Ankylosing spondylitis is an inflammatory rheumatic disease mainly affecting the axial skeleton. The rigid spine may secondarily develop osteoporosis, further increasing the risk of spinal fracture. In this study, we reviewed fractures in patients with ankylosing spondylitis that had been clinically diagnosed to better define the mechanism of injury, associated neurological deficit, predisposing factors, and management strategies.
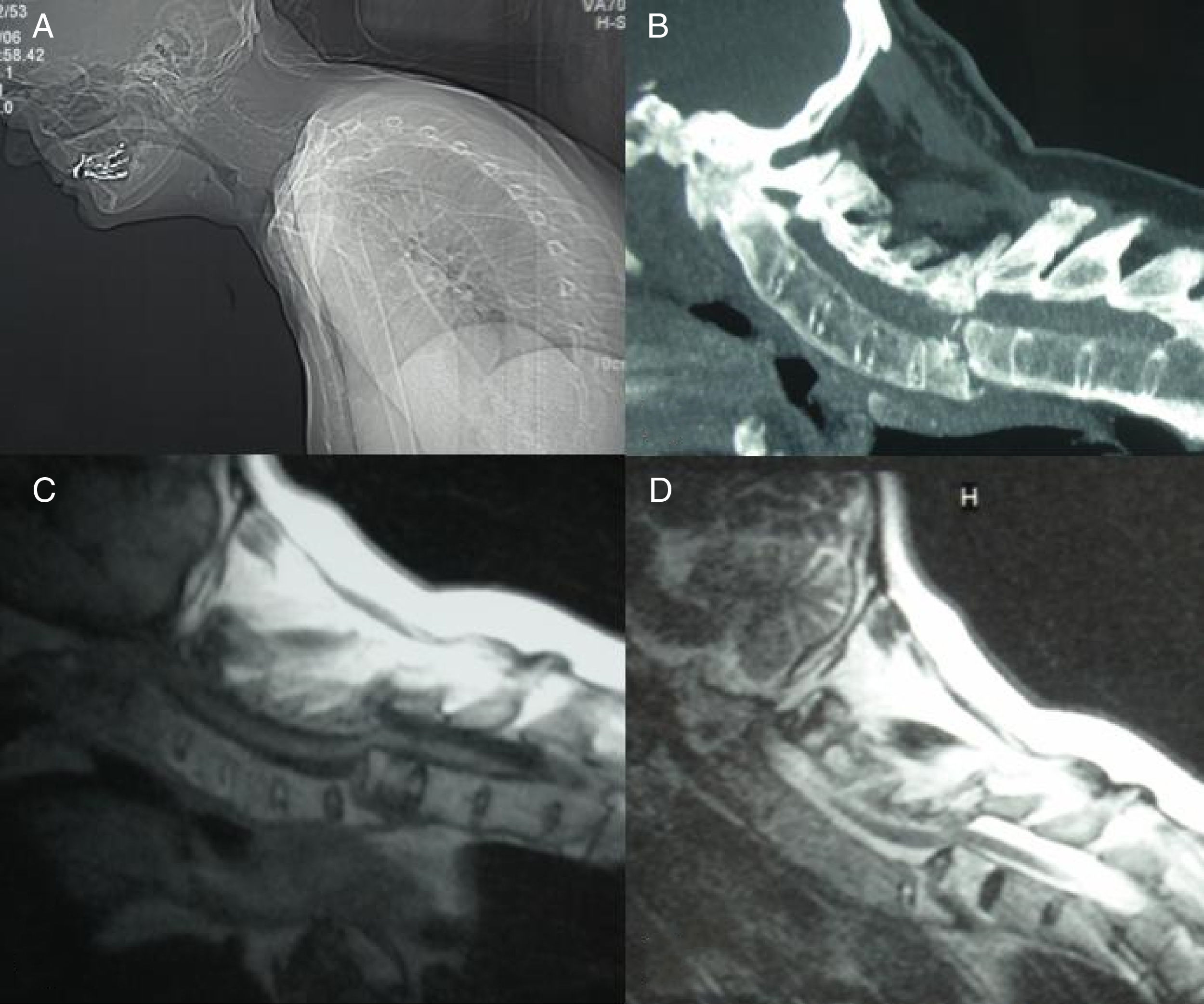
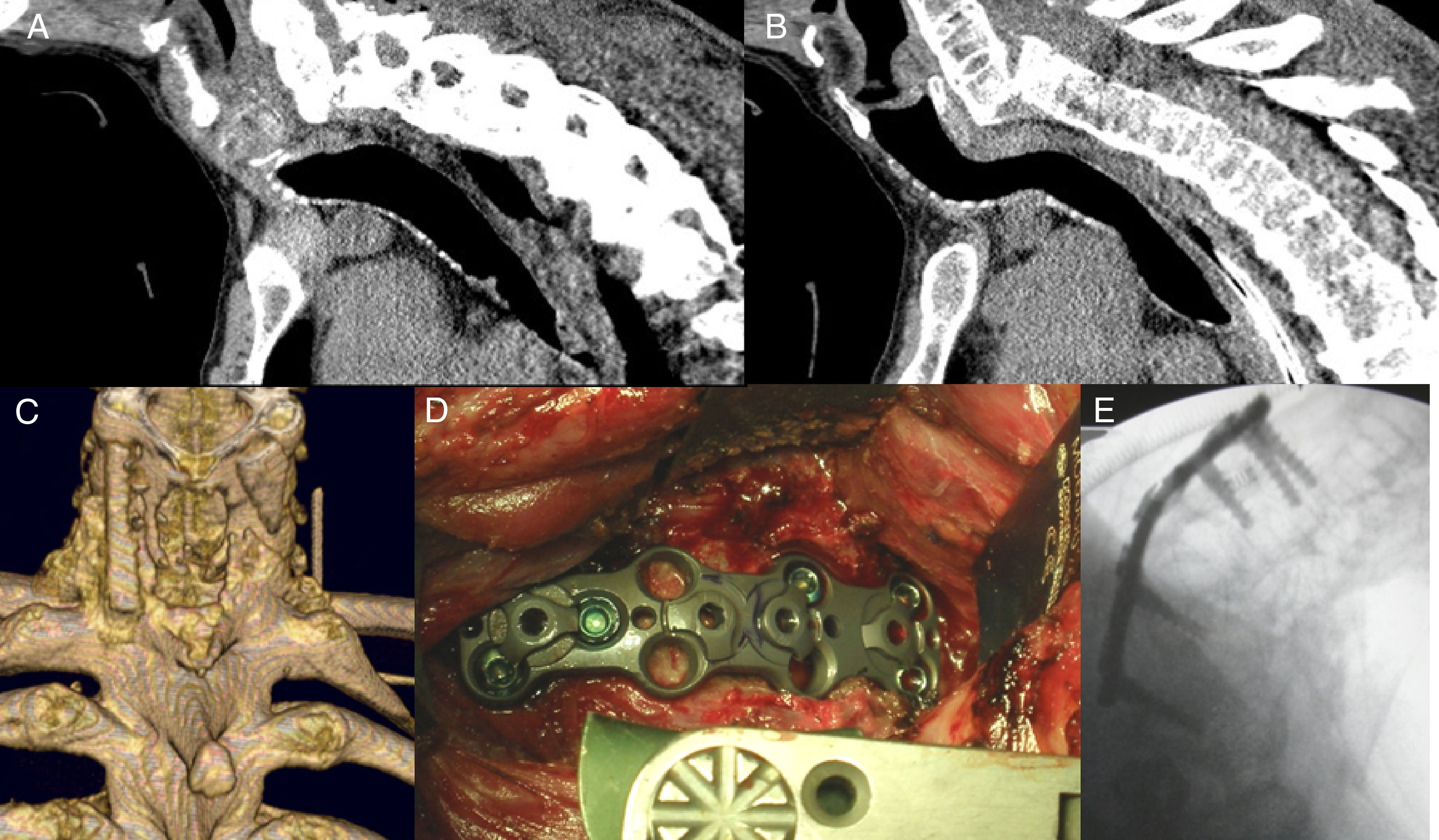
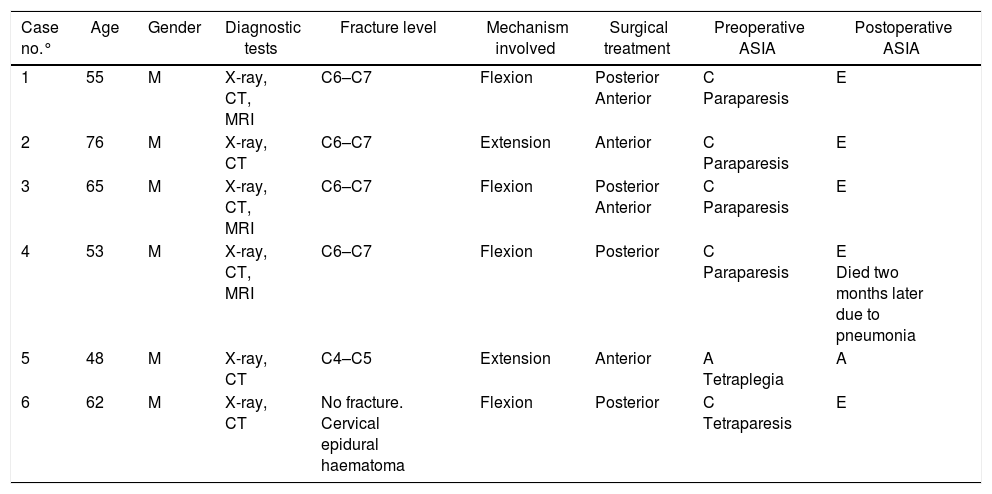
MethodsBetween January 2004 and December 2014, 6 patients with ankylosing spondylitis and neurological complications after injuries were treated. Neuroimaging evaluation was obtained in all patients by using plain radiography, CT scan, and MR imaging. The ASIA Impairment Scale was used in order to evaluate the neurologic status of the patients. Surgical decision was based on relationship of neurological involvement and spinal instability.
ResultsA total of 6 cervical injuries were identified in a review of patients in whom ankylosing spondylitis had been diagnosed. Of these, 2 patients were associated with a hyperextension mechanism and 4 cases by flexion mechanism. Posttraumatic neurological deficits were demonstrated in all 6 cases and neurological improvement after surgery was observed in 4 of these cases. The two cases were not improved by the surgery was on a case by presenting a degree of Asia A and another patient who initially improved with surgery but died of pneumonia in the postoperative.
ConclusionsPatients with ankylosing spondylitis are highly susceptible to spinal fracture and spinal cord injury even after only mild trauma. Initial CT or MR imaging of the whole spine is recommended even if the patient's symptoms are mild. The patient should also have early surgical stabilisation to correct spinal deformity and avoid worsening of the patient's neurological status.
La espondilitis anquilosante es una enfermedad reumática inflamatoria que afecta principalmente al esqueleto axial. La columna vertebral rígida puede secundariamente desarrollar osteoporosis, lo que aumenta aún más el riesgo de fractura vertebral. En este estudio, hemos revisado las fracturas en pacientes con espondilitis anquilosante que habían sido diagnosticados clínicamente para definir mejor el mecanismo de la lesión, déficit neurológico asociado y las estrategias de tratamiento.
MétodosEntre enero del 2004 y diciembre del 2014, 6 pacientes fueron revisados con espondilitis anquilosante y con complicaciones neurológicas después de caídas. El estudio de neuroimagen se obtuvo en todos los pacientes mediante el uso de la radiografía simple, TC y RM. La discapacidad se valoró según la escala de ASIA, se utilizó con el fin de evaluar el estado neurológico de los pacientes. La decisión quirúrgica se basó en relación con la afectación neurológica y la inestabilidad espinal.
ResultadosSe identificaron un total de 6 lesiones cervicales en pacientes con espondilitis anquilosante: 2 presentaron fracturas por mecanismos de extensión y 4 por mecanismos de flexión. Todos los casos fueron intervenidos quirúrgicamente. Los 6 pacientes presentaron déficit neurológico postraumático y en 4 de ellos se observó mejoría neurológica tras la cirugía. Dos casos no mejoraron tras la cirugía. Uno de ellos presentó un grado de ASIA A y el otro paciente, que mejoró inicialmente con la cirugía, falleció por neumonía en el postoperatorio dos meses después.
ConclusionesLos pacientes con espondilitis anquilosante son altamente susceptibles a la fractura vertebral y lesiones de la médula espinal, incluso después de traumatismos leves. Se recomienda la TC inicial o la RM de toda la columna vertebral, incluso si los síntomas del paciente son leves. El paciente también debe tener la estabilización quirúrgica temprana para corregir la deformidad espinal y evitar el empeoramiento del estado neurológico del paciente.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.