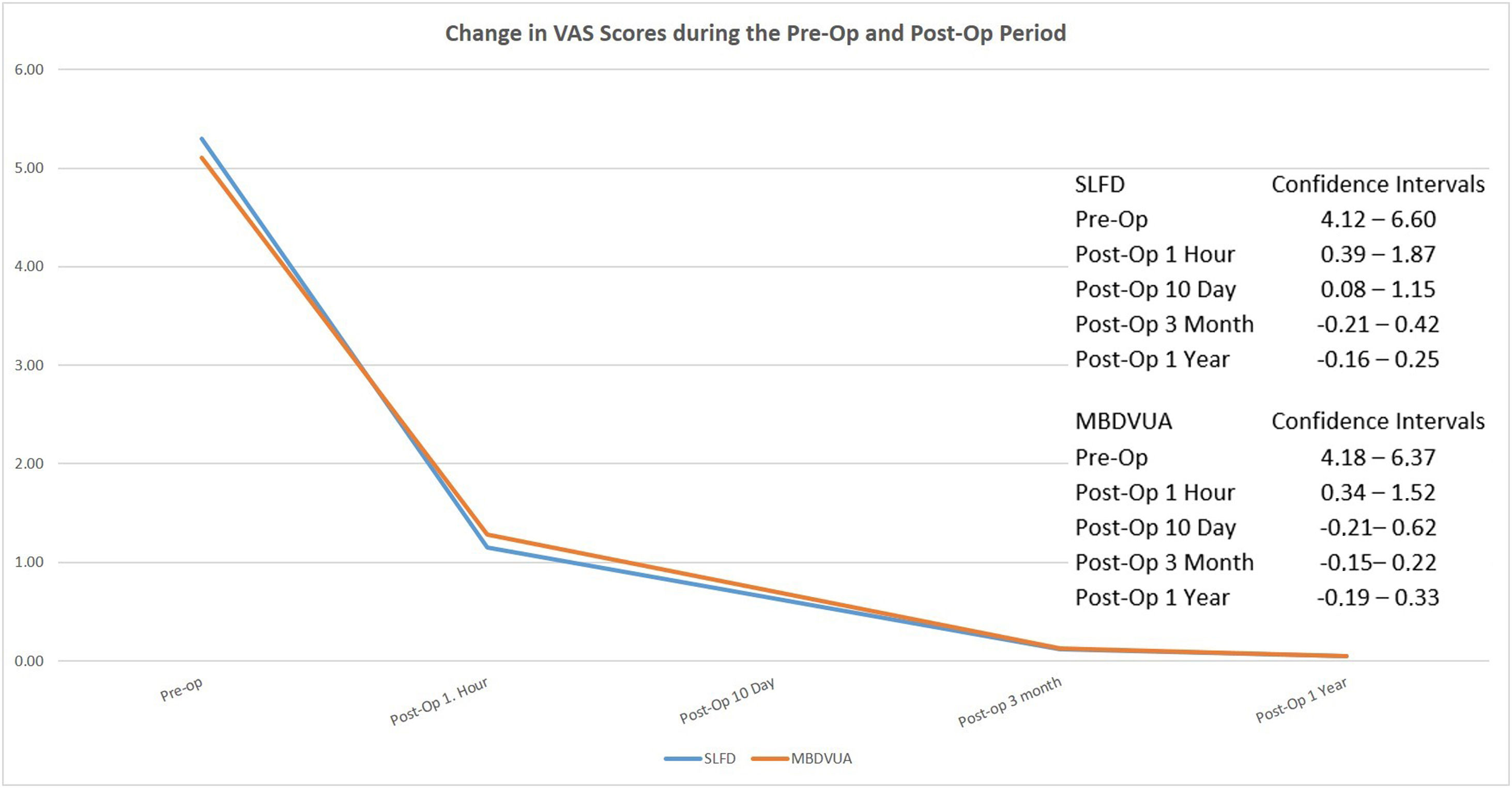
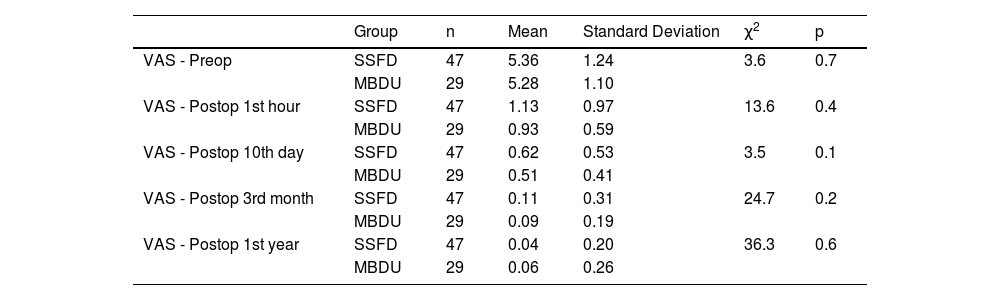
In terms of radicular pain assessment using VAS, the mean preoperative VAS score was 5.8 in the SSFD group and 1.4 at postoperative 1 hour, 1.2 at postoperative day 10, 0.8 at 3 months, and 0.2 at 1 year. In the MBDU group, the mean preoperative VAS score was 6.2 and 1.2 at postoperative 1 hour, 1.1 at postoperative day 10, 0.8 at 3 months, and 0.1 at 1 year. No significant difference was observed between the groups (Table 2) (Fig. 2).
VAS assessment for radicular pain.
| Group | n | Mean | Standard Deviation | χ2 | p | |
|---|---|---|---|---|---|---|
| VAS - Preop | SSFD | 47 | 5.36 | 1.24 | 3.6 | 0.7 |
| MBDU | 29 | 5.28 | 1.10 | |||
| VAS - Postop 1st hour | SSFD | 47 | 1.13 | 0.97 | 13.6 | 0.4 |
| MBDU | 29 | 0.93 | 0.59 | |||
| VAS - Postop 10th day | SSFD | 47 | 0.62 | 0.53 | 3.5 | 0.1 |
| MBDU | 29 | 0.51 | 0.41 | |||
| VAS - Postop 3rd month | SSFD | 47 | 0.11 | 0.31 | 24.7 | 0.2 |
| MBDU | 29 | 0.09 | 0.19 | |||
| VAS - Postop 1st year | SSFD | 47 | 0.04 | 0.20 | 36.3 | 0.6 |
| MBDU | 29 | 0.06 | 0.26 |
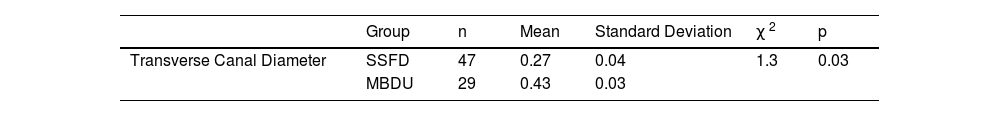
In the preoperative and postoperative 3-month lumbar MRI imaging, the mean ratio of transverse canal diameter at the segment that underwent decompression for ASD was 0.27 in the SSFD group and 0.43 in the MBDU group. A significant difference was observed between the groups in terms of this value (p = 0.03) (Table 3).
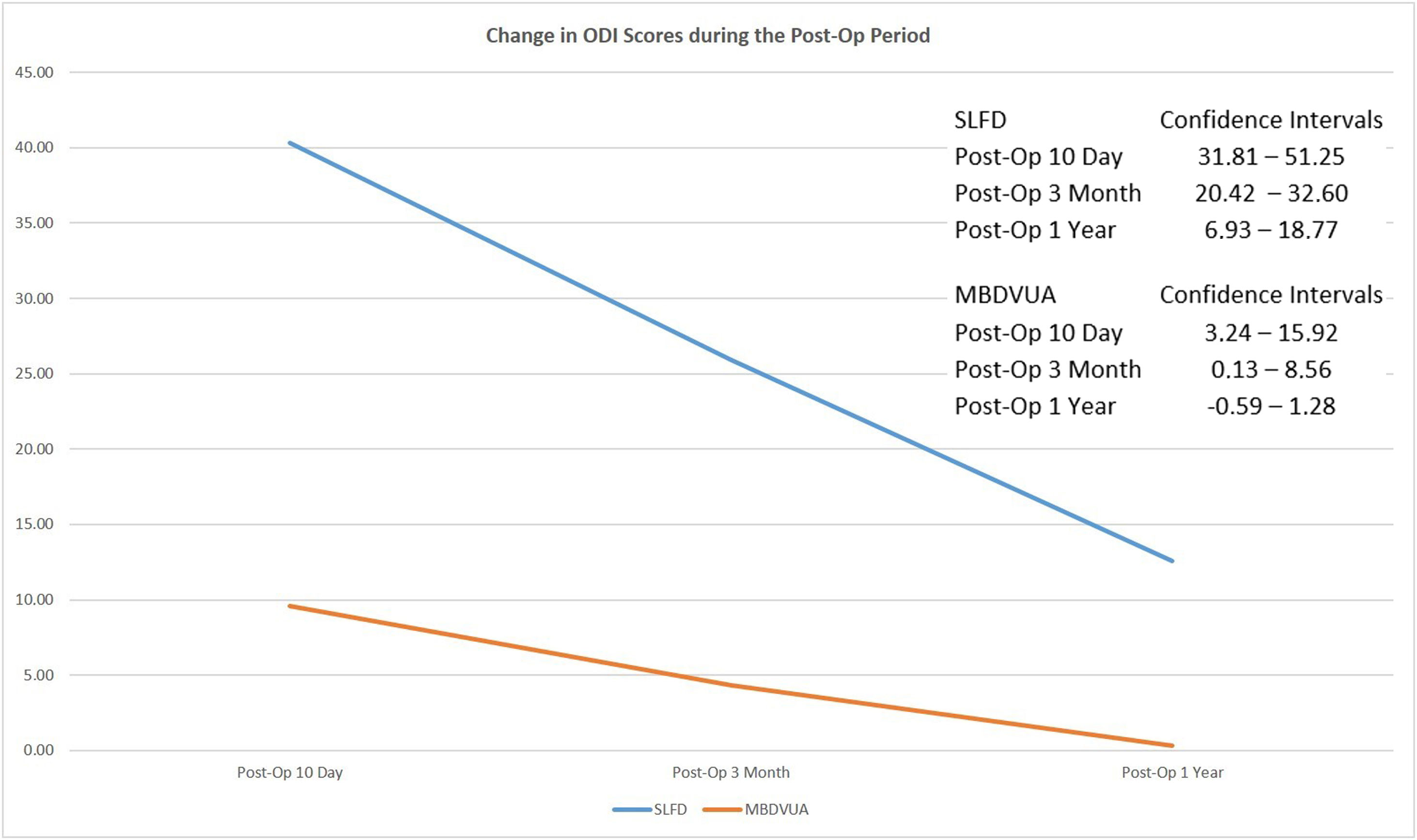
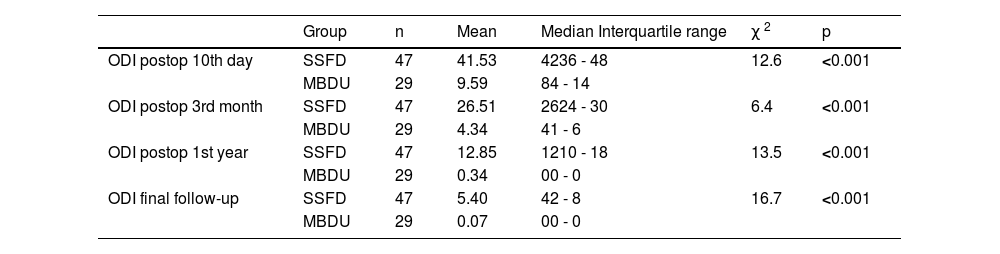
In terms of ODI assessment, in the SSFD group, the mean ODI score was observed as 42 on day 10, 38 at 3 months, 24 at 1 year, and 22 at the final follow-up. In the MBDU group, the mean ODI score was calculated as 18 on day 10, 12 at 3 months, 4 at 1 year, and 4 at the final follow-up. A statistically significant difference was found between the groups in terms of ODI scores (Table4) (Fig. 3).
Analysis of ODI Scores.
| Group | n | Mean | Median Interquartile range | χ 2 | p | |
|---|---|---|---|---|---|---|
| ODI postop 10th day | SSFD | 47 | 41.53 | 4236 - 48 | 12.6 | <0.001 |
| MBDU | 29 | 9.59 | 84 - 14 | |||
| ODI postop 3rd month | SSFD | 47 | 26.51 | 2624 - 30 | 6.4 | <0.001 |
| MBDU | 29 | 4.34 | 41 - 6 | |||
| ODI postop 1st year | SSFD | 47 | 12.85 | 1210 - 18 | 13.5 | <0.001 |
| MBDU | 29 | 0.34 | 00 - 0 | |||
| ODI final follow-up | SSFD | 47 | 5.40 | 42 - 8 | 16.7 | <0.001 |
| MBDU | 29 | 0.07 | 00 - 0 |
In the SSFD group, screw fracture was detected in 1 patient and low back pain secondary to loosening was detected in 4 patients, and these 5 patients were reoperated and their instruments were removed.
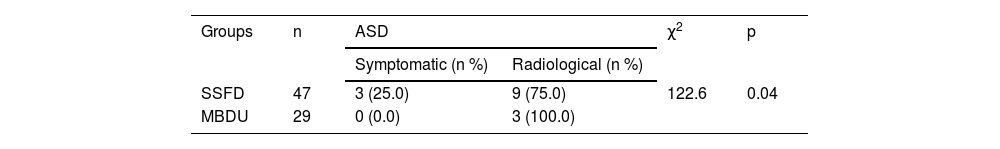
During an average follow-up period of 3 years, symptomatic ASD was observed in three cases (requiring reoperation), whereas radiological ASD was observed in nine cases in the SSFD group. Conversely, none of the 29 cases treated with MBDU exhibited symptomatic ASD during this period. This difference was statistically significant (p = 0.04) (Table 5). But radiological ASD was observed in three cases in the MBDU group also.
DiscussionIn cases of lumbar degenerative diseases where conservative treatment fails to yield results, spinal fusion has commonly been used as a surgical method that can often produce satisfactory outcomes.22,23 However, this method may lead to ASD in some cases during the postoperative period due to increased biomechanical stress on the adjacent segments caused by lumbar arthrodesis.24 Symptomatic ASD often leads to worsened clinical outcomes and the need for new surgical interventions.24
The decision regarding additional surgical interventions in cases unresponsive to conservative treatment is contentious. In cases where ASD develops, various surgical interventions can be performed, including extending the instrumentation with decompression, performing short-level stabilization at the adjacent segment after instrumentation removal, conducting minimally invasive decompression after instrumentation removal, or performing minimally invasive decompression without removing the instrumentation.1–11 Since minimally invasive decompression of the adjacent segment without extending or removing the instruments would not eliminate lumbar pain syndrome secondary to instrumentation and would cause confusion in the comparison between SSFD and MBDU methods, the study was planned and conducted only in cases in which the instrumentation was removed and additional intervention was performed.
There have been studies in the literature regarding the development of ASD following short-segment fixation and decompression applied to the pathological segment.9–11 In the present study, during the 3-year follow-up period, new symptomatic ASD was observed in 6.80% of cases treated with SSFD and radiological ASD development was observed in 19.15% of cases. Conversely, no new symptomatic ASD was observed in the MBDU group, whereas radiological ASD was observed in 10.34% of the patients. In cases where ASD is the primary concern, SSFD surgery carrying the risk of new ASD development can lead to further issues in the future. Furthermore, it may include expected complications secondary to fixation surgery such as loosening, instrument fracture, and pull-out. As MBDU does not create additional biomechanical stress, symptomatic ASD is not expected in these cases. However, Telfeian et al. reported a failure rate of 33% at 2 years after transforaminal endoscopic surgery for L5-S1 ASD after fusion in a study published in 2022.1 In our study, although the radiologic ASD rate was not very low in patients who underwent MBDU, it was interesting that no symptomatic ASD was observed. This may be due to the fact that MBDU allows wider decompression compared to endoscopic interventions and does not create additional biomechanical stress on adjacent segments as in instrumentation.
In terms of the duration of hospitalization, it can be said that MBDU is more advantageous compared to SSFD. Since MBDU causes less tissue trauma, it was noted that patients treated with MBDU could be discharged earlier and mobilized on the same day, and this period was longer in the SSFD group (p < 0.001) (Table 1).
In terms of radicular pain, no significant difference was observed between the two groups during postoperative follow-up (Table 2, Fig. 2). Additionally, ODI scores were significantly lower in the MBDU group (Table 4). The fact that it is a minimally invasive method that causes less tissue trauma, does not cause biomechanical stress secondary to fixation, and eliminates the possibility of pseudoarthrosis or loosening may have minimized the occurrence and severity of lumbar pain syndrome in the MBDU group.
Canal diameter ratios measured in the decompressed segment in preoperative and postoperative lumbar MRI were observed to be low in the SSFD applied group. This data shows that more extensive decompression is performed in SSFD than in MBDU. These results were thought to be due to the opportunity to perform wider decompression with facet resection in SSFD. Protecting the facets in order to avoid instability in MBDU may have caused the decompression to appear to be more inadequate than in SSFD. However, no clinical symptoms secondary to inadequate decompression were observed in the MBDU group during the 3-year follow-up.
Limitation of studyAs authors, we are aware that our study has some limitations. One of the limitations may be the relatively small number of cases in the groups. However, the results are clear that MBDU seems to be much more advantageous than SSFD in both groups at postoperative follow-up, especially in terms of ODI index and new ASD development. Therefore, it can be assumed that the results would not have been essentially different if more patients had been included.
Secondly, the homogeneity of the groups and the retrospective nature of the study may be questioned due to the fact that only one technique was used in one of the centers and the other technique was used in the other. In this sense, we believe that new prospective studies to be performed in a single center and, if possible, with cases operated by the same surgical team may provide more detailed results.
ConclusionThis is the first comparison of these two techniques after instrument removal in ASD cases in the literature. In selected cases with ASD after fusion surgery, without signs of instability, spinal deformities, or ASD at the spinal transition zones, MBDU after instrumentation removal can be considered as a minimally invasive option that does not exacerbate postoperative lumbar pain syndrome or trigger the development of new ASD.
CRediT authorship contribution statement- •
Study conception and design: TK, AK.
- •
Data collection: TK, AK.
- •
Analysis and interpretation of results: TK.
- •
Draft manuscript preparation: AK & TK.
- •
Critical revision of the article: TK, AK.
- •
Other (study supervision, fundings, materials, etc…): TK.
- •
All authors reviewed the results and approved the final version of the manuscript.
None.