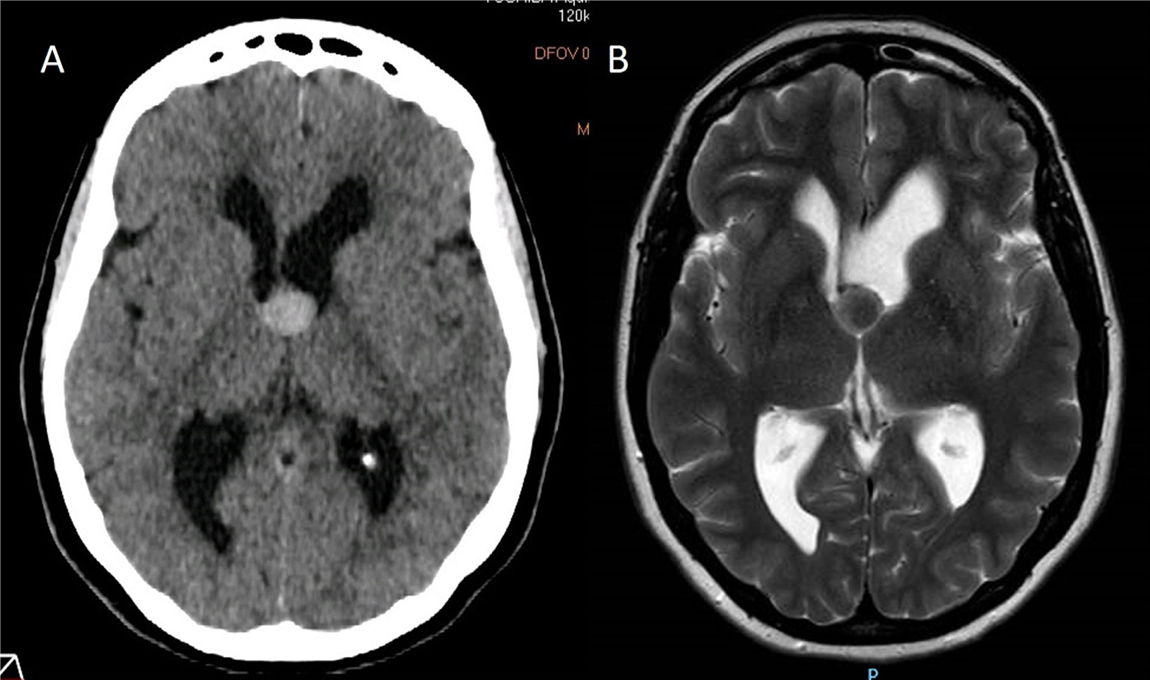
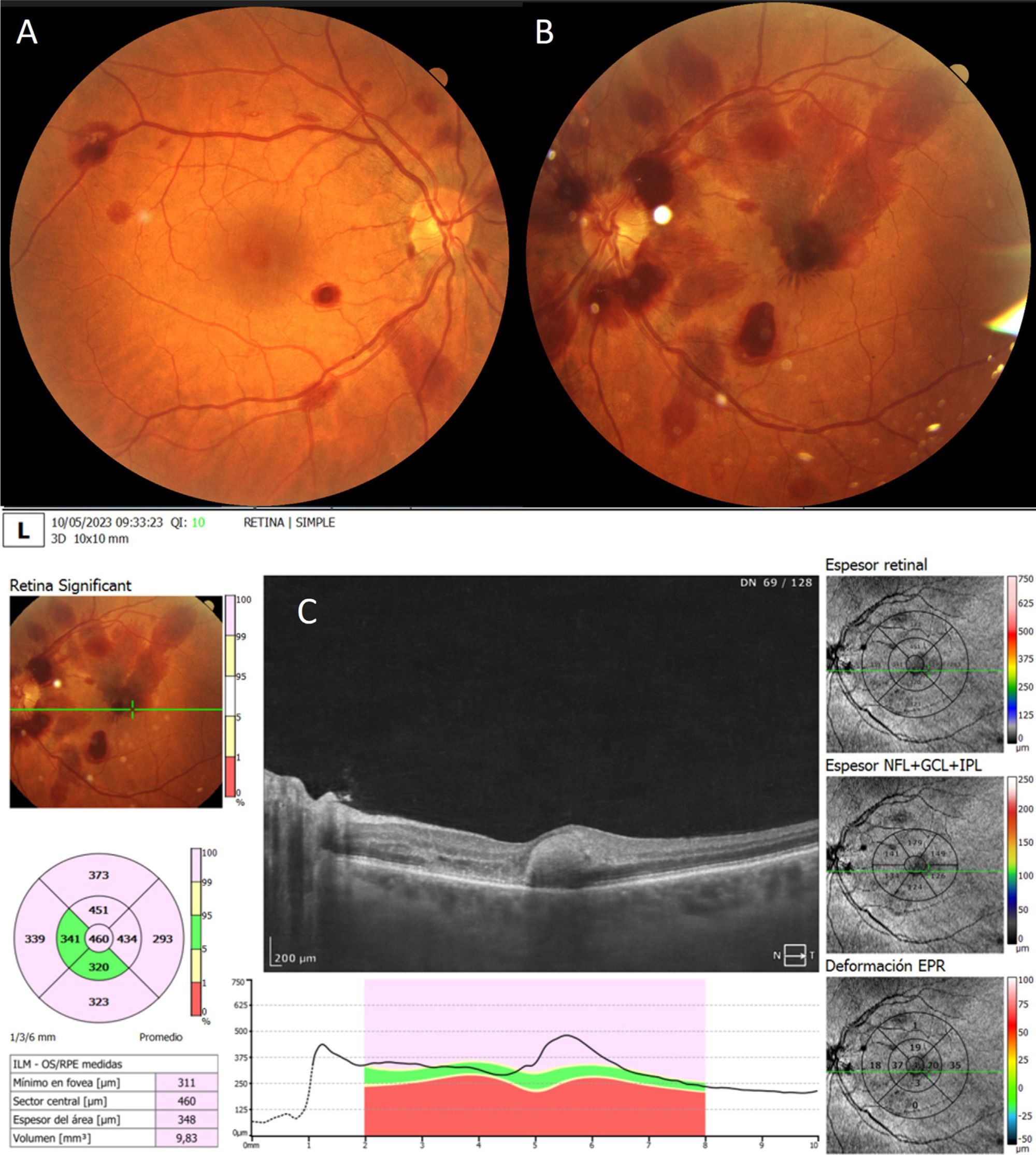
An extremely rare complication of endoscopic colloid cyst removal is presented. Terson’s syndrome related to endoscopic resection of a colloid cyst has been reported only twice before in the literature and it could be explained by intracranial hypertension related to rinsing during the procedure. The case is described and the complications in the neuroendoscopic removal of colloid cyst are reviewed from the literature.
Se presenta el caso de una rara complicación del tratamiento endoscópico e un quiste coloide. El síndrome de Terson en relación a la resección endoscópica de un quiste coloide ha sido publicada en solo dos ocasiones y podría estar relacionado con el aumento de presión intracraneal durante el procedimiento. Se describe el caso, así como las complicaciones potenciales del tratamiento endoscópico de los quistes coloides publicadas en la literatura.
Artículo

Si es la primera vez que accede a la web puede obtener sus claves de acceso poniéndose en contacto con Elsevier España en suscripciones@elsevier.com o a través de su teléfono de Atención al Cliente 902 88 87 40 si llama desde territorio español o del +34 932 418 800 (de 9 a 18h., GMT + 1) si lo hace desde el extranjero.
Si ya tiene sus datos de acceso, clique aquí.
Si olvidó su clave de acceso puede recuperarla clicando aquí y seleccionando la opción "He olvidado mi contraseña".