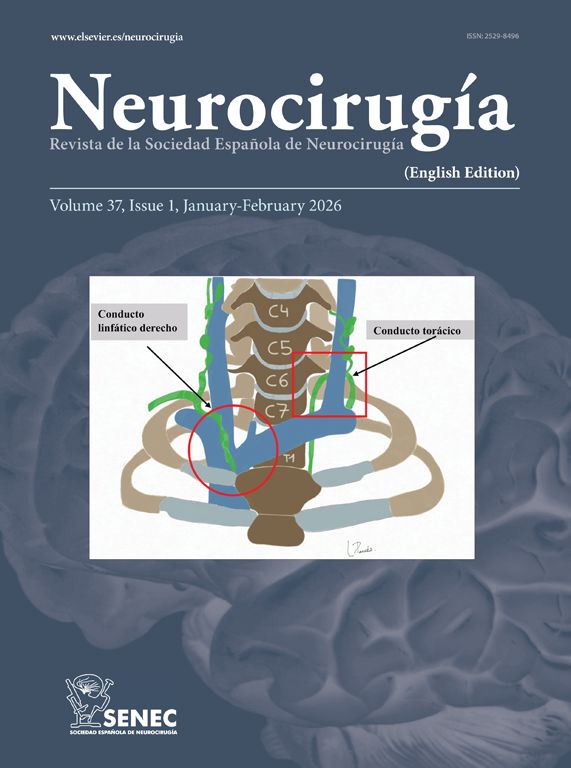
Throughout neurosurgical history, the treatment of intrinsic lesions located in the brainstem has been subject of much controversy. The brainstem is the anatomical structure of the central nervous system (CNS) that presents the highest concentration of nuclei and fibers, and its simple manipulation can lead to significant morbidity and mortality. Once one of the safe entry points at the medulla oblongata has been established, we wanted to evaluate the safest approach to the olivary body (the most used safe entry zone on the anterolateral surface of the medulla oblongata). The proposed objective was to evaluate the working channel from the surface of each of the far lateral and retrosigmoid approaches to the olivary body: distances, angles of attack and channel content.
Material and methodsTo complete this work, a total of 10 heads injected with red/blue silicone were used. A total of 40 approaches were made in the 10 heads used (20 retrosigmoid and 20 far lateral). After completing the anatomical study and obtaining the data referring to all the approaches performed, it was decided to expand the sample of this research study by using 30 high-definition magnetic resonance imaging of anonymous patients without cranial or cerebral pathology. The reference points used were the same ones defined in the anatomical study. After defining the working channels in each of the approaches, the working distances, angle of attack, exposed surface, and the number of neurovascular structures present in the central trajectory were analyzed.
ResultsThe distances to the cranial and medial region of the olivary body were 52.71 mm (SD 3.59) from the retrosigmoid approach and 27.94 mm (SD 3.99) from the far lateral; to the most basal region of the olivary body, the distances were 49.93 (SD 3.72) from the retrosigmoid approach and 18.1 mm (SD 2.5) from the far lateral. The angle of attack to the caudal region was 19.44° (SD 1.3) for the retrosigmoid approach and 50.97° (SD 8.01) for the far lateral approach; the angle of attack to the cranial region was 20.3° (SD 1.22) for the retrosigmoid and 39.9° (SD 5.12) for the far lateral. Regarding neurovascular structures, the probability of finding an arterial structure is higher for the lateral far, whereas a neural structure will be more likely from a retrosigmoid approach.
ConclusionsAs conclusions of this work, we can say that far lateral approach presents more favorable conditions for the microsurgical treatment of intrinsic bulbar and bulbomedullary lesions approached through the caudal half of the olivary body. In those cases of bulbar and pontine-bulbar lesions approached through the cranial half of the olivary body, the retrosigmoid approach can be considered for selected cases.
A lo largo de la historia neuroquirúrgica, el tratamiento de lesiones intrínsecas localizadas en el tronco cerebral ha sido tema de mucha controversia. El tronco cerebral es la estructura anatómica del sistema nervioso central (SNC) que presenta mayor concentración de núcleos y fibras, y su simple manipulación puede conllevar importante morbi-mortalidad. Una vez establecido uno de los puntos de entrada seguros a nivel bulbar, hemos querido evaluar el abordaje más seguro a la oliva bulbar (la principal zona de entrada segura a la región anterolateral del bulbo raquídeo). El objetivo planteado fue evaluar el canal de trabajo desde la superficie de cada uno de los abordajes far lateral y retrosigmoideo hasta la oliva bulbar: distancias, ángulos de ataque y contenido del canal.
Materiales y métodosPara completar el presente trabajo se utilizaron un total de 10 cabezas inyectadas con silicona rojo/azul. Se realizaron un total de 40 abordajes en las 10 cabezas utilizadas (20 retrosigmoideos y 20 far lateral). Tras completar el estudio anatómico y obtener los datos referentes a todos los abordajes realizados, se decidió ampliar la muestra del presente estudio de investigación mediante el uso de 30 resonancias magnéticas de alta definición de pacientes anónimos sin patología craneal ni cerebral. Los puntos referenciales utilizados fueron los mismos definidos en los estudios anatómicos. Tras definir los canales de trabajo en cada uno de los abordajes se analizaron las distancias de trabajo, ángulo de ataque, superficie de exposición y el número de estructuras neurovasculares presentes en el trayecto central.
ResultadosLas distancias para la región craneal y medial de la oliva bulbar fueron de 52,71 mm (DT 3,59) para el abordaje retrosigmoideo y de 27,94 mm (DT 3,99) para elfar lateral; para la región más basal de la oliva bulbar las distancias fueron de 49,93 (DT 3,72) para el abordaje retrosigmoideo y de 18,1 mm (DT 2,5) para el far lateral. El ángulo de ataque para la región caudal fue de 19,44° (DT 1,3) para el abordaje retrosigmoideo y de 50,97° (DT 8,01) para el abordaje far lateral; el ángulo de ataque para la región craneal fue de 20,3° (DT 1,22) para el retrosigmoideo y de 39,9° (DT 5,12) para el far lateral. En cuanto a las estructuras neurovasculares la probabilidad de encontrar una estructura arterial es más alta para el far lateral, en cambio una estructura neural será más probable desde un retrosigmoideo.
ConclusionesComo conclusiones de este trabajo podemos decir que el abordaje far lateral presenta condiciones más favorables para el tratamiento microquirúrgico de lesiones intrínsecas bulbares y bulbomedulares abordadas a través de la mitad caudal de la oliva bulbar. En aquellos casos de lesiones bulbares y bulboprotuberanciales abordadas a través de la mitad craneal de la oliva bulbar, el abordaje retrosigmoideo puede ser considerado para casos seleccionados.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.