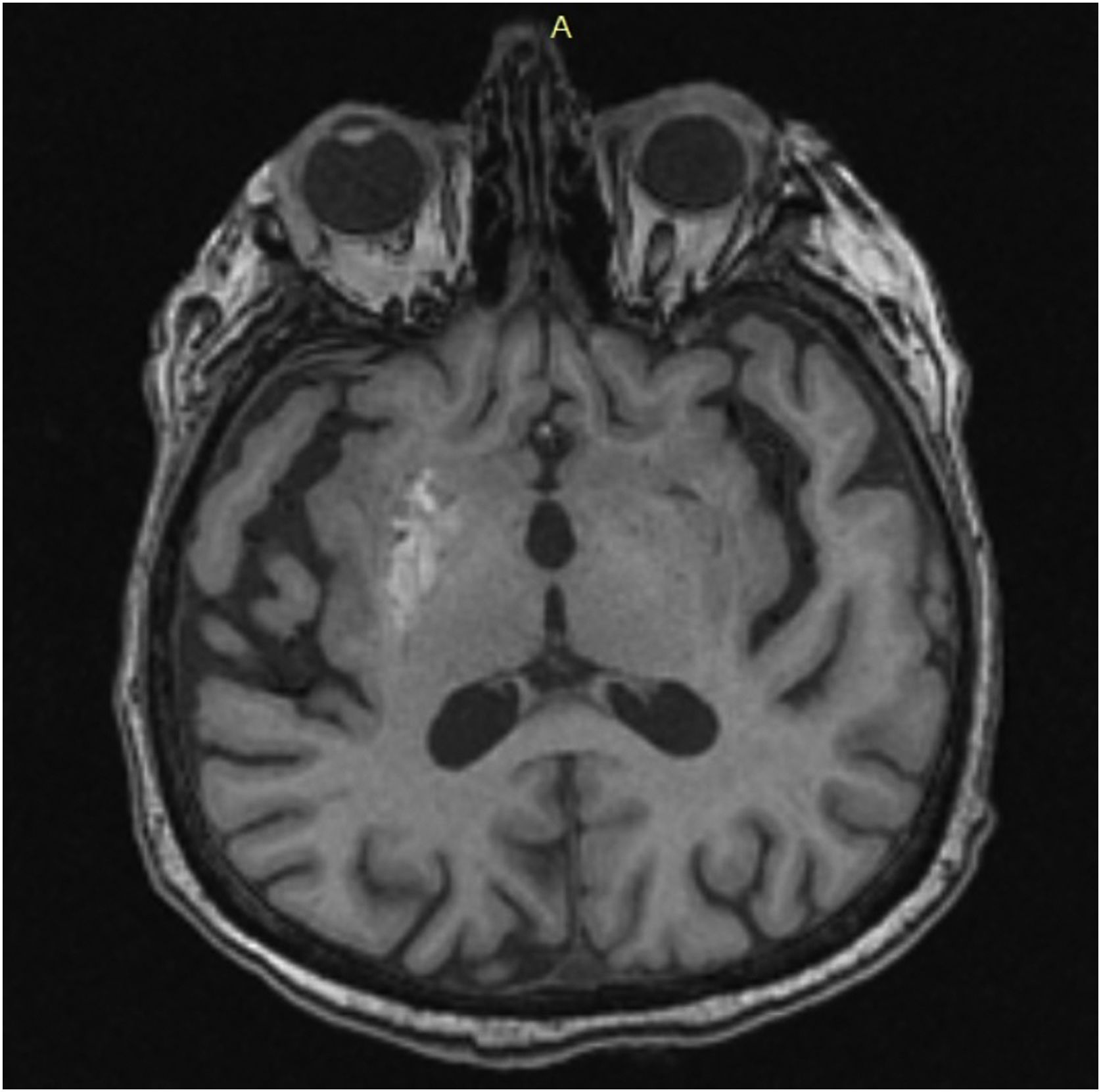
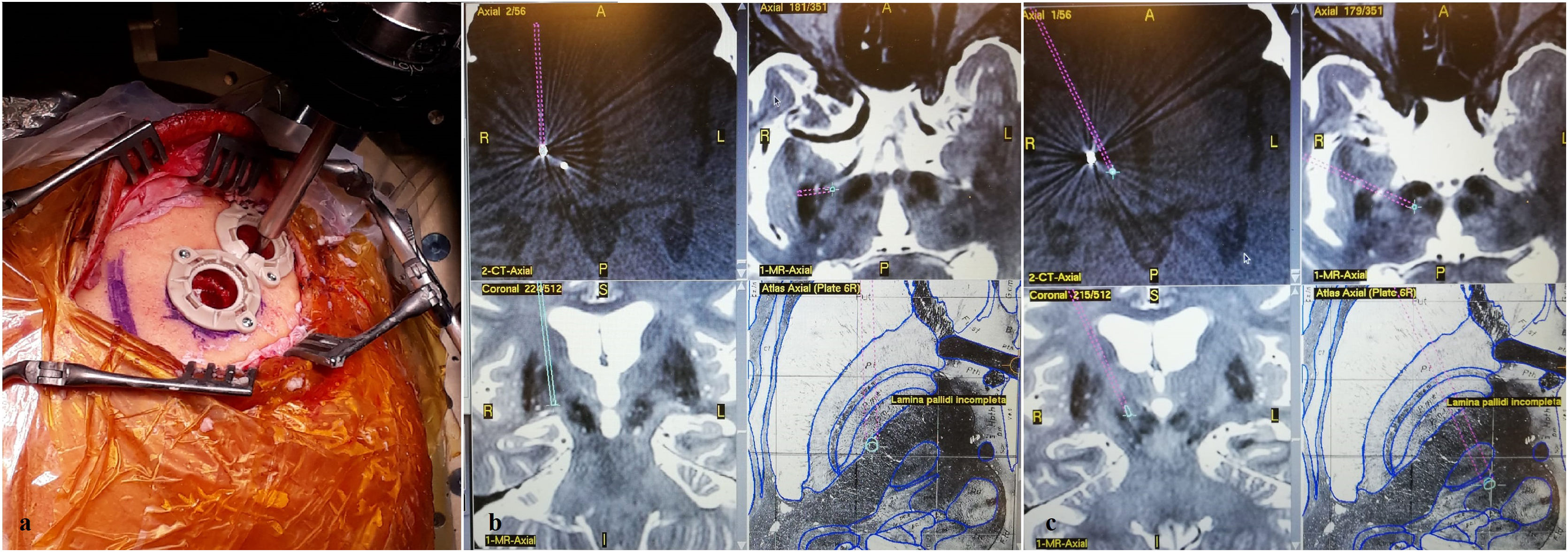
Hemiballism/hemichorea (HH) is a hyperkinetic movement disorder observed mostly in older adults with cerebrovascular diseases. Although the symptoms improve without any treatment, lesioning or DBS (deep brain stimulation) may be rarely required to provide symptomatic relief for patients with severe involuntary movements. HH is a rare complication of uncontrolled diabetes. There are only a few reported cases of diabetic HH that have been surgically treated. Thus, herein, we have reported the case of a 75-year-old female with type-II diabetes mellitus that presented with disabling involuntary limb movements of the left side, despite being treated conservatively for six months. DBS targeting the globus pallidus internus (GPi) and ventral intermediate (Vim) thalamic nucleus was performed. Complete resolution of symptoms was achieved with a combined stimulation of the thalamic Vim nucleus (at 1.7 mA) and GPi (at 2.4 mA). The combined stimulation of the Vim nucleus and GPi effectively resolved the diabetes-induced HH symptoms in our patient. Thus, although certain conclusions cannot be drawn due to the rarity of the surgically treated patients with HH, the combined stimulation is a novel treatment option for resistant HH.
El hemibalismo/hemicorea (HH) es un trastorno del movimiento hipercinético que se observa principalmente en adultos mayores con enfermedades cerebrovasculares. Aunque los síntomas mejoran sin ningún tratamiento, rara vez se requiere la cirugía de lesional o estimulación cerebral profunda (DBS, por sus siglas en inglés) para proporcionar alivio sintomático a los pacientes con movimientos involuntarios graves. La HH es una complicación rara de la diabetes no controlada. Solo hay unos pocos casos reportados de HH diabético que han sido tratados quirúrgicamente. Por lo tanto, en este documento informamos del caso de una mujer de 75 años con diabetes mellitus tipo II que presentó movimientos involuntarios incapacitantes en las extremidades del lado izquierdo, a pesar de haber sido tratada de forma conservadora durante seis meses. Se realizó DBS dirigida al globo pálido interno (GPi) y al núcleo talámico intermedio ventral (Vim). La resolución completa de los síntomas se logró con una estimulación combinada del núcleo talámico Vim (a 1,7 mA) y GPi (a 2,4 mA). La estimulación combinada del núcleo Vim y GPi resolvió eficazmente los síntomas de HH inducidos por la diabetes en nuestro paciente. Por lo tanto, aunque no se pueden sacar ciertas conclusiones debido a la rareza de los pacientes con HH tratados quirúrgicamente, la estimulación combinada es una nueva opción de tratamiento para la HH resistente.
Article

If it is the first time you have accessed you can obtain your credentials by contacting Elsevier Spain in suscripciones@elsevier.com or by calling our Customer Service at902 88 87 40 if you are calling from Spain or at +34 932 418 800 (from 9 to 18h., GMT + 1) if you are calling outside of Spain.
If you already have your login data, please click here .
If you have forgotten your password you can you can recover it by clicking here and selecting the option ¿I have forgotten my password¿.