Anterior cervical discectomy has a low non-mechanical complication rate. In our literature review, we found 7 cases of delayed surgical site infection. We report a case of cervical prevertebral abscess due to Propionibacterium acnes 2 years after discectomy and arthroplasty, with a beta-2-transferrin false positive test as a complementary highlighted finding. We discuss the diagnosis and etiology of this rare delayed infectious complication.
La discectomía cervical anterior tiene una baja tasa de complicaciones no mecánicas. En la revisión de la literatura, encontramos 7 casos de infección diferida del sitio quirúrgico. Presentamos un caso de absceso cervical prevertebral secundario a Propionibacterium acnes 2 años después de la cirugía, asociado a un falso positivo del test de beta-2-transferrina como hallazgo complementario a destacar, y discutimos el diagnóstico y la etiología de esta rara complicación infecciosa diferida.
Anterior cervical discectomy and fusion (or disk arthroplasty) has a low complication rate, with a reported infection rate lower than 3%.1,2 Most surgical site infections (SSI) occur in the early postoperative period. Delayed SSI, defined as occurring after 3 months from surgery, is a very rare complication.3 We report a case of delayed prevertebral cervical abscess diagnosed 2 years after two-level cervical arthroplasty, discuss the diagnosis and etiology, and review the literature.
Case reportA 55 years-old male consulted for a right cervical mass that had been slowly growing for eight weeks. Past medical history included high blood pressure, hyperlipidemia, smoking and alcoholic hepatopathy. Two years before, the patient was treated of disk herniation in another center, with C4–C5–C6 discectomy and arthroplasty (M6-C, Spinal Kinetics, Sunnyvale, CA, USA), with an uneventful postoperative period.
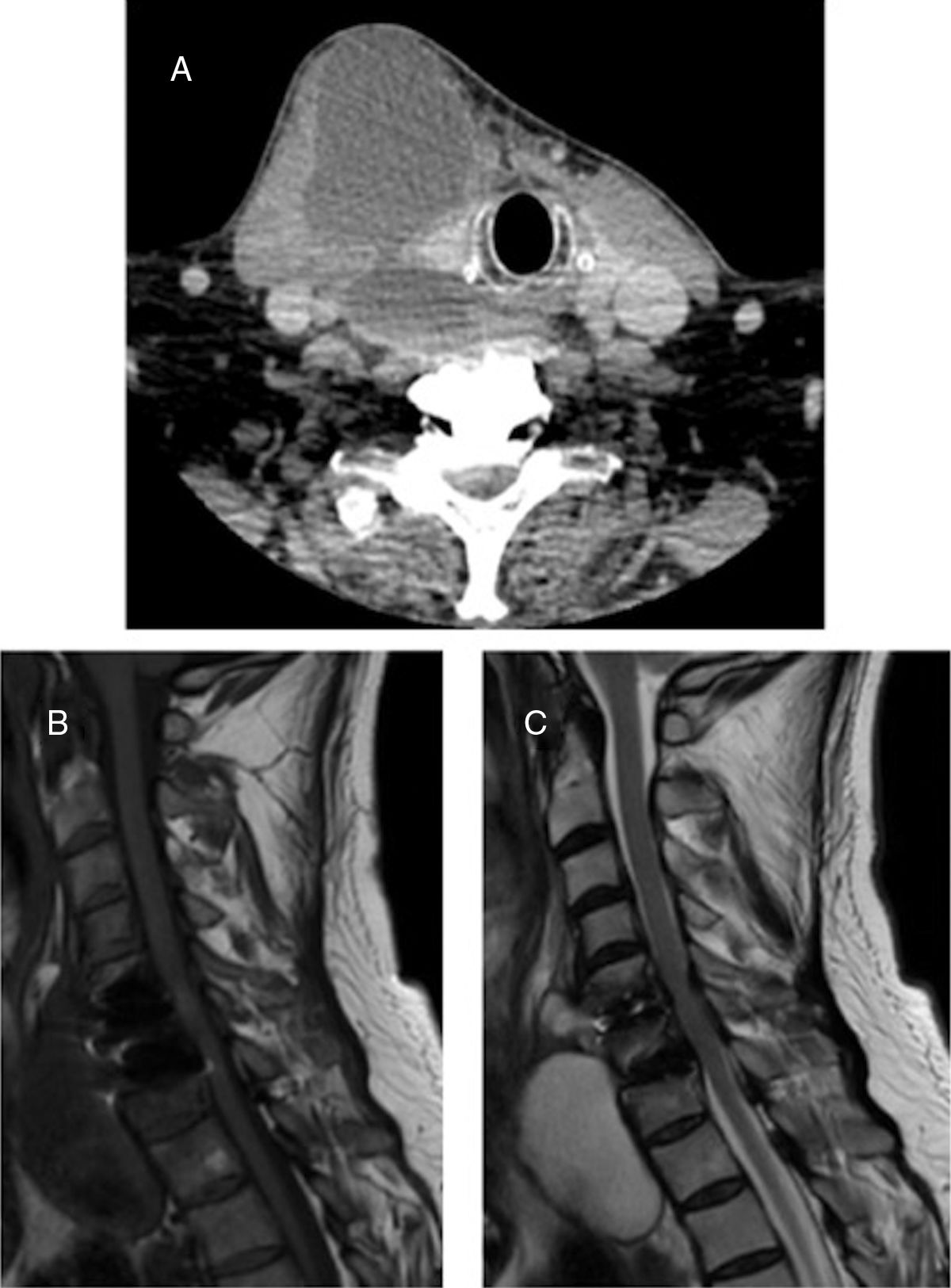
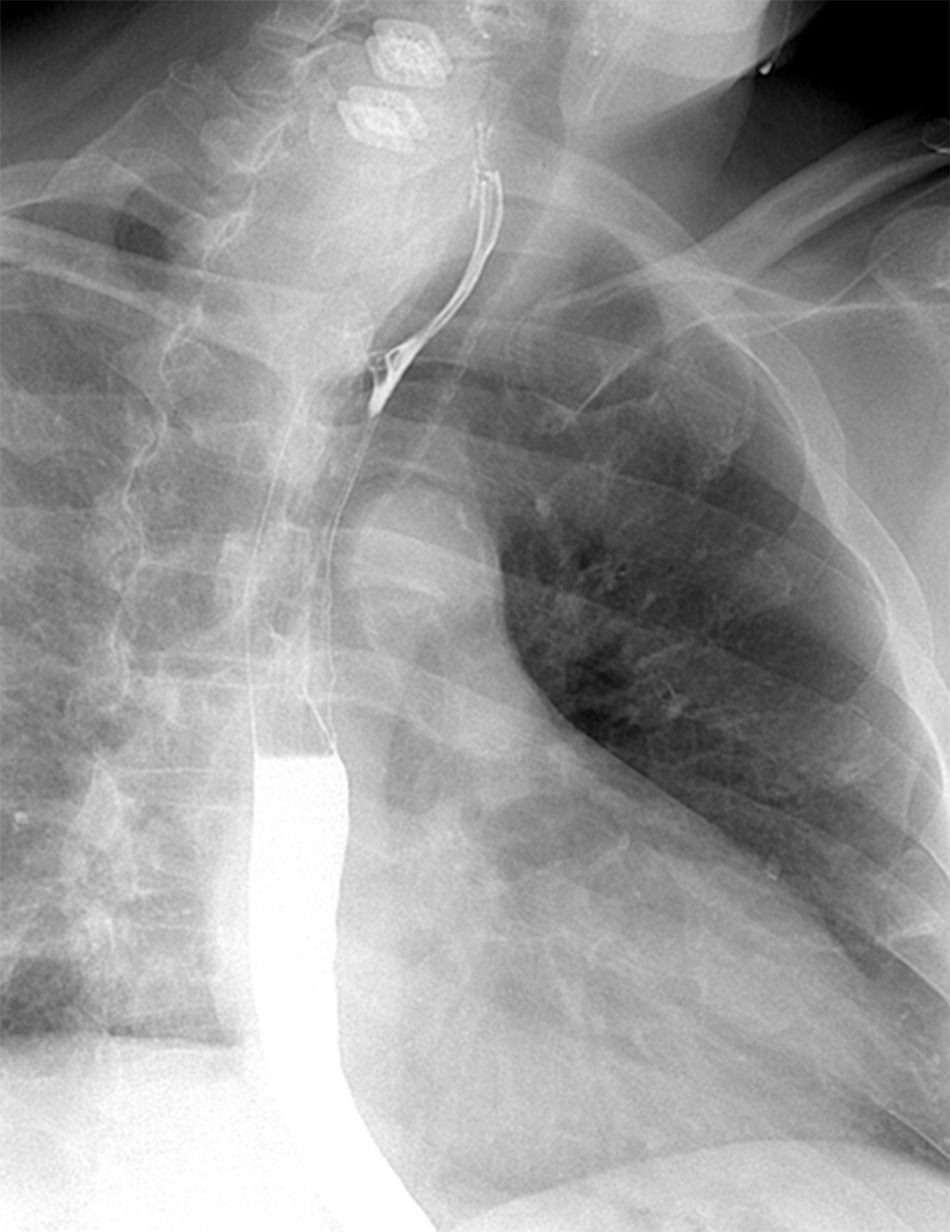
Physical examination revealed a fluctuant and tight right laterocervical mass, without fever, dysphagia, dyspnea or neurological deficits. Estimated sedimentation rate (ESR) was 20mm/h, C-reactive protein was (CRP) <1mg/dL and white blood cell (WBC) count was 6500/mm3 with 60% of neutrophils. Human immunodeficiency virus test was negative. Flexible laryngeal and esophageal endoscopy revealed an extrinsic laryngeal constriction but no intraluminal pathology. CT scan showed a right cervical prevertebral hypodens mass with mild peripheral iodine contrast enhancement at C4–D2 level (Fig. 1). MR revealed a T1WI hypointense and T2WI and STIR hyperintense mass (Fig. 1). The barium swallow did not show pass of contrast into the cavity (Fig. 2). Our primary diagnosis was delayed SSI because of the patient's risk factors. However, due to the slow growing of the collection, we could not exclude tuberculosis or post-surgical pseudomeningocele because of the lack of systemic inflammatory reaction and MR findings.
CT and MR. (A) Iodine contrast-enhanced CT scan, showing a right cervical prevertebral hypodense mass with mild peripheral contrast enhancement. (B) Sagittal cervical spine MR, showing a T1 hypointense mass. (C) Sagital cervical spine MR, showing a T2 hyperintense mass, suggestive of either cerebrospinal fluid collection or abscess.
Finally, owing to slow but continuous mass enlargement, an ultrasound guided puncture was performed, obtaining pus, but it did not provide enough evacuation neither microbiological diagnosis. Consequently, we indicated surgical exploration.
Intraoperatively, we found a capsulated cavity containing pus that extended to the prevertebral space in contact with the prostheses, without any associated tracheal or esophageal lesion. After abscess debridement, prostheses were removed and substituted for iliac crest bone graft (Fig. 3), and rifampicin was instilated.
We actively looked for a cerebrospinal fluid leak, aided by Valsalva maneuver, but we could not demonstrate it. In order to rule out a pseudomeningocele, we performed beta-2-transferrine test. It yielded a positive result but, as later discussed, we assumed it as a false positive. The bacterial culture and polymerase chain reaction analysis (PCR) were positive for Propionibacterium acnes, so antibiotic was adjusted from vancomycin and meropenem to amoxicillin-clavulanate 1g every 8h for 6 weeks. The postoperative period was uneventful. At 6 months follow-up, the patient remained asymptomatic.
DiscussionAnterior cervical discectomy is a common procedure with a low infection rate, being most of them during the early postoperative period.1,2 In our literature review we found 7 cases of delayed SSI, defined as infection occurring after 3 months from surgery.3
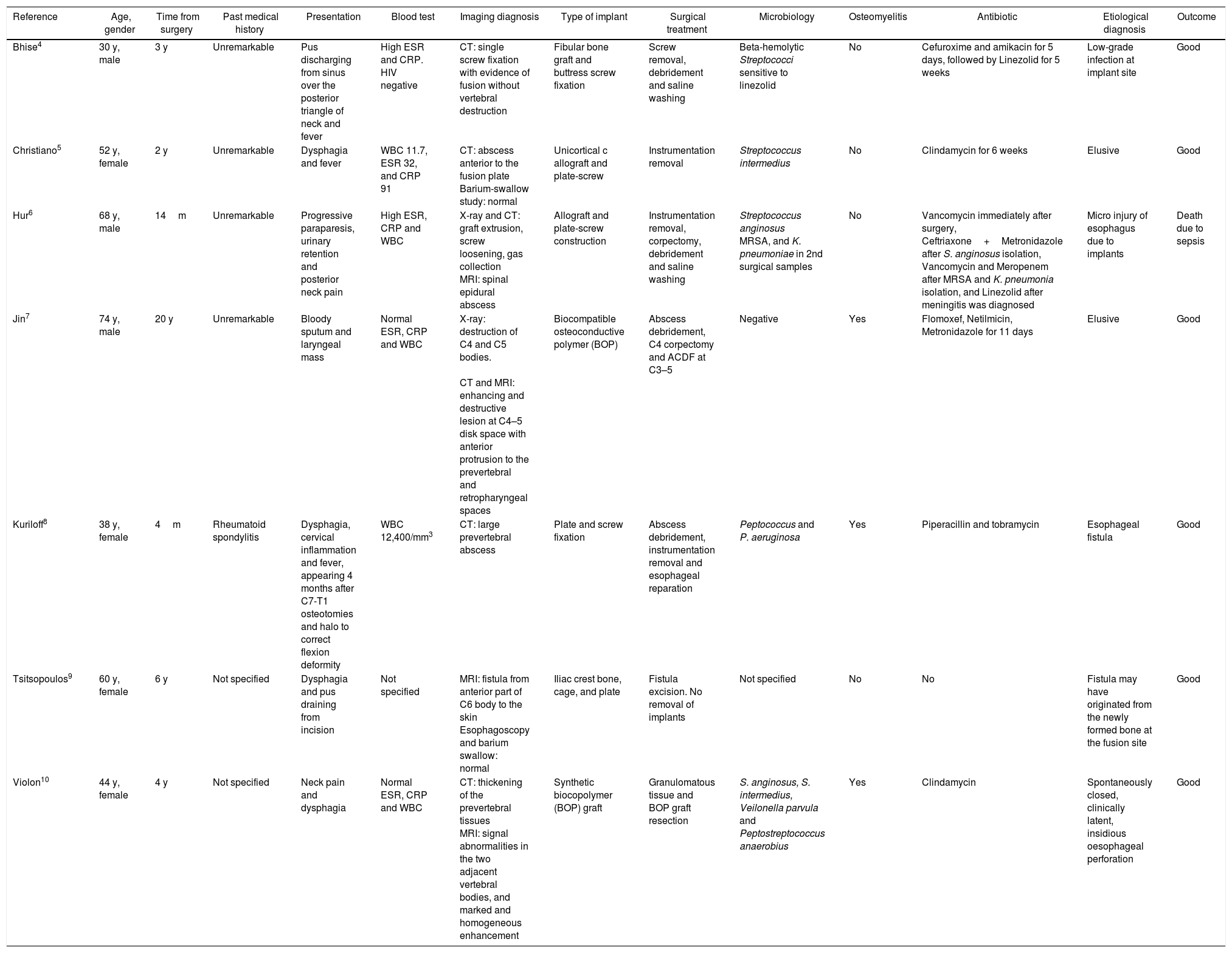
Bhise4 reported a patient with fever and pus-discharging sinus over the posterior triangle of the neck, without any cavitation around the fused segment, and suggested a low-grade infection at implant site as the probable etiology. Christiano5 reported a case that presented with dysphagia and fever secondary to a prevertebral abscess, and stated the cause of infection was elusive. Hur6 presented a case of neck pain and progressive spinal cord syndrome due to an epidural abscess and proposed micro injury of esophagus due to implants as a causal factor. Jin7 reported a patient who consulted for blood-tinged sputum and a laryngeal mass, CT and MR revealed a prevertebral abscess associated to osteomyelitis, and they reported the cause of infection as elusive. Kuriloff8 published a case of a patient who consulted for dysphagia, cervical inflammation and fever, whose CT revealed a prevertebral abscess, and that was secondary to an esophageal fistula. Tsitsopoulos9 presented a patient with dysphagia and pus draining from incision due to a fistula from prevertebral space, and suggested it may have originated from the newly formed bone at the fusion site. Violon10 reported a case of neck pain and dysphagia due to prevertebral abscess and stated an insidious esophageal wall perforation might be evoked as the possible source of the infection. All cases had a good outcome after surgical revision and antibiotherapy, except the patient reported by Hur,6 who died due to sepsis. See Table 1 for a detailed review of these reported cases.
Overview of 7 reported cases of anterior cervical spine delayed SSI.
| Reference | Age, gender | Time from surgery | Past medical history | Presentation | Blood test | Imaging diagnosis | Type of implant | Surgical treatment | Microbiology | Osteomyelitis | Antibiotic | Etiological diagnosis | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bhise4 | 30 y, male | 3 y | Unremarkable | Pus discharging from sinus over the posterior triangle of neck and fever | High ESR and CRP. HIV negative | CT: single screw fixation with evidence of fusion without vertebral destruction | Fibular bone graft and buttress screw fixation | Screw removal, debridement and saline washing | Beta-hemolytic Streptococci sensitive to linezolid | No | Cefuroxime and amikacin for 5 days, followed by Linezolid for 5 weeks | Low-grade infection at implant site | Good |
| Christiano5 | 52 y, female | 2 y | Unremarkable | Dysphagia and fever | WBC 11.7, ESR 32, and CRP 91 | CT: abscess anterior to the fusion plate Barium-swallow study: normal | Unicortical c allograft and plate-screw | Instrumentation removal | Streptococcus intermedius | No | Clindamycin for 6 weeks | Elusive | Good |
| Hur6 | 68 y, male | 14m | Unremarkable | Progressive paraparesis, urinary retention and posterior neck pain | High ESR, CRP and WBC | X-ray and CT: graft extrusion, screw loosening, gas collection MRI: spinal epidural abscess | Allograft and plate-screw construction | Instrumentation removal, corpectomy, debridement and saline washing | Streptococcus anginosus MRSA, and K. pneumoniae in 2nd surgical samples | No | Vancomycin immediately after surgery, Ceftriaxone+Metronidazole after S. anginosus isolation, Vancomycin and Meropenem after MRSA and K. pneumonia isolation, and Linezolid after meningitis was diagnosed | Micro injury of esophagus due to implants | Death due to sepsis |
| Jin7 | 74 y, male | 20 y | Unremarkable | Bloody sputum and laryngeal mass | Normal ESR, CRP and WBC | X-ray: destruction of C4 and C5 bodies. CT and MRI: enhancing and destructive lesion at C4–5 disk space with anterior protrusion to the prevertebral and retropharyngeal spaces | Biocompatible osteoconductive polymer (BOP) | Abscess debridement, C4 corpectomy and ACDF at C3–5 | Negative | Yes | Flomoxef, Netilmicin, Metronidazole for 11 days | Elusive | Good |
| Kuriloff8 | 38 y, female | 4m | Rheumatoid spondylitis | Dysphagia, cervical inflammation and fever, appearing 4 months after C7-T1 osteotomies and halo to correct flexion deformity | WBC 12,400/mm3 | CT: large prevertebral abscess | Plate and screw fixation | Abscess debridement, instrumentation removal and esophageal reparation | Peptococcus and P. aeruginosa | Yes | Piperacillin and tobramycin | Esophageal fistula | Good |
| Tsitsopoulos9 | 60 y, female | 6 y | Not specified | Dysphagia and pus draining from incision | Not specified | MRI: fistula from anterior part of C6 body to the skin Esophagoscopy and barium swallow: normal | Iliac crest bone, cage, and plate | Fistula excision. No removal of implants | Not specified | No | No | Fistula may have originated from the newly formed bone at the fusion site | Good |
| Violon10 | 44 y, female | 4 y | Not specified | Neck pain and dysphagia | Normal ESR, CRP and WBC | CT: thickening of the prevertebral tissues MRI: signal abnormalities in the two adjacent vertebral bodies, and marked and homogeneous enhancement | Synthetic biocopolymer (BOP) graft | Granulomatous tissue and BOP graft resection | S. anginosus, S. intermedius, Veilonella parvula and Peptostreptococcus anaerobius | Yes | Clindamycin | Spontaneously closed, clinically latent, insidious oesophageal perforation | Good |
In these reported cases, the predominant microbiological isolation was Streptococcus spp., associated to 1 case of Veilonella spp. and 2 of Peptostreptococcus spp., which are members of the salivary and gut microbiome.11
We could not find a common pattern between clinical manifestation, blood test results, type of implant and associated osteomyelitis in these patients with delayed SSI.
Different causes of delayed SSI are proposed among reported cases: low grade infection at implant site, microinjury of esophagus, definite esophageal fistula, fistulation to skin from the newly formed bone at fusion site, but infection was also reported as elusive in 2 cases.
Regarding treatment options, in all cases except in Tsitsopoulos’,9 surgical debridement and removal of implants was performed, followed by antibiotic adjusted by microorganism culture.
To our knowledge, this is the only report of a delayed cervical spine SSI manifesting as a slowly growing cervical mass as the only clinical manifestation without any associated inflammatory findings.
The microbiological isolation of P. acnes, confirmed by PCR assay, implies some discussion. First, it is a member of skin and gut floras,11 which could favor the hypotheses of either latent implant contamination or acquired and spontaneously healed esophageal microperforation. Second, it is known as a microfilm creator,12 which could support the latent implant contamination hypothesis, and favors surgical removal of implants. Third, the patient underwent arthroplasty instead of fusion, which raises the question if the different implant properties could be a risk factor for a delayed implant-related SSI by biofilm-producing bacteria. Finally, it has a slow growth,12 which would justify this unusual course for a cervical abscess.
The beta-2-transferrin test is an elementary tool in the diagnosis of cerebrospinal fluid leak.13 MR findings raised the possibility of a spontaneously closed and subsequently infected pseudomeningocele. Therefore, we performed beta-2-transferrin test in the sample of purulent material. We obtained a positive result, which lead to strict control of meningeal irritation signs or cerebrospinal fluid fistula. Nevertheless, the lack of meningeal symptomatology, the non-confirming imaging tests, the intraoperative findings and the neuraminidase secretion of most of P. acnes strains,14 a known cause of false-positive test due to transferrine enzymatic processing,13 lead us to assume it as a false positive.
Acquired esophageal/tracheal microperforation, latent clinically-silent implant infection and bacteremia15 have been described as possible causes of delayed SSI in the cervical spine. In this case, micro-trauma related and spontaneously healed esophageal micro-perforation could not be completely ruled out. Nonetheless, due to P. acnes slow growth and microfilm formation,12 a latent implant infection was the infection cause we assumed.
ConclusionWe report an illustrative case of a delayed cervical paravertebral abscess following uneventful cervical disk arthroplasty. Our patient presented with a slowly growing paravertebral abscess appearing 2 years after cervical surgery without any inflammatory parameters. Delayed SSI is a rare but potentially severe complication after anterior cervical discectomy. Revision surgery is almost always required followed by long-course antibiotic treatment.
Conflicts of interest and source of fundingThe manuscript submitted does not contain information about medical device(s)/drug(s). No funds were received in support of this work. No benefits in any form have been or will be received related directly or indirectly to the subject of this manuscript.
The present research has not received any specific scholarship from public, commercial, or non-profit agencies.
We would like to thank Carmen Cabellos, MD, PhD, not only for her help with the conception of this work, but also for her everyday dedication.