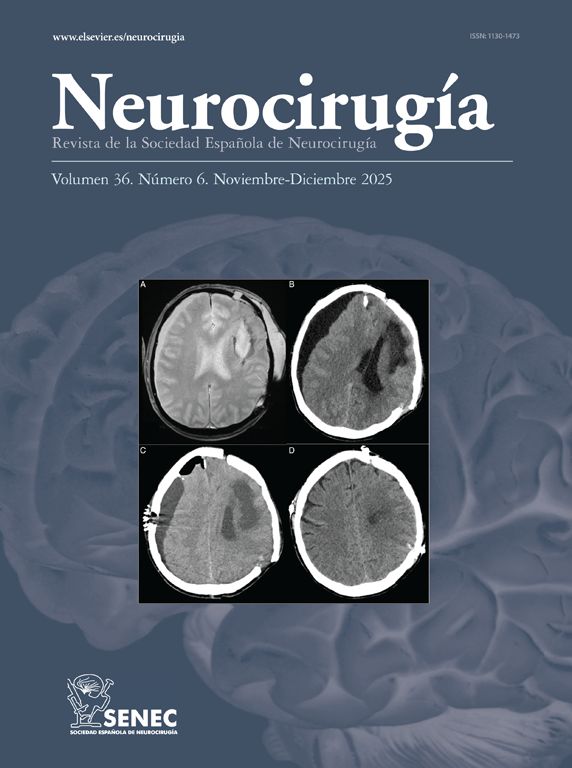
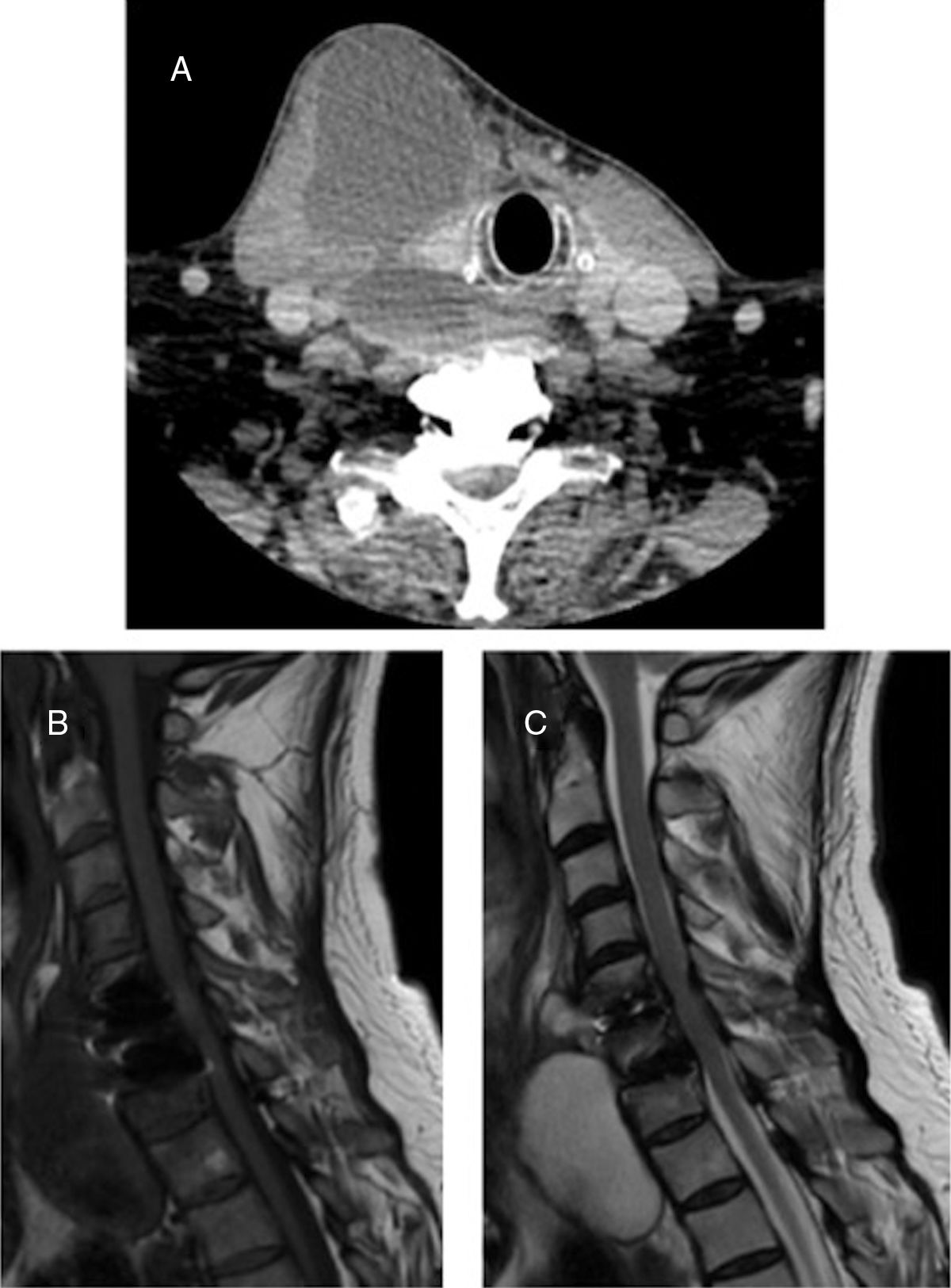
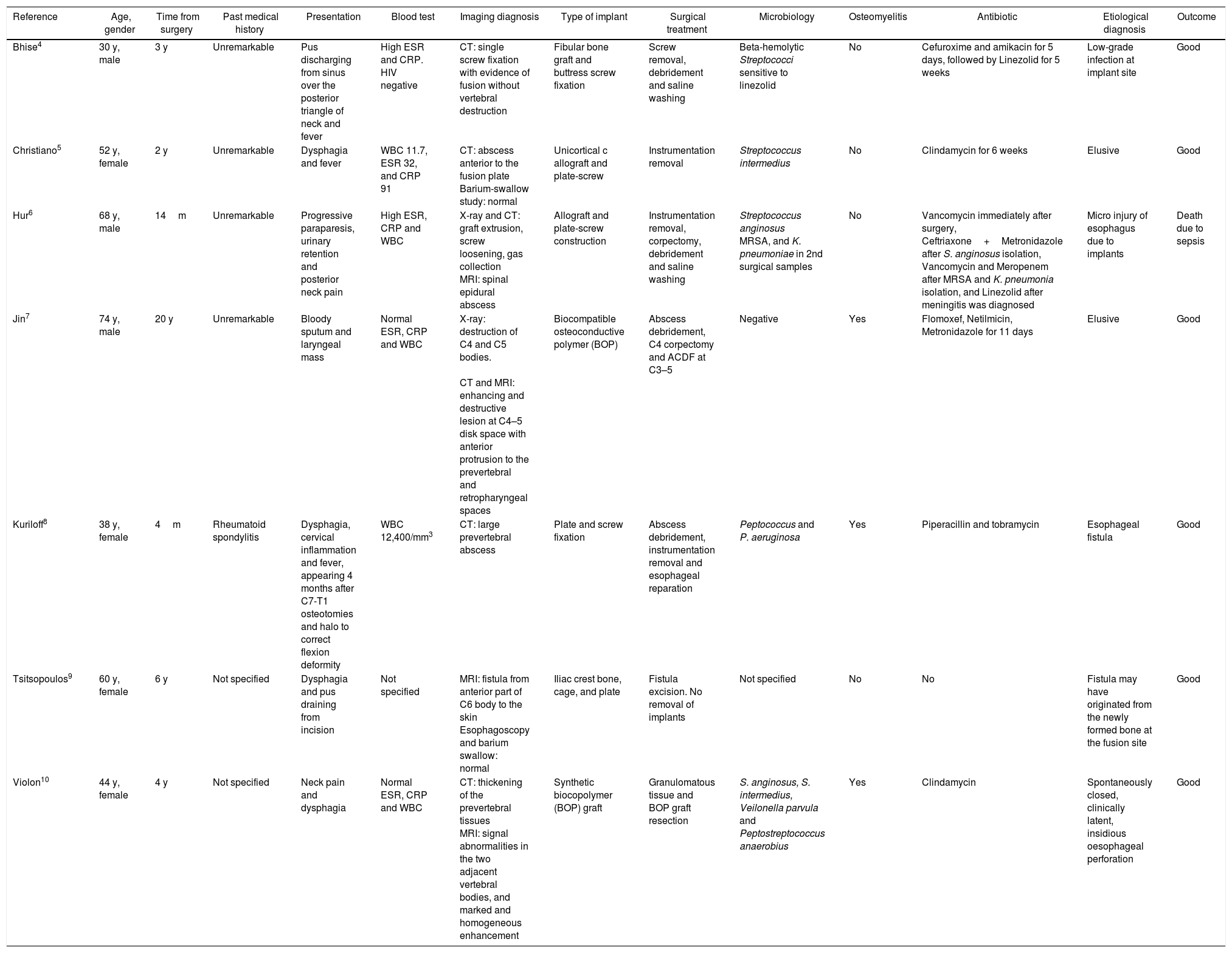
Anterior cervical discectomy has a low non-mechanical complication rate. In our literature review, we found 7 cases of delayed surgical site infection. We report a case of cervical prevertebral abscess due to Propionibacterium acnes 2 years after discectomy and arthroplasty, with a beta-2-transferrin false positive test as a complementary highlighted finding. We discuss the diagnosis and etiology of this rare delayed infectious complication.
La discectomía cervical anterior tiene una baja tasa de complicaciones no mecánicas. En la revisión de la literatura, encontramos 7 casos de infección diferida del sitio quirúrgico. Presentamos un caso de absceso cervical prevertebral secundario a Propionibacterium acnes 2 años después de la cirugía, asociado a un falso positivo del test de beta-2-transferrina como hallazgo complementario a destacar, y discutimos el diagnóstico y la etiología de esta rara complicación infecciosa diferida.
Artículo

Si es la primera vez que accede a la web puede obtener sus claves de acceso poniéndose en contacto con Elsevier España en suscripciones@elsevier.com o a través de su teléfono de Atención al Cliente 902 88 87 40 si llama desde territorio español o del +34 932 418 800 (de 9 a 18h., GMT + 1) si lo hace desde el extranjero.
Si ya tiene sus datos de acceso, clique aquí.
Si olvidó su clave de acceso puede recuperarla clicando aquí y seleccionando la opción "He olvidado mi contraseña".