To describe the specific surgical details and report the lessons learned with a series of patients suffering from spinal tumours that underwent total en bloc spondylectomy (TES).
MethodsA retrospective case series review is presented, together with an analysis of the clinical and technical variables, as well as the outcomes.
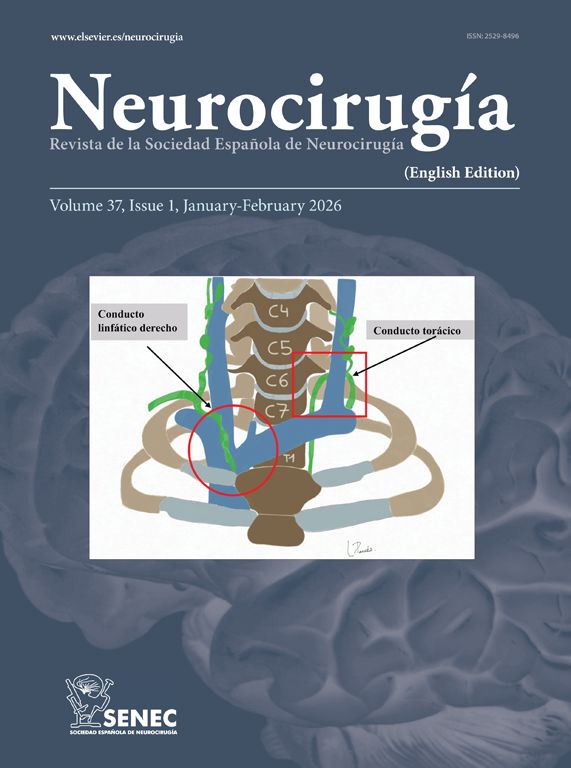
ResultsA total of 10 patients underwent TES (2000–2016) for primary (osteosarcoma, chondrosarcoma, fibrosarcoma and chordoma) and secondary spinal tumours (lung, breast, thyroid, oesophagus, and meningioma metastases). According to the Tomita classification, 2 patients had intra-compartmental tumours, and the rest presented as extra-compartmental. All patients experienced an improvement in their pain level after surgery. Nine patients preserved ambulation post-operatively and one patient developed paraplegia. Six patients needed subsequent operations for wound debridement, tumour recurrence, or revision of the fixation. Other complications included pneumothorax, pleural effusion and venous thrombosis. Four patients remain alive (4 months to 15 years follow-up). The rest died due to primary tumour progression (6.5 months to 12 years). A detailed description of the surgical steps, tips, and pitfalls is provided. Modifications of the technique and adjuncts to resection are commented on. Observation of some considerations (selection of candidates, careful blunt vertebral dissection, strict blood loss control, careful handling of the spinal cord, and maintenance of the radical resection concept at all stages) is key for a successful operative performance.
ConclusionTES is a paradigmatic operation, in which the concept of radical resection provides functional effectiveness and improves survival in selected patients suffering from spinal tumours. Our preliminary experience allows us to highlight some specific and relevant features, especially those favouring a simpler and safer operation.
Describir detalles quirúrgicos específicos y comentar algunas lecciones aprendidas, a partir de una serie de pacientes con tumores vertebrales a los que se les practicó una vertebrectomía total en bloque (VTB).
MétodosPresentamos una serie retrospectiva de casos. Se analizan variables clínicas, técnicas y de resultado.
ResultadosSe intervinieron 10 pacientes (2000-2016) mediante VTB por tumor primario vertebral (osteosarcoma, condrosarcoma, fibrosarcoma y cordoma) o secundario (pulmón, mama, tiroides, esófago y meningioma). Según la clasificación de Tomita, 2 pacientes presentaban lesiones intracompartimentales y el resto extracompartimentales. Todos los pacientes mejoraron del dolor tras la cirugía. Nueve pacientes conservaron la capacidad de caminar en el postoperatorio y uno desarrolló paraplejía. Seis pacientes precisaron reoperaciones por desbridamiento de la herida quirúrgica, recidiva o revisión de la fijación. Otras complicaciones fueron neumotórax, derrame pleural y trombosis venosa. Cuatro pacientes sobreviven (tras 4 meses y hasta 15 años). El resto fallecieron por progresión del tumor primario (de 6,5 meses a 12 años). Se realiza una descripción detallada de los pasos quirúrgicos, consejos y dificultades de la técnica. Se comentan ciertas modificaciones de la técnica y otras cuestiones relativas a la resección. El respeto a ciertas consideraciones (selección de los candidatos, disección vertebral cuidadosa, control estricto del sangrado, manejo cuidadoso de la médula y mantenimiento del concepto de resección radical en todo momento) es clave para realizar con éxito esta intervención.
ConclusiónLa VTB es una intervención paradigmática en la que el concepto de resección radical implica efectividad funcional y mejora la supervivencia en pacientes seleccionados portadores de tumores vertebrales. Esta experiencia preliminar nos permite destacar algunas de sus características relevantes, especialmente aquellas dirigidas a simplificar la técnica y hacerla más segura.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.