Current treatment of cervical spine spondylodiscitis generally involves a radical surgical debridement and stable reconstruction together with antibiotic therapy until complete healing. But this classical approach could be difficult for patients who have been treated previously for an esophageal carcinoma and received radiotherapy.
We present a case of a 75-year-old male who underwent an esophageal dilation procedure and developed afterward a spondylodiscitis with epidural abscess due to a neglected esophageal perforation. Blood cultures were positive for Peptostreptococcus. Cervical spondylodiscitis and epidural abscess are extremely rare complications of esophageal dilations. Successful treatment without debridement was achieved by performing a posterior fixation without decompression associated with antibiotic therapy for 8 weeks. The present case highlights that spondylodiscitis and epidural abscess may be treated in selected cases where the anterior neck is unapproachable and with a recognized pathogen by a posterior approach fixation without debridement, in association to specific antibiotic therapy.
El tratamiento actual de la espondilodiscitis de la columna cervical implica generalmente un desbridamiento quirúrgico radical y una reconstrucción estable junto con un tratamiento antibiótico hasta la curación completa. Pero este enfoque clásico puede resultar difícil para pacientes que han sido tratados previamente por un carcinoma de esófago y han recibido radioterapia.
Presentamos el caso de un varón de 75 años a quien se le realizó un procedimiento de dilatación esofágica y posteriormente desarrolló una espondilodiscitis con absceso epidural debido a una perforación esofágica desapercibida. Los hemocultivos fueron positivos para Peptostreptococcus. La espondilodiscitis cervical y el absceso epidural son complicaciones extremadamente raras de las dilataciones esofágicas. El tratamiento exitoso sin desbridamiento se logró mediante la realización de una fijación posterior sin descompresión asociada a terapia con antibióticos durante 8 semanas. El presente caso destaca que la espondilodiscitis y el absceso epidural pueden tratarse en casos seleccionados donde la región cervical anterior es inaccesible y con un patógeno reconocido mediante una fijación posterior sin desbridamiento ni descompresión, asociado a una terapia antibiótica específica.
Esophageal stenosis is a common complication of laryngeal cancer treatments,1 commonly requiring repeated bougie dilations. Esophageal perforations are rare (0.04−0.40%).2 Subsequent spondylodiscitis and epidural abscess are even rarer, exceptionally reported, with only few cases in the literature to our knowledge. The treatment of this condition, in this selected group of patients, where it is usual to have anterior neck soft tissue problems due to previous surgical approaches and radiation therapy, can become a challenge for the surgeon, limiting the usual management of other causes of spondylodiscitis where an anterior approach debridement and fixation would surely be the first option. We present the first case published, to the best of our knowledge, of successful treatment by posterior fixation and specific intravenous antibiotic therapy.
Case descriptionA 75-year-old male with a history of larynx carcinoma treated with laryngectomy and radiotherapy 30 years earlier, with the consequent deterioration of soft tissues of the anterior neck and progressive esophagus stricture secondary to the treatment, leading to multiple esophageal dilations. Four weeks after an apparently uneventful dilation procedure, the patient consulted at the Emergency Department for neck stiffness, pain and fever. At admission in the infectious disease department, he presented weakness to left shoulder abduction (M:3/5). Leukocytosis (18,690/mL) and elevated C-reactive-protein (25.55 mg/dl, normal <1 mg/dl) were remarkable. Lumbar puncture showed hypoglycorrhachia (3 mg/dl) and an elevated protein count (883 mg/dl). Blood cultures were positive for Peptostreptococcus. Bacterial meningitis was the initial diagnosis in the medical department and was treated with antibiotics according to sensitivity without improvement.
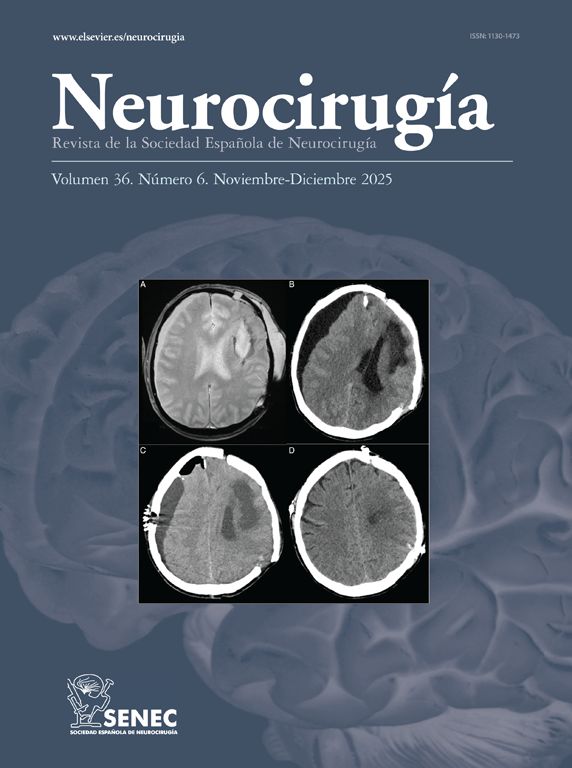
Further image studies were performed. Cervical X-ray showed hypodense areas of C5/C6 vertebral bodies and prevertebral calcification compatible with an abscess (Fig. 1A). Computed tomography (CT) demonstrated a prevertebral collection and a radiolucency of anterior cortical margin of C5-C6 (Fig. 1B). Magnetic resonance imaging (MRI) reported a prevertebral collection with sinus tract from the esophagus, C5/C6 osteomyelitis and an epidural abscess with subarachnoid space occupancy and associated increased uptake of cervicodorsal perimedular ependyma (Fig. 1C). The patient developed a spondylodiscitis and epidural abscess after a previous, four weeks before, neglected esophageal perforation.
A. Cervical lateral radiograph: hypodense lesions of C5/C6 vertebral bodies with slight listhesis from C4 to C5. Prevertebral calcification is compatible with abscess formation and increased anterior soft tissue volume (arrows); B. Cervical lateral computed tomography shows erosion and radiolucency of the anterior aspect of C5/C6 vertebral bodies (arrow); C and D. Cervical sagittal T2 and STIR weighted contrast magnetic resonance showing prevertebral collection, increased prevertebral space (double arrow) associated with osteomyelitic signs in the C5/C6 vertebrae, sinus tract from the esophagus and epidural abscess with mild obliteration signs of the spinal cord (arrow).
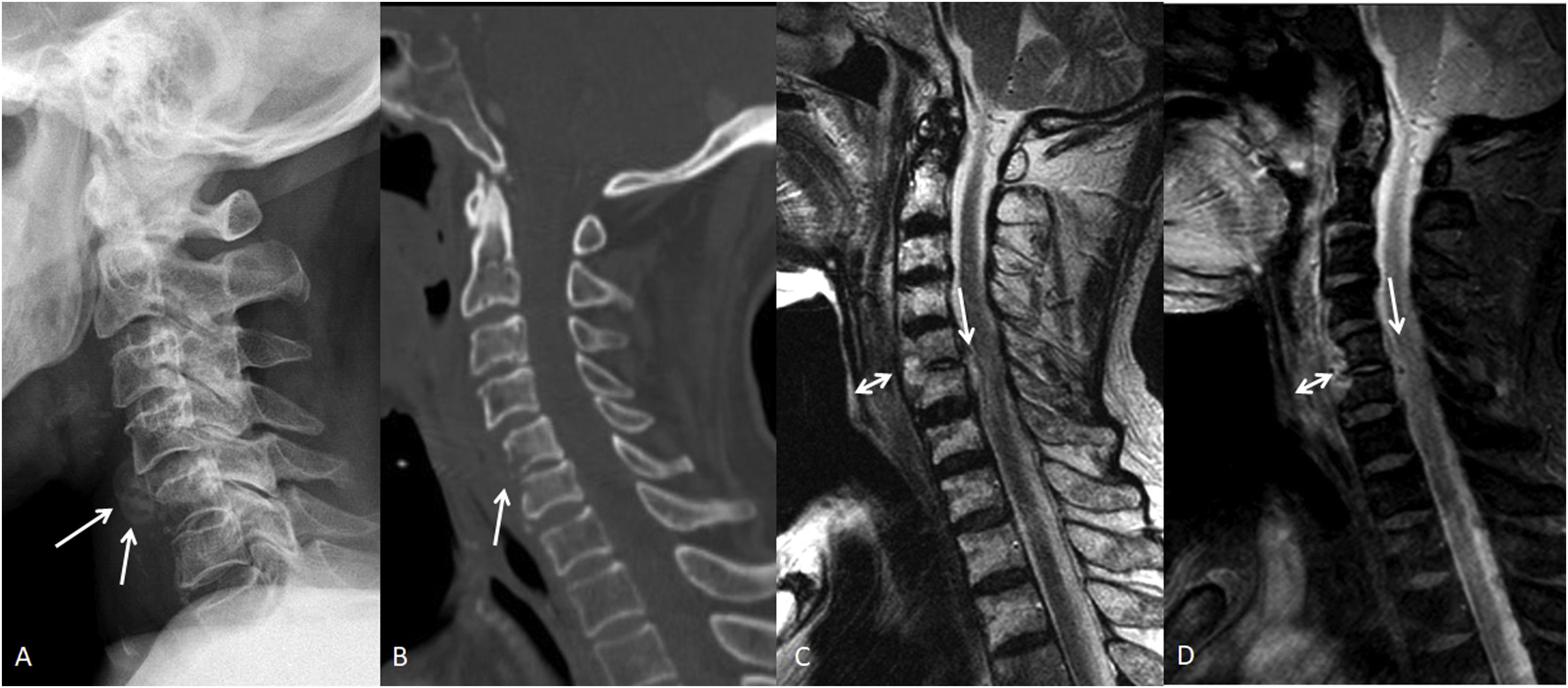
Patient received treatment with antibiotics and a Philadelphia collar after his admission. Ten days later, without clinical improvement of shoulder abduction we consider the need for a surgical debridement. Surgical treatment for spondylodiscitis is usually performed through an anterior approach that involves debridement, vertebral body curettage or resection and anterior fixation and fusion. However, in the reported patient, after careful evaluation of the serious soft tissue-damaged state of the anterior neck, the option of doing an anterior approach was discarded. The option of a conservative management with a cervical collar was discarded due to the risk of progressive neurological deterioration. The patient was treated with a posterior approach and fixation by bilateral facet joints C4-C6 and pedicle C7 screws without debridement, associated with 8 weeks of antibiotics. A nasogastric tube was placed in the esophagus for parenteral nutrition during this period although the dilaceration caused by the dilation was probably closed spontaneously. The patient showed progressive improvement, regaining strength in the upper limb (M: 4/5). A 6-month control MRI showed resolution of C5/C6 osteomyelitis and no evidence of abscesses or sinus tracts, although it showed intramedullary expansive high signal (C4-T11), anterior medullary synechiae, and persistent dural and arachnoid enhancement throughout the cord (Fig. 2). After 6 months, total strength was regained without signs of infectious processes after an 8-year follow-up.
A. Lateral cervical radiograph at six months post-operation: posterior fixation with bilateral facet screws at C4-C5-C6 and pedicle screws at C7 six months after surgery; B. MRI at 6 moths post- operation showed resolution of C5/C6 osteomyelitis and no evidence of abscesses or sinus tracts, although it showed intramedullary expansive high signal (C4-T11), anterior medullary synechiae, and persistent dural and arachnoid enhancement throughout the cord.
Management of laryngeal tumors is often complicated by esophageal stricture,3 particularly if radiation therapy has been associated, requiring dilations and causing microtrauma that could induce direct inoculation of intestinal bacteria into adjacent tissues.1 An even more threatening complication is a perforation. The Killian triangle is an anatomically weak area (between the inferior pharyngeal constrictor and the cricopharyngeous muscle) more susceptible to perforations. Its proximity to C4–C6 vertebrae places them at high risk of infection by direct inoculation of bacteria through esophageal perforation.1 Several causes of direct inoculation of bacteria into adjacent tissues of the cervical spine with subsequent infection secondary to esophageal injuries have been reported, such as esophageal diverticulitis, spontaneous rupture,4 complications of stent placements,5 gastrointestinal endoscopies, anterior cervical fusions6 traumatic esophageal injuries7–10 and or surgical procedures as a pharyngolaryngectomy.11
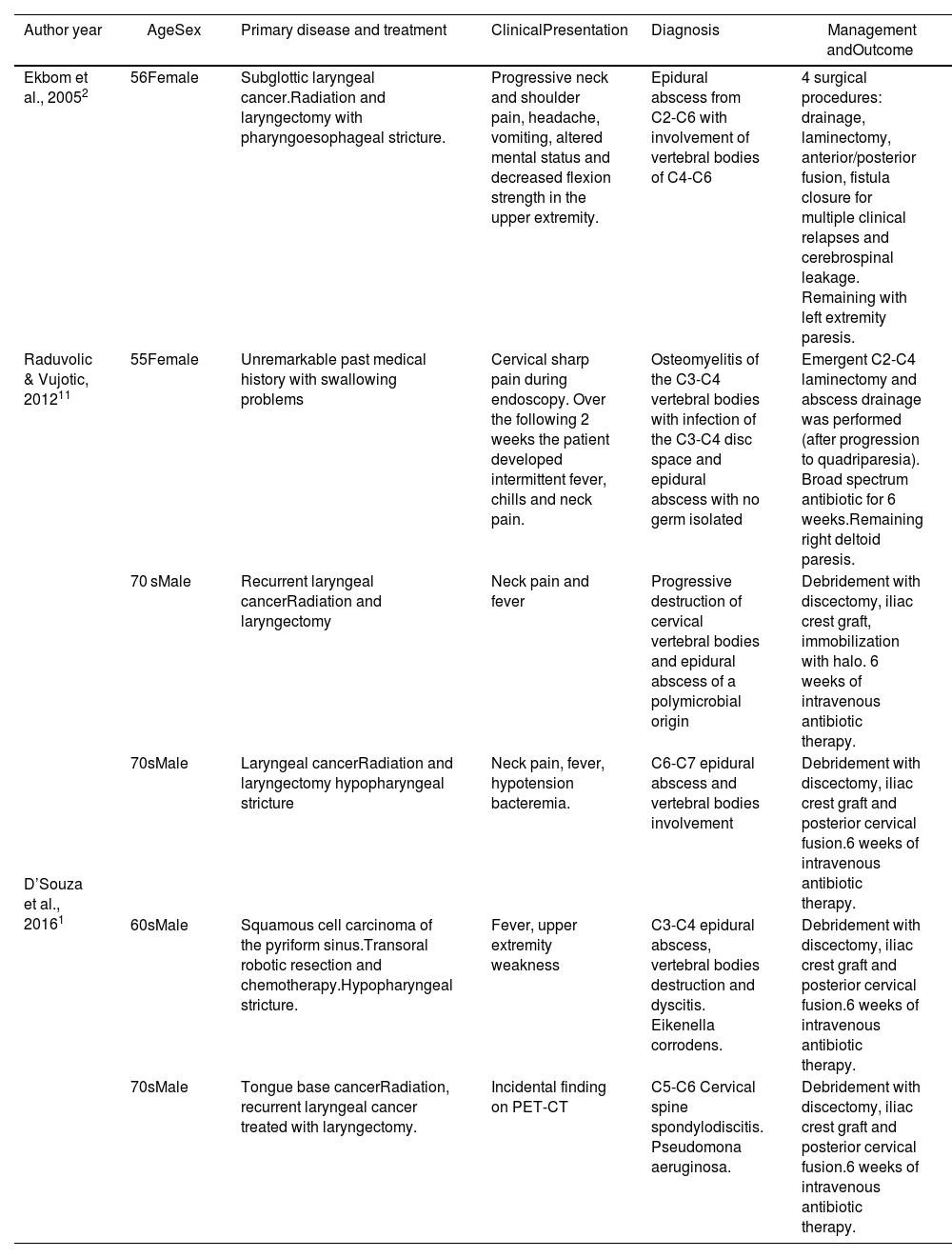
Spondylodiscitis after perforations as a consequence of esophageal dilations is exceptionally described in the literature. Ekbom first reported a case of cervical spondylodiscitis and epidural abscess after a dilation with paresis of an upper extremity, managed with posterior drainage of the abscess that later recurred. Needing further treatment (anterior approach, corpectomy and fusion) nevertheless, cerebrospinal leakage and a persistent fistula developed (Table 1).2
Reported cases of cervical spondylodyscitis or epidural abscess related to esophageal dilations.
| Author year | AgeSex | Primary disease and treatment | ClinicalPresentation | Diagnosis | Management andOutcome |
|---|---|---|---|---|---|
| Ekbom et al., 20052 | 56Female | Subglottic laryngeal cancer.Radiation and laryngectomy with pharyngoesophageal stricture. | Progressive neck and shoulder pain, headache, vomiting, altered mental status and decreased flexion strength in the upper extremity. | Epidural abscess from C2-C6 with involvement of vertebral bodies of C4-C6 | 4 surgical procedures: drainage, laminectomy, anterior/posterior fusion, fistula closure for multiple clinical relapses and cerebrospinal leakage. Remaining with left extremity paresis. |
| Raduvolic & Vujotic, 201211 | 55Female | Unremarkable past medical history with swallowing problems | Cervical sharp pain during endoscopy. Over the following 2 weeks the patient developed intermittent fever, chills and neck pain. | Osteomyelitis of the C3-C4 vertebral bodies with infection of the C3-C4 disc space and epidural abscess with no germ isolated | Emergent C2-C4 laminectomy and abscess drainage was performed (after progression to quadriparesia). Broad spectrum antibiotic for 6 weeks.Remaining right deltoid paresis. |
| D’Souza et al., 20161 | 70 sMale | Recurrent laryngeal cancerRadiation and laryngectomy | Neck pain and fever | Progressive destruction of cervical vertebral bodies and epidural abscess of a polymicrobial origin | Debridement with discectomy, iliac crest graft, immobilization with halo. 6 weeks of intravenous antibiotic therapy. |
| 70sMale | Laryngeal cancerRadiation and laryngectomy hypopharyngeal stricture | Neck pain, fever, hypotension bacteremia. | C6-C7 epidural abscess and vertebral bodies involvement | Debridement with discectomy, iliac crest graft and posterior cervical fusion.6 weeks of intravenous antibiotic therapy. | |
| 60sMale | Squamous cell carcinoma of the pyriform sinus.Transoral robotic resection and chemotherapy.Hypopharyngeal stricture. | Fever, upper extremity weakness | C3-C4 epidural abscess, vertebral bodies destruction and dyscitis. Eikenella corrodens. | Debridement with discectomy, iliac crest graft and posterior cervical fusion.6 weeks of intravenous antibiotic therapy. | |
| 70sMale | Tongue base cancerRadiation, recurrent laryngeal cancer treated with laryngectomy. | Incidental finding on PET-CT | C5-C6 Cervical spine spondylodiscitis. Pseudomona aeruginosa. | Debridement with discectomy, iliac crest graft and posterior cervical fusion.6 weeks of intravenous antibiotic therapy. |
Later, Radulovic reported another case of perforation, causing a rapidly progressive infection, with neurological involvement that underwent drainage of the abscess, with a good outcome after 6 weeks of antibiotics. At two-year follow-up, spontaneous fusion of intervertebral bodies (C2-C4) and paresis of the deltoid muscle were present.12 D’Souza reported 4 cases of cervical spondylodiscitis after reviewing 1221 patients with esophageal dilations; of these, only one had neurological involvement. All were surgically managed with debridement and stabilization.1
Neglecting epidural abscesses related to spondylodiscitis is likely considering its uncommon occurrence and initial subtle symptoms, presenting the classic triad (localized pain, neurologic deficit and fever) only in 37% of the cases.11–14 After onset of neurological symptoms, a rapid progressive compression of neurovascular structures can be expected without rapid intervention.13,14 Although in some series there was no neurological impairment, the incidence of neurological deficit ranges from 40 to 55 % of cervical spondylodiscitis cases reported in the literature.11
Management of spondylodiscitis depends on potential instability, the presence of neurological and progressive symptoms,11 and the overall state of the patient. Conservative management includes intravenous antibiotics based on isolated bacteria, analgesics and cervical bracing.14 Most authors recommend radical debridement, stable reconstruction using anterior only surgery, when needed, and antibiotic therapy. Management of cervical epidural abscesses remains controversial. Most authors recommend immediate decompression and drainage due to the potential risk of expansion, secondary neurological compression and vascular thrombosis. The prognosis of epidural abscesses is inversely proportionate to the duration and severity of symptoms. However, medical management is still a viable option when the infectious germ has been identified, if strict vigilance is ensured.11,15
In the reported case, the usual management would have been to perform an anterior debridement and instrumentation. However, considering the status of the prevertebral cervical skin and soft tissues with fibrosis and adherence related to the history of radiotherapy and surgery, the presence of a traqueostomy, and having identified the infecting bacteria by blood cultures, we decided to perform a posterior cervical instrumentation to stabilize and fix the affected spinal segment and the use of intravenous antibiotic therapy for four weeks that was followed by another 4 weeks of oral antibiotics, obtaining a complete resolution of the infection. An anterior approach, regardless of its difficulty in the case presented, could have been the source of multiple further complications, including greater esophageal perforation.
ConclusionsIn cases of spondylodiscitis and epidural abscess, usual management would be anterior debridement and instrumentation. However, after considering the status of prevertebral cervical tissues with fibrosis, adherences related to the history of radiotherapy and surgery, the presence of traqueostomy, and identified infecting bacteria, a posterior fixation without anterior debridement and intravenous antibiotic specific therapy can could be a successful treatment.
Ethics approvalThis study was performed in line with the principles of the Declaration of Helsinki.
Consent to participateAccording to Institutional Review Board, the informed consent is not required.
Consent for publicationAuthors consent to publish this report in NEUROCIRUGIA (ASTUR).
Conflicts of interestThe authors have no relevant financial or non-financial interests to disclose.
FundingThis research did not receive specific support from public sector agencies, the commercial sector, or non-profit organizations.
Availability of data and materialNot applicable. All data are in the text
Code availabilityNot applicable.
Authors' contributionsAll authors contributed equally to this paper.