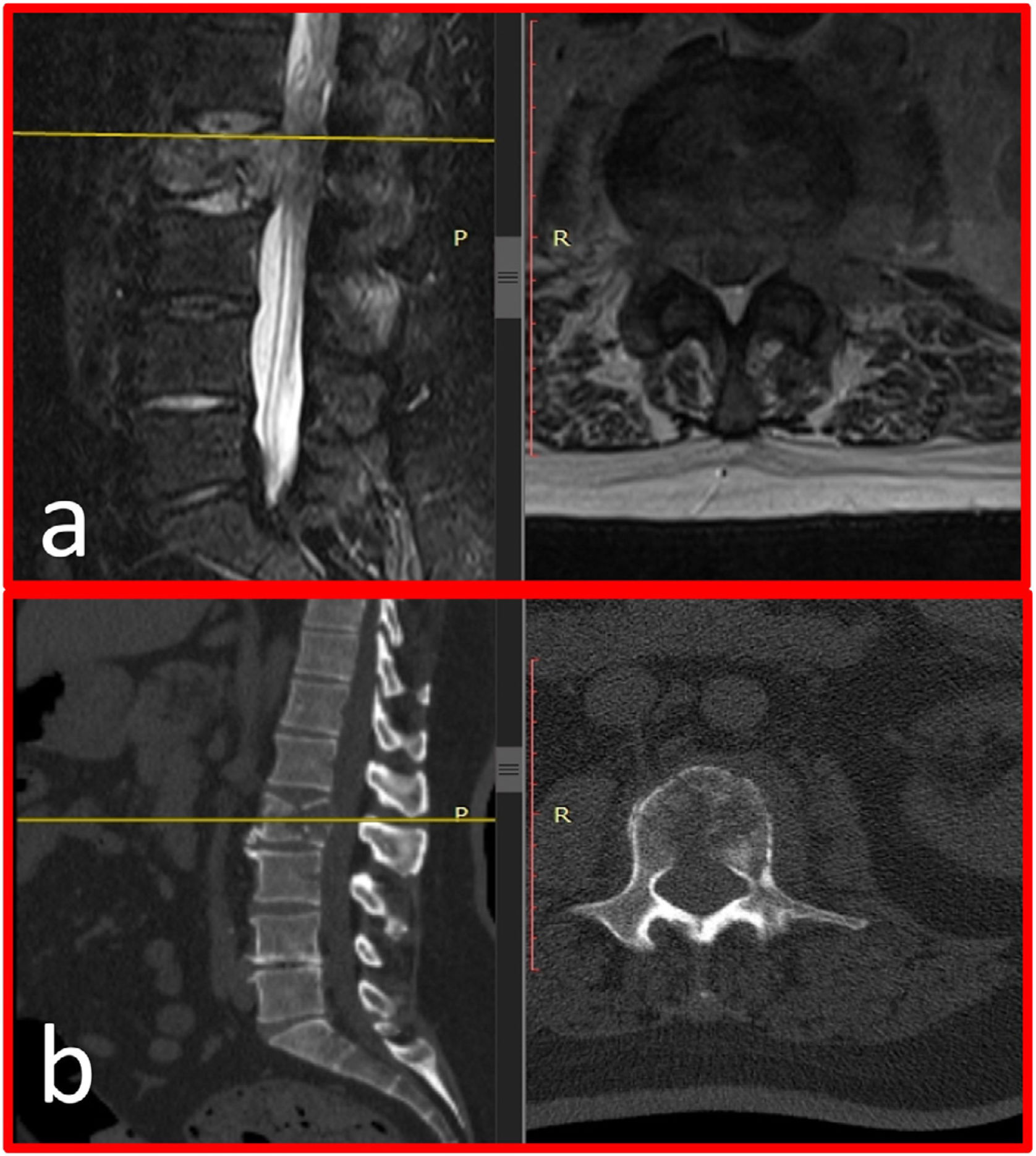
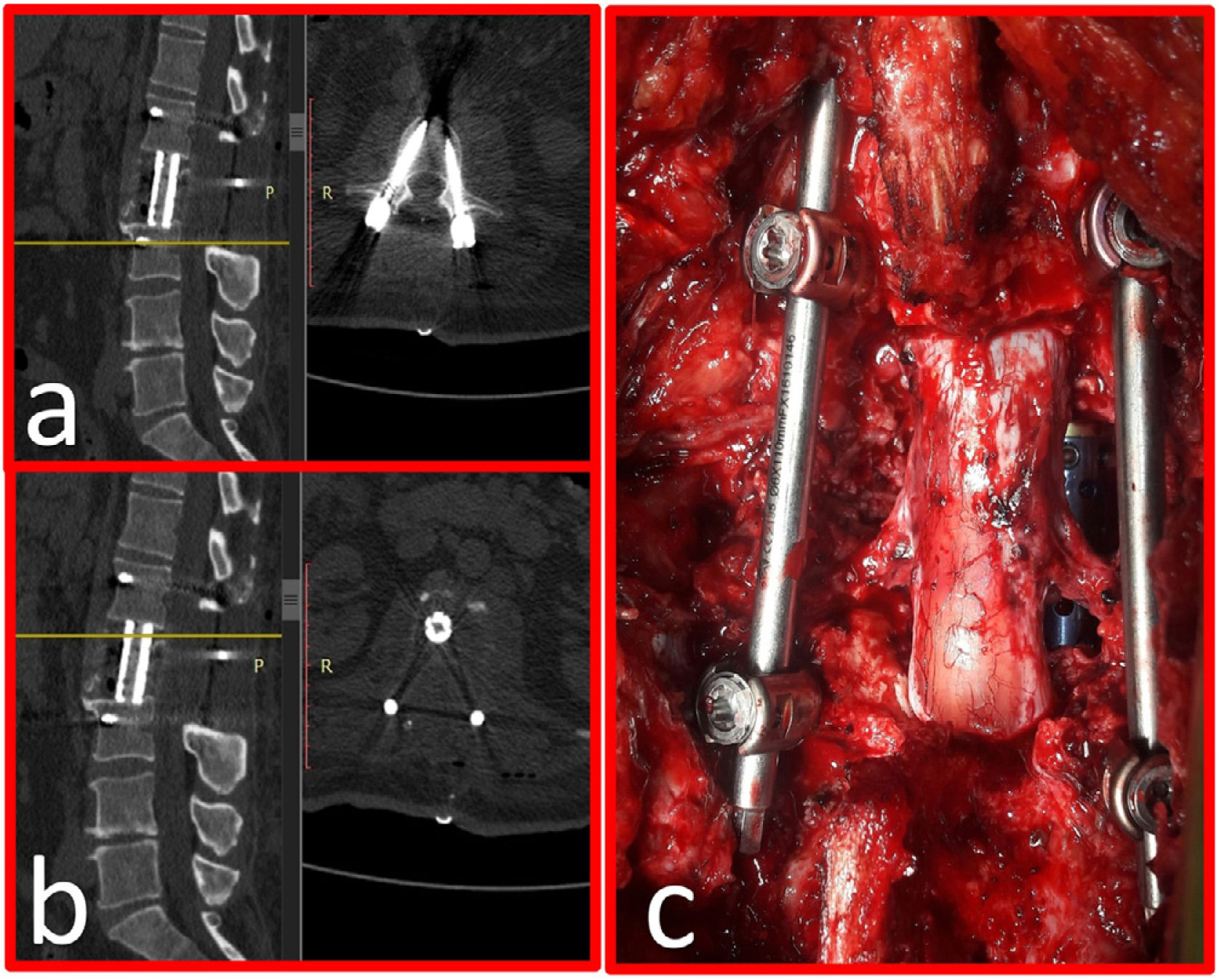
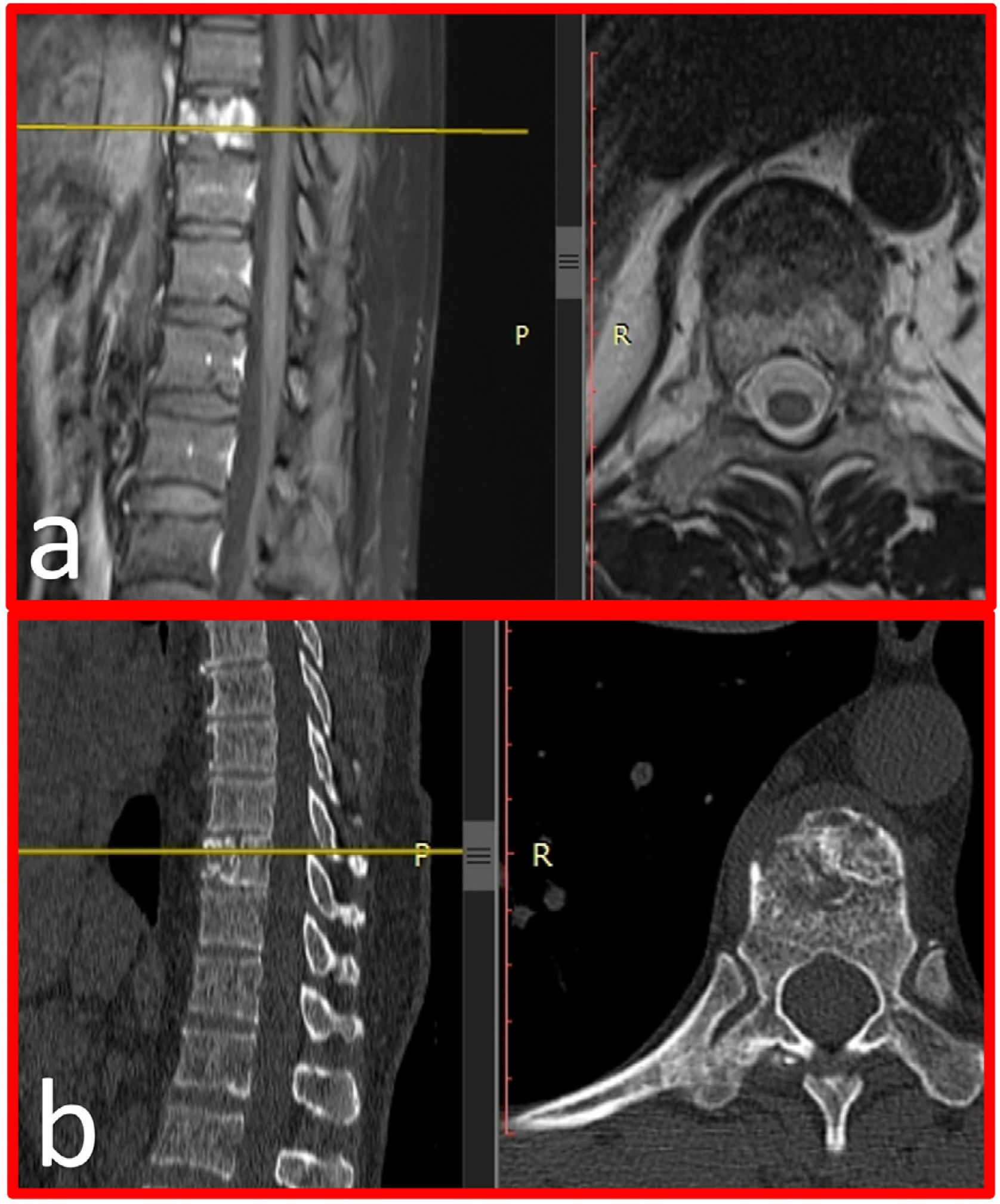
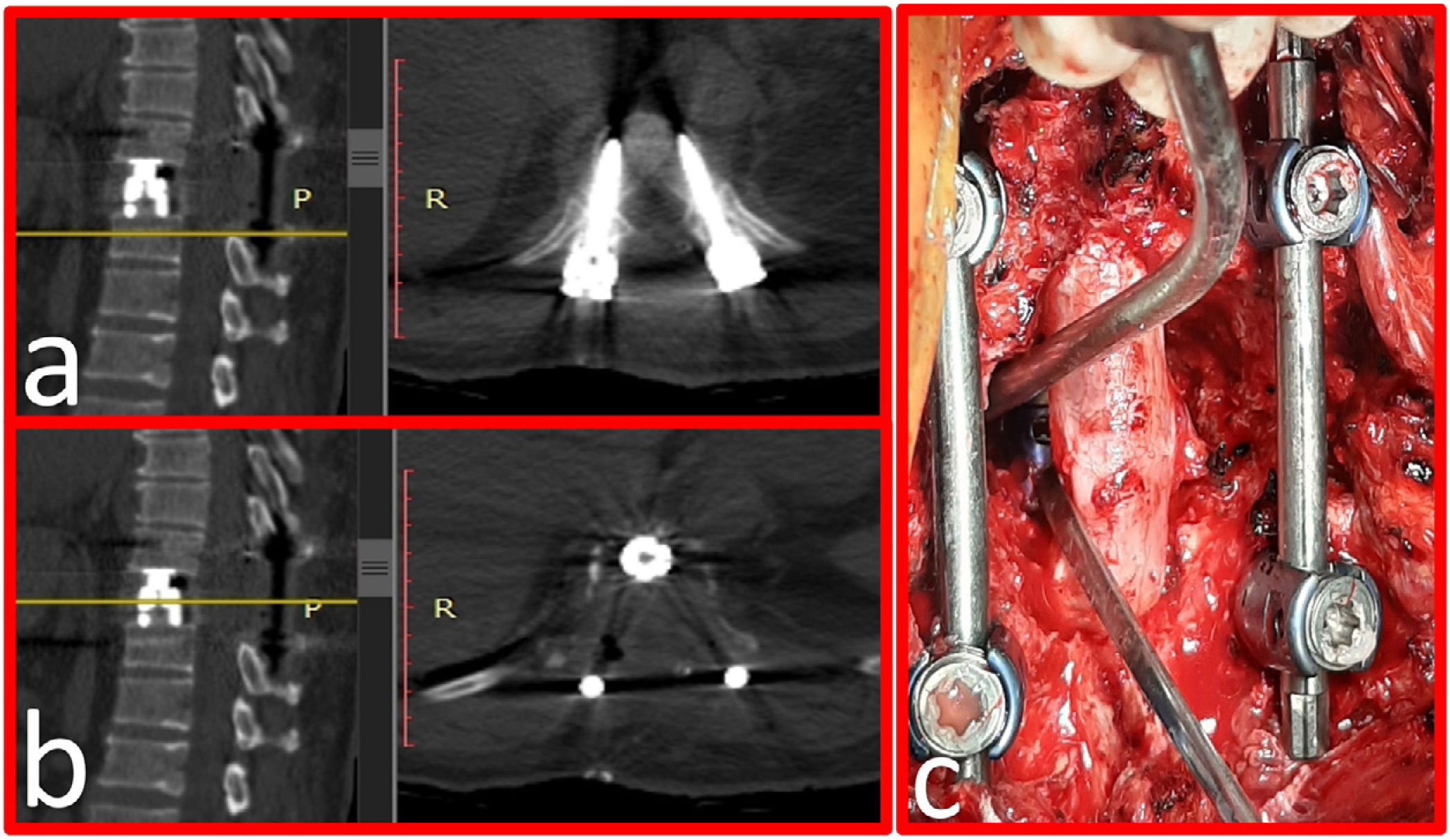
The surgical treatment of spinal metastases is mostly palliative in nature and focuses on improving the quality of life of patients. The posterior transpedicular surgical approach provides circumferential 360° decompression, allows reconstruction and stabilisation to be achieved in a single session and can be performed using an open, mini-open or minimally invasive approach. We present and discuss the surgical techniques and outcomes for patients with single-level metastatic spinal disease and in poor general condition who underwent surgery via the posterior-only transpedicular corpectomy approach and reconstruction with expandable corpectomy cages.
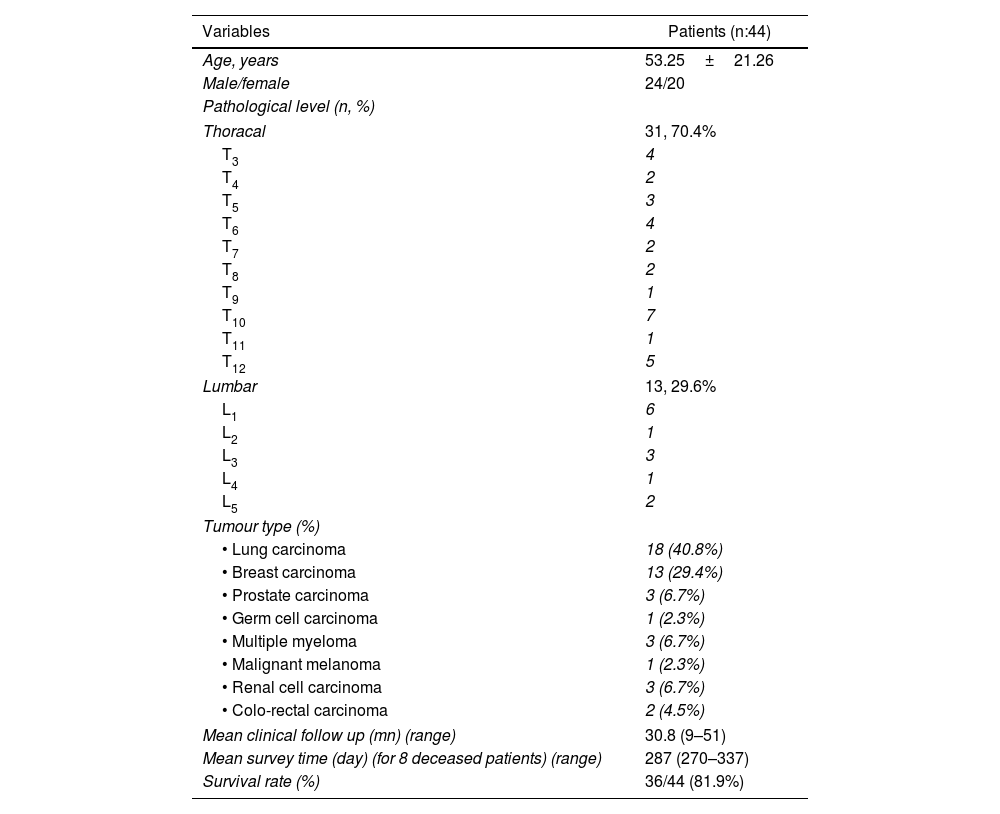
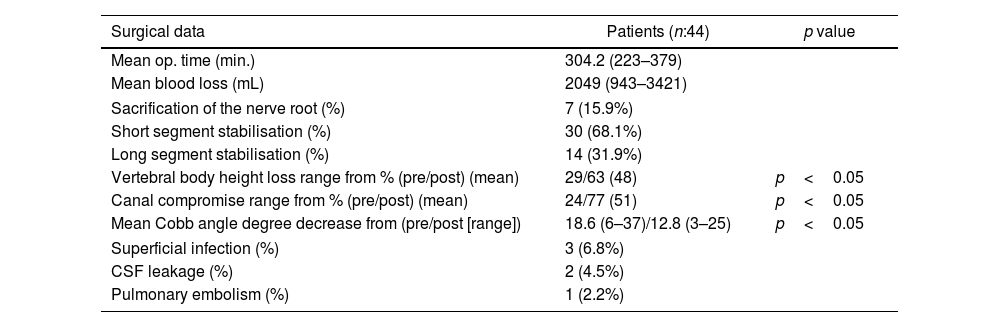
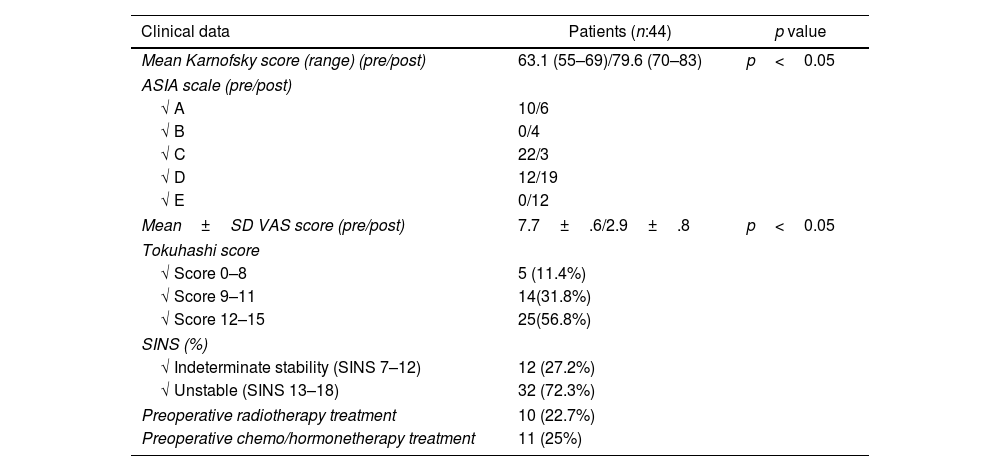
MethodsPatients with a single level thoracolumbar metastatic disease (T3-L5) and a Karnofsky score of ≤70, who underwent a complete posterior transpedicular corpectomy with expandable cage reconstruction of the anterior spinal column were retrospectively reviewed. Patients’ demographics, SINS, modified Tokuhashi scores as well as preoperative and postoperative ASIA scale, Karnofsky scores, VAS scores and vertebral height/Cobb angle values were analysed.
ResultsA total of 44 patients (24 M/20 F) (mean age 53.25±21.26 years) met the inclusion criteria. The modified Tokuhashi scores were as follows: score 0–8, 5 (11.4%) patients; score 9–11, 14 (31.8%) patients; and score 12–15, 25 (56.8%) patients. There were significant improvements in the postoperative VAS scores (mean 7.7–2.9), Karnofsky scores (mean 63.3–79.6) as well as the Cobb angles (18.6–12.8°) and vertebral height. Thirtyfive patients showed improved neurological function by at least one ASIA grade, whereas 9 showed no improvement during the postoperative period.
ConclusionsThis technique, which has a low complication rate and a short recovery time, can help achieve satisfactory results even in patients with poor metabolic profiles and Karnofsky scores in the preoperative period. Further clinical studies with large patient groups are warranted to confirm the results of this study.
El tratamiento quirúrgico de las metástasis espinales es principalmente de naturaleza paliativa y se enfoca en mejorar la calidad de vida de los pacientes. El abordaje quirúrgico transpedicular posterior proporciona una descompresión circunferencial de 360°, permite lograr la reconstrucción y estabilización en una sola sesión y se puede realizar mediante un abordaje abierto, miniabierto o mínimamente invasivo. Presentamos y discutimos las técnicas quirúrgicas y los resultados para pacientes con enfermedad espinal metastásica de un solo nivel, y en mal estado general, que se sometieron a cirugía mediante el abordaje de corpectomía transpedicular solo posterior y reconstrucción con jaulas de corpectomía expandibles.
MétodosSe revisaron retrospectivamente pacientes con una enfermedad metastásica toracolumbar de un solo nivel (T3-L5) y una puntuación de Karnofsky≤70, que se sometieron a una corpectomía transpedicular posterior completa con reconstrucción de la columna anterior con jaula expandible. Se analizaron los datos demográficos de los pacientes, SINS, las puntuaciones de Tokuhashi modificadas, así como la escala ASIA preoperatoria y posoperatoria, las puntuaciones de Karnofsky, las puntuaciones VAS y los valores de altura vertebral/ángulo de Cobb.
ResultadosUn total de 44 pacientes (24 M/20 F) (edad media 53,25±21,26 años) cumplieron los criterios de inclusión. Las puntuaciones de Tokuhashi modificadas fueron las siguientes: puntuación de 0 a 8, 5 (11,4%) pacientes; puntuación 9-11, 14 (31,8%) pacientes; y puntuación 12-15, 25 (56,8%) pacientes. Hubo mejoras significativas en las puntuaciones VAS postoperatorias (media de 7,7 a 2,9), las puntuaciones de Karnofsky (media de 63,3 a 79,6), así como los ángulos de Cobb (18,6° a 12,8°) y la altura vertebral. Treinta y cinco pacientes mostraron una función neurológica mejorada en al menos un grado ASIA, mientras que 9 no mostraron mejoría durante el período postoperatorio.
ConclusionesEsta técnica, que tiene una tasa de complicaciones baja y un tiempo de recuperación corto, puede ayudar a lograr resultados satisfactorios incluso en pacientes con perfiles metabólicos y puntuaciones de Karnofsky deficientes en el período preoperatorio. Se justifican más estudios clínicos con grandes grupos de pacientes para confirmar los resultados de este estudio.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.