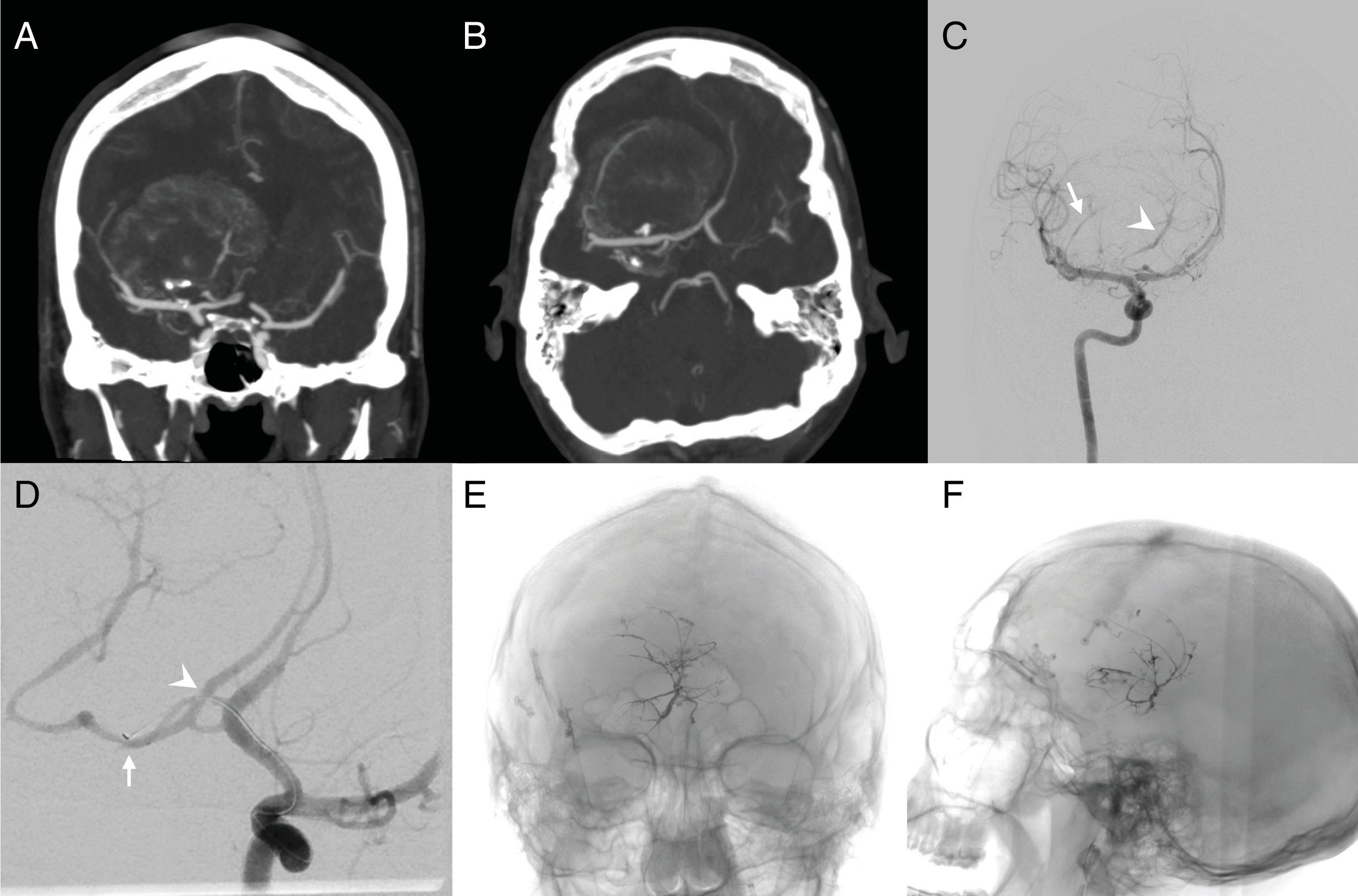
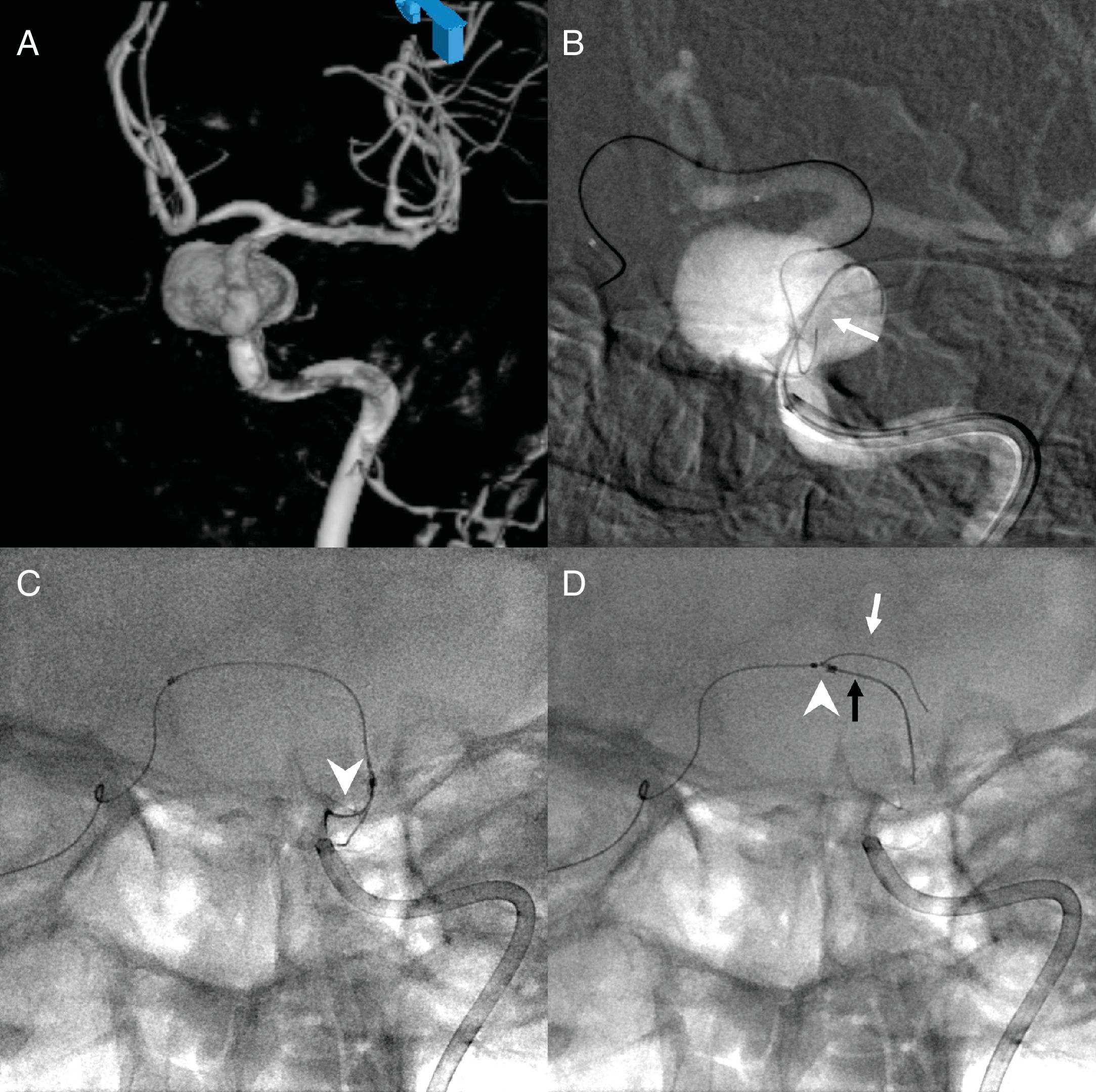
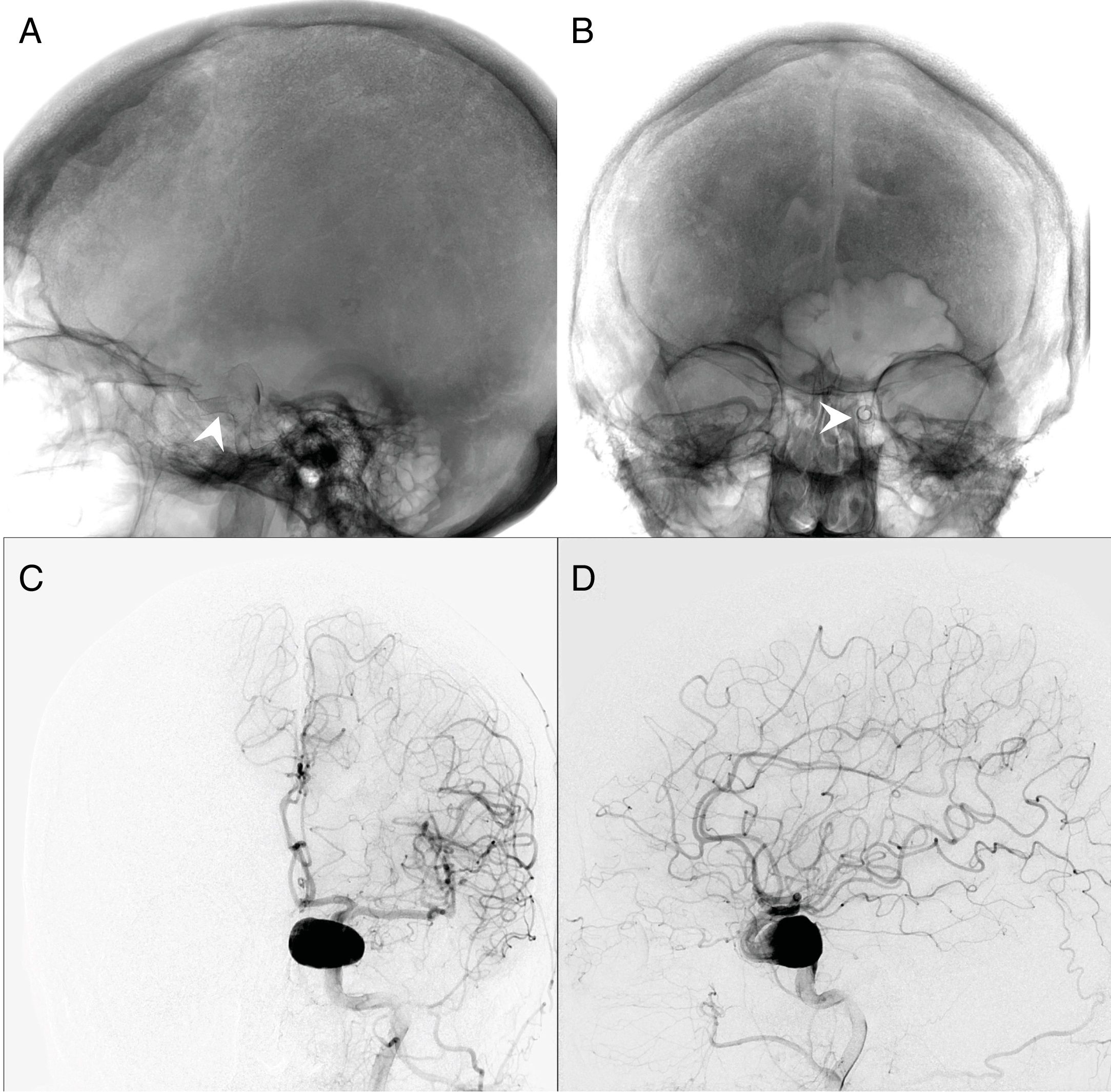
The breadth and complexity of neurovascular pathologies treated with endovascular neurosurgery has expanded dramatically in recent years. Many aneurysms remain difficult to treat safely. Transcirculation (contralateral and/or retrograde) approaches through the circle of Willis are useful alternatives for treating challenging lesions endovascularly. Here, we present a series of patients treated with unconventional transcirculation techniques.
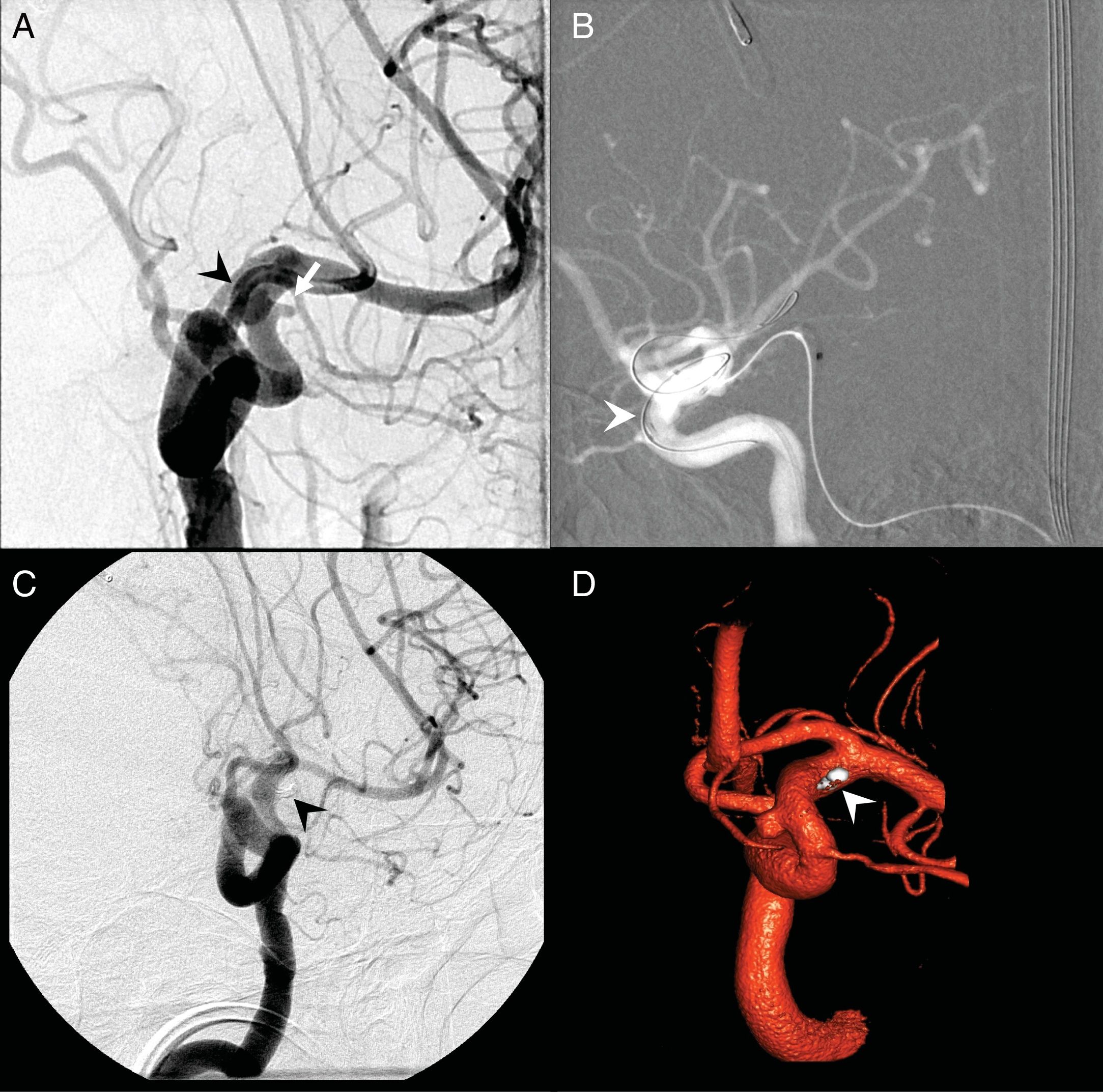
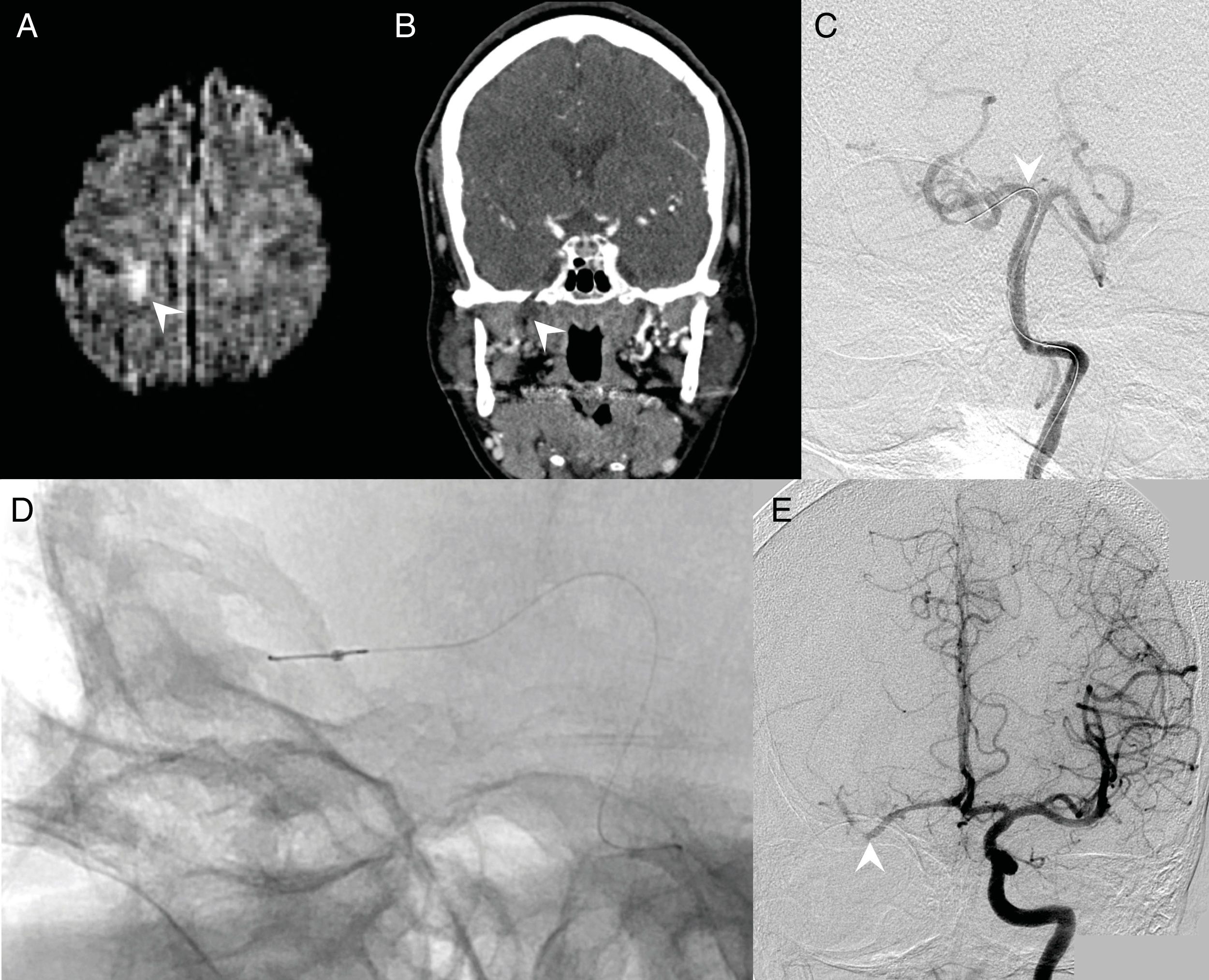
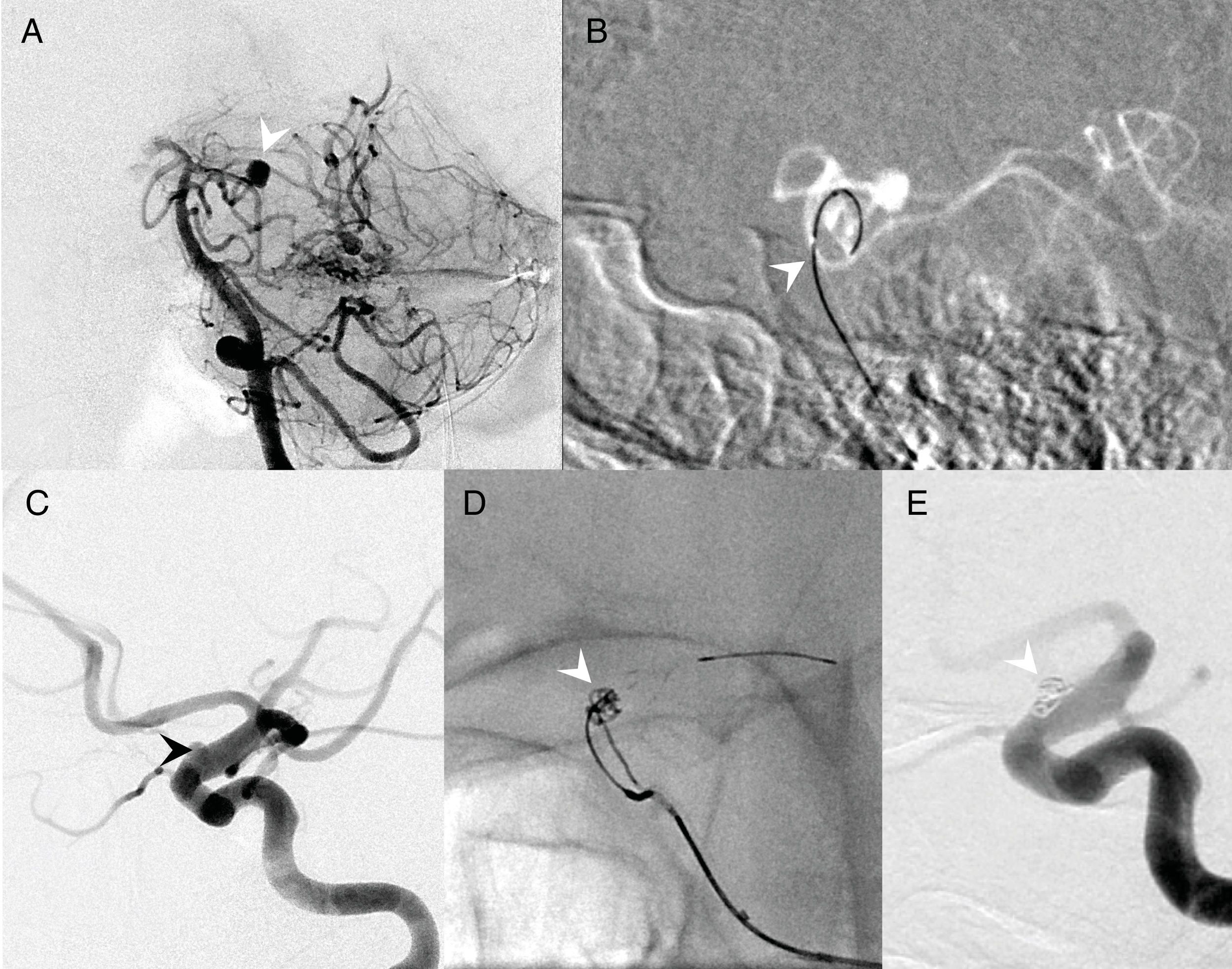
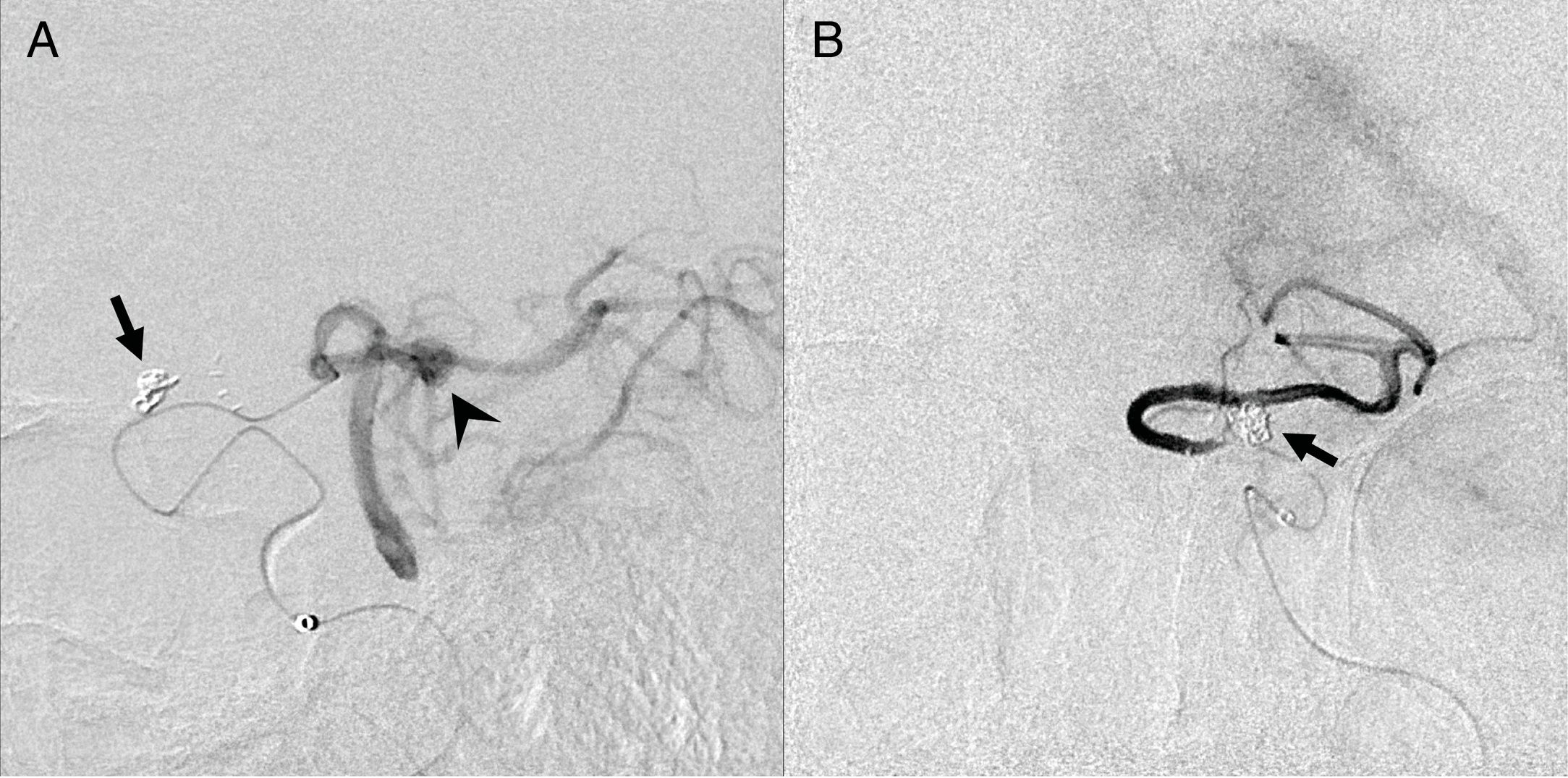
MethodsA total of six patients were treated: four patients with five aneurysms, one patient with an MCA stroke, and one patient with a meningioma requiring preoperative embolization were initially thought not to be amenable to endovascular treatment. The decision was made to treat these patients with transcirculation approaches. All patients were treated by one interventionist. One aneurysm was located in the cavernous internal carotid artery (ICA), one in the vertebral artery, two in the paraclinoid ICA, and one in a cerebellar AVM feeder vessel were treated.
ResultsFive of six patients (83%) made a full neurologic recovery. Three aneurysms were treated to complete occlusion, one aneurysm was left with small residual neck filling, and one aneurysm was not able to be treated. One patient underwent mechanical thrombectomy of a middle cerebral artery (MCA) embolus and MCA filling was restored after treatment. One patient underwent complete embolization of the deep vascular supply of a meningioma.
ConclusionsAlthough many neurovascular pathologies remain unsuitable for endovascular treatment, transcirculation approaches can allow for safe, successful treatment of challenging lesions in select patients.
La variedad y la complejidad de las enfermedades neurovasculares tratadas con neurocirugía endovascular ha aumentado drásticamente en los últimos años. Muchos aneurismas continúan siendo difíciles de tratar de forma segura. Los enfoques de transcirculación (contralateral y/o retrógrada) a través del círculo de Willis son alternativas útiles para el tratamiento endovascular de lesiones difíciles. Presentamos una serie de casos de pacientes tratados con técnicas de transcirculación no convencionales.
MétodosSe trató a un total de 6 pacientes que inicialmente se creía que no eran aptos para el tratamiento endovascular: 4 pacientes con 5 aneurismas, un paciente con un ictus de la arteria cerebral media (ACM) y un paciente con un meningioma que requería embolización preoperatoria. Se tomó la decisión de tratar a estos pacientes con métodos de transcirculación. Todos los pacientes fueron tratados por un solo especialista. Se localizaron y trataron un aneurisma en el segmento cavernoso de la arteria carótida interna (ACI), otro en la arteria vertebral, 2 en el segmento paraclinoideo de la ACI y otro en una malformación arteriovenosa cerebelosa de un vaso nutriente.
ResultadosCinco de los 6 pacientes (83%) alcanzaron una recuperación neurológica completa. Se trataron 3 aneurismas hasta una oclusión completa, un aneurisma se dejó con un pequeño relleno de cuello residual y otro aneurisma no pudo ser tratado. Un paciente fue sometido a una trombectomía mecánica de un émbolo en la ACM y el relleno de la ACM se restauró después del tratamiento. Un paciente se sometió a embolización completa del riego vascular profundo de un meningioma.
ConclusionesAunque muchas enfermedades neurovasculares siguen sin ser adecuadas para el tratamiento endovascular, los enfoques de transcirculación pueden permitir el tratamiento seguro y exitoso de lesiones difíciles en pacientes seleccionados.
Artículo

Si es la primera vez que accede a la web puede obtener sus claves de acceso poniéndose en contacto con Elsevier España en suscripciones@elsevier.com o a través de su teléfono de Atención al Cliente 902 88 87 40 si llama desde territorio español o del +34 932 418 800 (de 9 a 18h., GMT + 1) si lo hace desde el extranjero.
Si ya tiene sus datos de acceso, clique aquí.
Si olvidó su clave de acceso puede recuperarla clicando aquí y seleccionando la opción "He olvidado mi contraseña".