Share
array:23 [
"pii" => "S2529849624000479"
"issn" => "25298496"
"doi" => "10.1016/j.neucie.2024.07.008"
"estado" => "S200"
"fechaPublicacion" => "2024-08-05"
"aid" => "619"
"copyright" => "Sociedad Española de Neurocirugía"
"copyrightAnyo" => "2024"
"documento" => "article"
"crossmark" => 0
"subdocumento" => "crp"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"Traduccion" => array:1 [
"es" => array:18 [
"pii" => "S1130147324000769"
"issn" => "11301473"
"doi" => "10.1016/j.neucir.2024.07.003"
"estado" => "S200"
"fechaPublicacion" => "2024-08-26"
"aid" => "619"
"copyright" => "Sociedad Española de Neurocirugía"
"documento" => "simple-article"
"crossmark" => 0
"subdocumento" => "crp"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"es" => array:12 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Caso clínico</span>"
"titulo" => "Papel de la craniectomía descompresiva en el edema cerebral fulminante agudo"
"tienePdf" => "es"
"tieneTextoCompleto" => "es"
"tieneResumen" => array:2 [
0 => "es"
1 => "en"
]
"titulosAlternativos" => array:1 [
"en" => array:1 [
"titulo" => "Decompressive craniectomy in the acute fulminant cerebral edema"
]
]
"contieneResumen" => array:2 [
"es" => true
"en" => true
]
"contieneTextoCompleto" => array:1 [
"es" => true
]
"contienePdf" => array:1 [
"es" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:7 [
"identificador" => "fig0010"
"etiqueta" => "Figura 2"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr2.jpeg"
"Alto" => 693
"Ancho" => 1801
"Tamanyo" => 127603
]
]
"descripcion" => array:1 [
"es" => "<p id="spar0030" class="elsevierStyleSimplePara elsevierViewall">Imágenes de resonancia en T2. Tumefacción del parénquima frontotemporal. A) Axial a las 72 horas. B) Coronal a las 72 horas. Cambios secundarios a craniectomía bifrontal. En ambos cortes se observa una importante y extensa tumefacción, con hiperseñal en secuencias potenciadas en T2. Afecta a los núcleos caudados y putámenes respetando tálamo, corteza occipitoparietal y cerebelo. Los hallazgos son compatibles con encefalitis, sin un patrón que sugiera una etiología concreta. C) Corte axial al nivel de la imagen en A, tras la cirugía de craneoplastia a los 21 días tras la cirugía descompresiva. Aumento difuso de la señal en T2 y en localización cortical, subcortical y en menor medida en la sustancia blanca de los lóbulos frontales y parietales y parcheado en los lóbulos occipitales y temporales. En los lóbulos frontales se observan signos de pérdida de volumen. Línea media centrada con tamaño ventricular normal.</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "Aida Antuña Ramos, Juan Mayordomo-Colunga, Raquel Blanco Lago, Marco Antonio Álvarez Vega"
"autores" => array:4 [
0 => array:2 [
"nombre" => "Aida"
"apellidos" => "Antuña Ramos"
]
1 => array:2 [
"nombre" => "Juan"
"apellidos" => "Mayordomo-Colunga"
]
2 => array:2 [
"nombre" => "Raquel"
"apellidos" => "Blanco Lago"
]
3 => array:2 [
"nombre" => "Marco Antonio"
"apellidos" => "Álvarez Vega"
]
]
]
]
]
"idiomaDefecto" => "es"
"Traduccion" => array:1 [
"en" => array:9 [
"pii" => "S2529849624000479"
"doi" => "10.1016/j.neucie.2024.07.008"
"estado" => "S200"
"subdocumento" => ""
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"idiomaDefecto" => "en"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849624000479?idApp=UINPBA00004B"
]
]
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S1130147324000769?idApp=UINPBA00004B"
"url" => "/11301473/unassign/S1130147324000769/v1_202408260353/es/main.assets"
]
]
"itemSiguiente" => array:17 [
"pii" => "S2529849624000480"
"issn" => "25298496"
"doi" => "10.1016/j.neucie.2024.07.009"
"estado" => "S200"
"fechaPublicacion" => "2024-08-14"
"aid" => "621"
"copyright" => "Sociedad Española de Neurocirugía"
"documento" => "article"
"crossmark" => 0
"subdocumento" => "fla"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"en" => array:12 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Clinical Research</span>"
"titulo" => "Effective method of pedicle screw fixation in patients with neurologically intact thoracolumbar burst fractures: a systematic review of studies published over the last 20 years"
"tienePdf" => "en"
"tieneTextoCompleto" => "en"
"tieneResumen" => array:2 [
0 => "en"
1 => "es"
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Método efectivo de fijación con tornillo pedicular en pacientes con fracturas por estallido toracolumbares neurológicamente intactas: una revisión sistemática de estudios publicados en los últimos 20 años"
]
]
"contieneResumen" => array:2 [
"en" => true
"es" => true
]
"contieneTextoCompleto" => array:1 [
"en" => true
]
"contienePdf" => array:1 [
"en" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:8 [
"identificador" => "fig0005"
"etiqueta" => "Fig. 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 3416
"Ancho" => 2925
"Tamanyo" => 510033
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0005"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">PRISMA flowchart for study selection.</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "Andrey Grin, Vasiliy Karanadze, Ivan Lvov, Anton Kordonskiy, Aleksandr Talypov, Vladimir Smirnov, Petr Zakharov"
"autores" => array:7 [
0 => array:2 [
"nombre" => "Andrey"
"apellidos" => "Grin"
]
1 => array:2 [
"nombre" => "Vasiliy"
"apellidos" => "Karanadze"
]
2 => array:2 [
"nombre" => "Ivan"
"apellidos" => "Lvov"
]
3 => array:2 [
"nombre" => "Anton"
"apellidos" => "Kordonskiy"
]
4 => array:2 [
"nombre" => "Aleksandr"
"apellidos" => "Talypov"
]
5 => array:2 [
"nombre" => "Vladimir"
"apellidos" => "Smirnov"
]
6 => array:2 [
"nombre" => "Petr"
"apellidos" => "Zakharov"
]
]
]
]
]
"idiomaDefecto" => "en"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849624000480?idApp=UINPBA00004B"
"url" => "/25298496/unassign/S2529849624000480/v2_202408161126/en/main.assets"
]
"itemAnterior" => array:16 [
"pii" => "S2529849624000352"
"issn" => "25298496"
"doi" => "10.1016/j.neucie.2024.06.003"
"estado" => "S200"
"fechaPublicacion" => "2024-07-11"
"aid" => "615"
"documento" => "article"
"crossmark" => 0
"subdocumento" => "fla"
"abierto" => array:3 [
"ES" => false
"ES2" => false
"LATM" => false
]
"gratuito" => false
"lecturas" => array:1 [
"total" => 0
]
"en" => array:12 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Clinical Research</span>"
"titulo" => "Integrating endovascular techniques into established open neurosurgery practice: a temporal analysis of treatment evolution in a dual-trained neurosurgical unit"
"tienePdf" => "en"
"tieneTextoCompleto" => "en"
"tieneResumen" => array:2 [
0 => "en"
1 => "es"
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Integración de técnicas endovasculares en la práctica de la neurocirugía abierta: análisis temporal de la evolución del tratamiento en una unidad de neurocirugía vascular dual"
]
]
"contieneResumen" => array:2 [
"en" => true
"es" => true
]
"contieneTextoCompleto" => array:1 [
"en" => true
]
"contienePdf" => array:1 [
"en" => true
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:8 [
"identificador" => "fig0005"
"etiqueta" => "Fig. 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 1526
"Ancho" => 2508
"Tamanyo" => 226263
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0005"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">The graph illustrates the evolution of treatment modality preferences over time, as represented by the rolling average proportion of EN (ENDO) and ON (OPEN) neurosurgical procedures. The navy blue line indicates the proportion of OPEN procedures, while the crimson line represents the ENDO procedures.</p>"
]
]
]
"autores" => array:1 [
0 => array:2 [
"autoresLista" => "Ignacio Arrese, Sergio García-García, Santiago Cepeda, Rosario Sarabia"
"autores" => array:4 [
0 => array:2 [
"nombre" => "Ignacio"
"apellidos" => "Arrese"
]
1 => array:2 [
"nombre" => "Sergio"
"apellidos" => "García-García"
]
2 => array:2 [
"nombre" => "Santiago"
"apellidos" => "Cepeda"
]
3 => array:2 [
"nombre" => "Rosario"
"apellidos" => "Sarabia"
]
]
]
]
]
"idiomaDefecto" => "en"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849624000352?idApp=UINPBA00004B"
"url" => "/25298496/unassign/S2529849624000352/v1_202407110420/en/main.assets"
]
"en" => array:18 [
"idiomaDefecto" => true
"cabecera" => "<span class="elsevierStyleTextfn">Case Report</span>"
"titulo" => "Decompressive craniectomy in the acute fulminant cerebral edema"
"tieneTextoCompleto" => true
"autores" => array:1 [
0 => array:4 [
"autoresLista" => "Aida Antuña Ramos, Juan Mayordomo-Colunga, Raquel Blanco Lago, Marco Antonio Álvarez Vega"
"autores" => array:4 [
0 => array:3 [
"nombre" => "Aida"
"apellidos" => "Antuña Ramos"
"referencia" => array:1 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">a</span>"
"identificador" => "aff0005"
]
]
]
1 => array:3 [
"nombre" => "Juan"
"apellidos" => "Mayordomo-Colunga"
"referencia" => array:1 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">b</span>"
"identificador" => "aff0010"
]
]
]
2 => array:3 [
"nombre" => "Raquel"
"apellidos" => "Blanco Lago"
"referencia" => array:1 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">c</span>"
"identificador" => "aff0015"
]
]
]
3 => array:4 [
"nombre" => "Marco Antonio"
"apellidos" => "Álvarez Vega"
"email" => array:1 [
0 => "marcove1@hotmail.com"
]
"referencia" => array:2 [
0 => array:2 [
"etiqueta" => "<span class="elsevierStyleSup">a</span>"
"identificador" => "aff0005"
]
1 => array:2 [
"etiqueta" => "*"
"identificador" => "cor0005"
]
]
]
]
"afiliaciones" => array:3 [
0 => array:3 [
"entidad" => "Departamento de Neurocirugía, Hospital Universitario Central de Asturias, Asturias, Spain"
"etiqueta" => "a"
"identificador" => "aff0005"
]
1 => array:3 [
"entidad" => "Sección de Cuidados Intensivos Pediátricos, Hospital Universitario Central de Asturias, Asturias, Spain"
"etiqueta" => "b"
"identificador" => "aff0010"
]
2 => array:3 [
"entidad" => "AGC Pediatría, Neuropediatria, Hospital Universitario Central de Asturias, Asturias, Spain"
"etiqueta" => "c"
"identificador" => "aff0015"
]
]
"correspondencia" => array:1 [
0 => array:3 [
"identificador" => "cor0005"
"etiqueta" => "⁎"
"correspondencia" => "<span class="elsevierStyleItalic">Corresponding author</span>."
]
]
]
]
"titulosAlternativos" => array:1 [
"es" => array:1 [
"titulo" => "Papel de la craniectomía descompresiva en el edema cerebral fulminante agudo"
]
]
"resumenGrafico" => array:2 [
"original" => 0
"multimedia" => array:8 [
"identificador" => "fig0005"
"etiqueta" => "Fig. 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 505
"Ancho" => 1347
"Tamanyo" => 93972
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0005"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
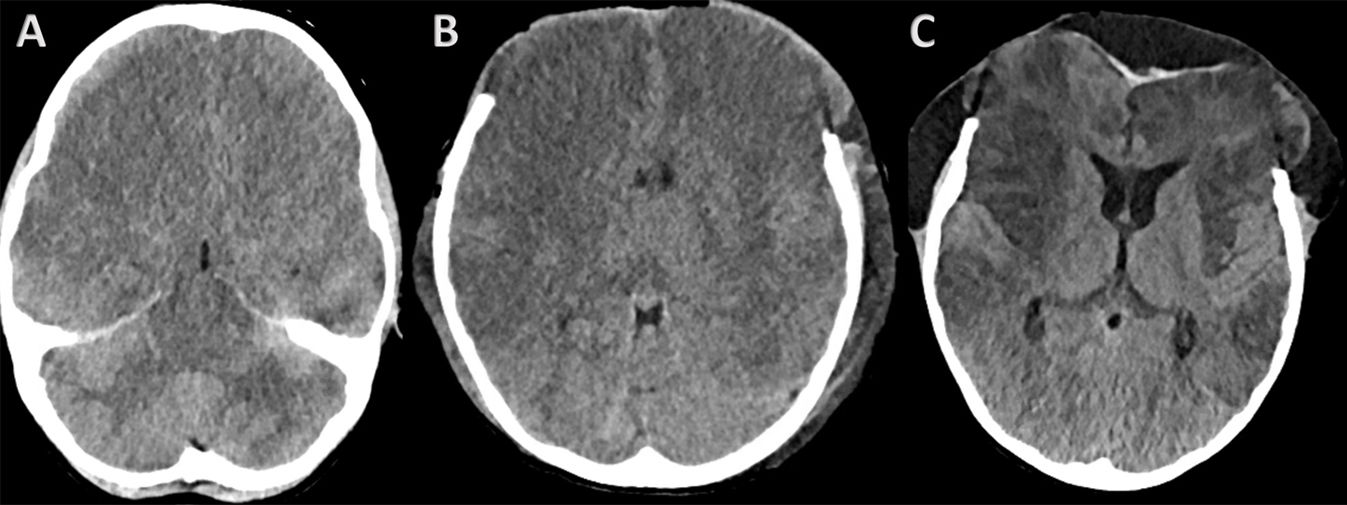
"en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Brain computed tomography (CT) images (A) CT scan prior to surgical indication: loss of cortico-subcortical differentiation symmetrically and bilaterally in both frontal lobes and anterior portion of parietal and temporal lobes. Also visible are complete collapse of the sulci of both convexities and a decrease in the subarachnoid cisterns and almost complete collapse of the 4th ventricle. These findings are consistent with diffuse cerebral oedema. (B) CT scan 24 h after surgery: postoperative changes secondary to bilateral frontal craniectomy. Significant loss of cortico-subcortical differentiation suggestive of diffuse cerebral oedema still identifiable. Slight improvement in bilateral frontal basal parenchymal density and slight re-expansion of the 4th ventricle. (C) CT scan prior to bone replacement: 21 days after surgery. Postoperative changes showing an extra-axial frontal hypodense collection. The lesions are more sharply defined and hypodense than in the previous study.</p>"
]
]
]
"textoCompleto" => "<span class="elsevierStyleSections"><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0025">Introduction</span><p id="par0055" class="elsevierStylePara elsevierViewall">Acute fulminant cerebral oedema (AFCO) is a clinical manifestation of encephalitis occurring in the paediatric age group. The signs and symptoms are rapidly progressive and it has significant morbidity and mortality rates.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> It is a recently recognised condition, which may be triggered by common paediatric infections or have no obvious cause.<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a></p><p id="par0060" class="elsevierStylePara elsevierViewall">Although the indication for decompressive craniectomy in the treatment of refractory intracranial hypertension secondary to encephalitis is described in the literature<a class="elsevierStyleCrossRef" href="#bib0015"><span class="elsevierStyleSup">3</span></a> as a second-level measure, in this condition, cerebral oedema occurs very quickly and is also refractory to the different drug treatments.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> Therefore, in order to avoid brain damage due to hypoxia and/or ischaemia secondary to increased intracranial pressure, intracranial pressure monitoring and decompressive craniectomy should be considered early options in the therapy scale for cerebral oedema.<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a> The aim should be not only to increase survival but also to improve functional prognosis.<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a></p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0030">Case report</span><p id="par0065" class="elsevierStylePara elsevierViewall">This was an eight-year-old boy with predominantly gastrointestinal symptoms accompanied by fever of two days' duration. No relevant medical history was reported and he was fully vaccinated for his age, including meningococcal vaccination. He was admitted to the paediatric ward for investigation. The day after admission, he developed an episode of aphasia and somnolence. Brain scan and a brain MRI were performed and reported as normal. A cerebrospinal fluid (CSF) sample was also taken by lumbar puncture with the following results: Leucocytes 20/μl * (0–7); Lymphocytes 97% * (100−100); Polynuclear 3%; Glucose 62 mg/dl (45–75); Total Proteins 29.7 mg/dl (10.0–45.0). FilmArray study of cerebrospinal fluid was negative. Clinical examination revealed bilateral Babinski reflex, exaggeration of the osteotendinous reflexes and sucking and chewing movements. No rash or petechiae were evident on the skin. Treatment with aciclovir at a dose of 60 mg/kg/day was started on suspicion of viral encephalitis.</p><p id="par0070" class="elsevierStylePara elsevierViewall">Within 48 h, he suffered an epileptic seizure, with a decrease in his level of consciousness, requiring orotracheal intubation and mechanical ventilation. At this point, he was started on treatment with non-specific human immunoglobulin 2 mg/kg and methylprednisolone 30 mg/kg/day for three days, due to the likelihood of autoimmune encephalitis. Although the patient was afebrile on admission to the intensive care unit, Augmentin 100 mg/kg/day empirically and Septrin 5 mg/kg/day as prophylaxis were added to his treatment.</p><p id="par0075" class="elsevierStylePara elsevierViewall">Following this acute clinical deterioration, a repeat brain scan was performed (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>), showing a symmetrical, bilateral loss of cortico-subcortical differentiation in both frontal and temporal lobes and in the anterior portion of the parietal lobes. Also visible was complete collapse of the sulci of both convexities and a decrease in the subarachnoid cisterns. Virtually complete collapse of the IV ventricle was reported, with no associated supratentorial ventricular system dilation and no signs of periependymal transudation. All these findings are consistent with diffuse cerebral oedema.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0080" class="elsevierStylePara elsevierViewall">An electroencephalogram was also performed, which showed slowed brain activity, consistent with severe, non-specific diffuse encephalopathy, without epileptiform activity.</p><p id="par0085" class="elsevierStylePara elsevierViewall">The patient developed bradycardia, hypertension and anisocoria with disappearance of the pupillary light reflex. An intraparenchymal sensor was then placed for intracranial pressure monitoring and, with high pressures found, treatment was started with 3% hypertonic saline and 20% mannitol. Although initially the patient's intracranial pressure was controlled with these measures, over the following hours, values above 40 mmHg were maintained, and so, 72 h after admission, it was decided to proceed with an urgent surgical intervention to perform a bilateral frontal decompressive craniectomy. The parenchyma had a congestive and oedematous appearance, protruding outside the bony ridge and with a very weak pulse, but without macroscopic evidence of an infectious component.</p><p id="par0090" class="elsevierStylePara elsevierViewall">After surgery, intracranial pressure monitoring showed values maintained within normal ranges. Three days after the operation, a repeat brain MRI was performed (<a class="elsevierStyleCrossRef" href="#fig0010">Fig. 2</a>), which showed a significant and extensive parenchymal tumour with thickening of the cerebral cortex of the bilateral frontotemporal convexity and hypersignal in T2-weighted, flair and diffusion sequences, with restriction in the diffusion sequence at the cortico-subcortical junction. Although to a lesser extent, both caudate and putamen nuclei were also affected, with patchy involvement of the pons. The findings described are consistent with encephalitis.</p><elsevierMultimedia ident="fig0010"></elsevierMultimedia><p id="par0095" class="elsevierStylePara elsevierViewall">All other studies performed (virology and viral serology, blood cultures, cerebrospinal fluid cultures, metabolic studies, porphyria screening and studies of immunity, and ammonium and toxic levels) were negative. It was ultimately judged to be autoimmune encephalopathy. In view of this suspected diagnosis, seven plasmapheresis procedures and four doses of rituximab 375 mg/m<span class="elsevierStyleSup">2</span> were added to the general supportive care.</p><p id="par0100" class="elsevierStylePara elsevierViewall">We were able to extubate the patient 12 days after surgery. At that time, clinical examination revealed acquired neurological damage consisting of spastic quadriparesis and impaired language and connection with the environment.</p><p id="par0105" class="elsevierStylePara elsevierViewall">Three weeks after the decompressive craniectomy, bone repositioning with autologous flap was performed. Rehabilitation therapy was started at the same time, with progressive improvement of all motor and language functions. Three months after the onset of the condition, the patient is able to mobilise independently and communicate in simple sentences, with his final neurocognitive status still to be assessed. He is currently undergoing neuro-specific rehabilitation at a referral centre.</p></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0035">Discussion</span><p id="par0110" class="elsevierStylePara elsevierViewall">Encephalitis is defined as an inflammatory process in the brain parenchyma, which is associated with obvious clinical signs of neurological dysfunction.<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a> It may result from a direct infection of brain tissue (infectious encephalitis) or from an immune process (autoimmune encephalitis). In infectious encephalitis, if the causative agent spreads to neighbouring structures (meninges or spinal cord), we may have mixed pictures of meningoencephalitis or encephalomyelitis.</p><p id="par0115" class="elsevierStylePara elsevierViewall">The mortality rate for encephalitis in the paediatric population has been estimated at 3% and has been linked to HSV and Enterovirus A71 aetiology.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">6</span></a></p><p id="par0120" class="elsevierStylePara elsevierViewall">For the diagnosis of encephalitis of infectious origin, the criteria of The International Encephalitis Consortium (IEC<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a> can be used, which establishes major and minor criteria. The major (essential) criterion is the presence of encephalopathy, defined as an altered mental status (decreased level of consciousness, lethargy or personality changes) of at least 24 h' duration with no other identified cause. Minor criteria include: (a) fever >38 °C within 72 h before or after clinical onset; (b) partial or generalised seizures without previous epileptogenic pathology; (c) appearance of a new focal neurological sign; (d) CSF pleocytosis; (e) abnormal electroencephalogram (EEG) consistent with suspected encephalitis not attributable to other causes; and (f) abnormalities in the brain parenchyma on neuroimaging tests. Possible encephalitis is considered with one major and two minor criteria and probable encephalitis with three or more minor criteria. Confirmation requires an anatomical-pathological diagnosis (following autopsy or biopsy of brain tissue) or identification of a causative microorganism (<a class="elsevierStyleCrossRef" href="#tbl0005">Table 1</a>).</p><elsevierMultimedia ident="tbl0005"></elsevierMultimedia><p id="par0125" class="elsevierStylePara elsevierViewall">In the case of autoimmune encephalitis, fever and CSF pleocytosis are less common, and abnormal EEGs are less specific. Diagnostic confirmation requires immunological and antibody studies, which can take weeks to obtain. For all these reasons, we propose the diagnostic criteria published by Graus,<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">7</span></a> which suggest a possible diagnosis of autoimmune encephalitis from the onset of the clinical signs and symptoms. The following three criteria must be met: (a) subacute onset of memory deficits, mental status changes or psychiatric symptoms; (b) at least one of the following; new onset of focal neurological signs, epileptic seizure without previous epileptogenic pathology, CSF pleocytosis and brain MRI findings consistent with encephalitis; (c) exclusion of other causes of encephalitis (<a class="elsevierStyleCrossRef" href="#tbl0005">Table 1</a>).</p><p id="par0130" class="elsevierStylePara elsevierViewall">The above case is an example of the rapid neurological deterioration that characterises AFCO. It corresponds to a phenotype within encephalitis with a worse prognosis due to increased intracranial pressure and a more acute clinical pattern.<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a></p><p id="par0135" class="elsevierStylePara elsevierViewall">The incidence of AFCO in paediatric encephalitis is around 2%.<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a> It is defined as: (a) rapid and progressive elevation of intracranial pressure accompanied by neurological deterioration (Glasgow Coma Scale, GCS < 8) and signs of brainstem dysfunction; and (b) appearance on neuroimaging tests, either CT or MRI, of impending brain herniation or herniation with brainstem compression<a class="elsevierStyleCrossRefs" href="#bib0005"><span class="elsevierStyleSup">1,8,9</span></a> (<a class="elsevierStyleCrossRef" href="#tbl0005">Table 1</a>). The outcome and prognosis will be better in patients who undergo surgical decompression than those who receive only medical treatment,<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">10</span></a> especially if it is performed in the early stages of brain stem dysfunction,<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">9</span></a> as in the case described here.</p><p id="par0140" class="elsevierStylePara elsevierViewall">Most of the recently published articles<a class="elsevierStyleCrossRefs" href="#bib0005"><span class="elsevierStyleSup">1,11</span></a> refer to isolated cases. A case series reported in the literature<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a> in which no surgical treatment was considered for any of the patients reports high rates of mortality and neurological sequelae (64% mortality and 36% vegetative state or severe neurological sequelae).<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a> However, a second case series reports favourable results in terms of survival and neurological recovery in all patients in whom decompressive craniectomy was performed<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">10</span></a> (4% mortality and 81% good neurological recovery).</p><p id="par0145" class="elsevierStylePara elsevierViewall">The pathophysiology of acute fulminant cerebral oedema is probably due to a combination of factors, including hypoxic-ischaemic brain damage, systemic inflammatory response and genetic predisposition.<a class="elsevierStyleCrossRef" href="#bib0055"><span class="elsevierStyleSup">11</span></a></p><p id="par0150" class="elsevierStylePara elsevierViewall">As in our case, normal radiological tests at the onset do not rule out the possibility of developing AFCO, with neuroimaging findings not abnormal until 24−48 hours after the onset of symptoms.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2,4</span></a></p><p id="par0155" class="elsevierStylePara elsevierViewall">There are no established parameters defining which cases of encephalitis will progress to AFCO, but the presence of seizures, status epilepticus, and the appearance within the first three days of neurological signs and symptoms or signs of brain herniation, point to a higher likelihood of developing fulminant oedema.<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a> Therefore, even if the initial treatment for intracranial hypertension is medical (hyperosmolar therapy, hyperventilation), lack of rapid response to these treatments should not delay decompressive surgery.<a class="elsevierStyleCrossRefs" href="#bib0020"><span class="elsevierStyleSup">4,12</span></a></p><p id="par0160" class="elsevierStylePara elsevierViewall">In this case, no brain biopsy was performed as the brain was found to be congestive overall, but with no clearly differentiated pathological areas either radiologically or surgically. However, a targeted brain biopsy of magnetic resonance imaging abnormalities may be necessary when the diagnosis remains uncertain after the initial study.<a class="elsevierStyleCrossRef" href="#bib0065"><span class="elsevierStyleSup">13</span></a> The diagnostic yield of brain biopsy is higher in paediatric patients than in adults,<a class="elsevierStyleCrossRef" href="#bib0070"><span class="elsevierStyleSup">14</span></a> but it should be borne in mind that biopsy is not free of complications, especially in patients in a clinical situation requiring admission to an intensive care unit.<a class="elsevierStyleCrossRef" href="#bib0075"><span class="elsevierStyleSup">15</span></a> Therefore, biopsy could be considered in cases of encephalitis where a causative microorganism has not been obtained and the suspicion of autoimmune encephalitis is not a likely diagnosis that could be confirmed by immunological and autoantibody studies.</p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0040">Conclusions</span><p id="par0165" class="elsevierStylePara elsevierViewall">We have presented here the report of a case with clinical signs that progressed to the development of acute fulminant cerebral oedema, which included rapid neurological deterioration, increased intracranial pressure and radiological signs of brain herniation.</p><p id="par0170" class="elsevierStylePara elsevierViewall">Intracranial pressure monitoring and early decompressive craniectomy were necessary due to lack of response to medical treatment.</p><p id="par0175" class="elsevierStylePara elsevierViewall">The aim of decompressive craniectomy should not only be to increase survival but also to reduce neurological sequelae. Biopsy should be considered during surgery in certain cases where it may help to complete diagnostic studies.</p></span><span id="sec0025" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0045">Funding</span><p id="par0180" class="elsevierStylePara elsevierViewall">This article received no funding from public, private or non-profit organisations.</p></span><span id="sec0030" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0050">Conflicts of interest</span><p id="par0185" class="elsevierStylePara elsevierViewall">The authors declare that they have no conflicts of interest.</p></span></span>"
"textoCompletoSecciones" => array:1 [
"secciones" => array:11 [
0 => array:3 [
"identificador" => "xres2215461"
"titulo" => "Abstract"
"secciones" => array:1 [
0 => array:1 [
"identificador" => "abst0005"
]
]
]
1 => array:2 [
"identificador" => "xpalclavsec1857318"
"titulo" => "Keywords"
]
2 => array:3 [
"identificador" => "xres2215462"
"titulo" => "Resumen"
"secciones" => array:1 [
0 => array:1 [
"identificador" => "abst0010"
]
]
]
3 => array:2 [
"identificador" => "xpalclavsec1857317"
"titulo" => "Palabras clave"
]
4 => array:2 [
"identificador" => "sec0005"
"titulo" => "Introduction"
]
5 => array:2 [
"identificador" => "sec0010"
"titulo" => "Case report"
]
6 => array:2 [
"identificador" => "sec0015"
"titulo" => "Discussion"
]
7 => array:2 [
"identificador" => "sec0020"
"titulo" => "Conclusions"
]
8 => array:2 [
"identificador" => "sec0025"
"titulo" => "Funding"
]
9 => array:2 [
"identificador" => "sec0030"
"titulo" => "Conflicts of interest"
]
10 => array:1 [
"titulo" => "References"
]
]
]
"pdfFichero" => "main.pdf"
"tienePdf" => true
"fechaRecibido" => "2024-04-02"
"fechaAceptado" => "2024-07-06"
"PalabrasClave" => array:2 [
"en" => array:1 [
0 => array:4 [
"clase" => "keyword"
"titulo" => "Keywords"
"identificador" => "xpalclavsec1857318"
"palabras" => array:4 [
0 => "Acute fulminant cerebral edema"
1 => "Encephalitis"
2 => "Decompressive craniectomy"
3 => "Pediatric age"
]
]
]
"es" => array:1 [
0 => array:4 [
"clase" => "keyword"
"titulo" => "Palabras clave"
"identificador" => "xpalclavsec1857317"
"palabras" => array:4 [
0 => "Edema cerebral agudo fulminante"
1 => "Encefalitis"
2 => "Craniectomía descompresiva"
3 => "Edad pediátrica"
]
]
]
]
"tieneResumen" => true
"resumen" => array:2 [
"en" => array:2 [
"titulo" => "Abstract"
"resumen" => "<span id="abst0005" class="elsevierStyleSection elsevierViewall"><p id="spar0040" class="elsevierStyleSimplePara elsevierViewall">Acute fulminant cerebral edema is a type of rapidly progressive encephalitis that occurs in children and is associated with significant morbidity and mortality.</p><p id="spar0045" class="elsevierStyleSimplePara elsevierViewall">We present a clinical case with seizures, rapid neurological deterioration and the early appearance of cerebral herniation signs. Although the radiological tests were initially normal and there are no established parameters that predict the evolution of encephalitis to a rapidly progressive subtype, the clinical evolution forced to consider the decompressive craniectomy due to the lack of response to the medical management of the cerebral edema. It may be necessary take a brain biopsy to confirm the etiology of the encephalitis origin of acute fulminant cerebral edema. The objective of surgery should be not only to increase survival, but also to reduce subsequent neurological sequelae.</p></span>"
]
"es" => array:2 [
"titulo" => "Resumen"
"resumen" => "<span id="abst0010" class="elsevierStyleSection elsevierViewall"><p id="spar0050" class="elsevierStyleSimplePara elsevierViewall">El edema cerebral fulminante agudo es un cuadro clínico dentro de las encefalitis con una evolución rápidamente progresiva de aparición en la edad pediátrica y que se asocia a una importante morbimortalidad.</p><p id="spar0055" class="elsevierStyleSimplePara elsevierViewall">Presentamos un caso clínico que cursa con crisis comiciales, deterioro neurológico rápido y la aparición precoz de signos de herniación cerebral. Aunque las pruebas radiológicas fueron normales inicialmente y no hay establecidos parámetros que predigan la evolución de encefalitis a un subtipo rápidamente progresiva, la evolución clínica que presentó obligó a la realización de una craniectomía descompresiva ante la falta de respuesta al manejo médico del edema cerebral. En ocasiones puede ser necesario la toma de una biopsia cerebral para llegar al diagnóstico de la causa que ha producido la encefalitis origen del edema cerebral agudo fulminante. El objetivo de la cirugía debe ser no sólo el aumento de la supervivencia, sino la disminución de las secuelas neurológicas posteriores.</p></span>"
]
]
"multimedia" => array:3 [
0 => array:8 [
"identificador" => "fig0005"
"etiqueta" => "Fig. 1"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr1.jpeg"
"Alto" => 505
"Ancho" => 1347
"Tamanyo" => 93972
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0005"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
"en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Brain computed tomography (CT) images (A) CT scan prior to surgical indication: loss of cortico-subcortical differentiation symmetrically and bilaterally in both frontal lobes and anterior portion of parietal and temporal lobes. Also visible are complete collapse of the sulci of both convexities and a decrease in the subarachnoid cisterns and almost complete collapse of the 4th ventricle. These findings are consistent with diffuse cerebral oedema. (B) CT scan 24 h after surgery: postoperative changes secondary to bilateral frontal craniectomy. Significant loss of cortico-subcortical differentiation suggestive of diffuse cerebral oedema still identifiable. Slight improvement in bilateral frontal basal parenchymal density and slight re-expansion of the 4th ventricle. (C) CT scan prior to bone replacement: 21 days after surgery. Postoperative changes showing an extra-axial frontal hypodense collection. The lesions are more sharply defined and hypodense than in the previous study.</p>"
]
]
1 => array:8 [
"identificador" => "fig0010"
"etiqueta" => "Fig. 2"
"tipo" => "MULTIMEDIAFIGURA"
"mostrarFloat" => true
"mostrarDisplay" => false
"figura" => array:1 [
0 => array:4 [
"imagen" => "gr2.jpeg"
"Alto" => 693
"Ancho" => 1801
"Tamanyo" => 127603
]
]
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0010"
"detalle" => "Fig. "
"rol" => "short"
]
]
"descripcion" => array:1 [
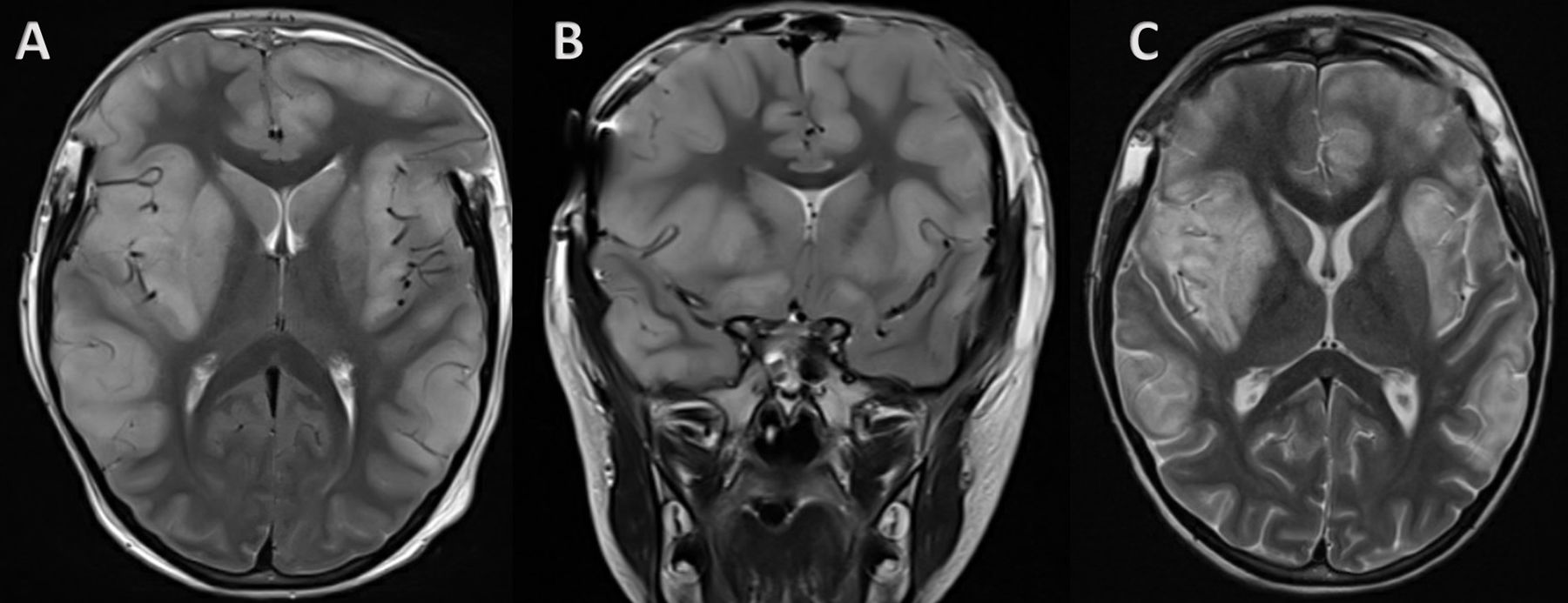
"en" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">T2-weighted magnetic resonance images. Frontotemporal parenchymal swelling. (A) Axial at 72 h. (B) Coronal at 72 h. Changes secondary to bilateral frontal craniectomy. Both slices show significant and extensive swelling, with hypersignal on T2-weighted sequences. It affects the caudate and putamen nuclei while respecting the thalamus, occipitoparietal cortex and cerebellum. The findings are consistent with encephalitis, with no pattern suggesting a specific aetiology. (C) Axial slice at the level of the image in A, after cranioplasty surgery 21 days after the decompressive surgery. Diffuse signal enhancement on T2-weighted images and in cortical and subcortical locations, and to a lesser extent in the white matter of the frontal and parietal lobes and patchy in the occipital and temporal lobes Signs of volume loss can be seen in the frontal lobes. Centred midline with normal ventricle size.</p>"
]
]
2 => array:8 [
"identificador" => "tbl0005"
"etiqueta" => "Table 1"
"tipo" => "MULTIMEDIATABLA"
"mostrarFloat" => true
"mostrarDisplay" => false
"detalles" => array:1 [
0 => array:3 [
"identificador" => "at0015"
"detalle" => "Table "
"rol" => "short"
]
]
"tabla" => array:2 [
"leyenda" => "<p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">CSF: cerebrospinal fluid. EEG: electroencephalogram.</p><p id="spar0025" class="elsevierStyleSimplePara elsevierViewall">Infectious encephalitis: one major criterion and at least two minor criteria.</p><p id="spar0030" class="elsevierStyleSimplePara elsevierViewall">Autoimmune encephalitis: at least one of each of the criteria.</p><p id="spar0035" class="elsevierStyleSimplePara elsevierViewall">Fulminant cerebral oedema: all three criteria.</p>"
"tablatextoimagen" => array:1 [
0 => array:2 [
"tabla" => array:1 [
0 => """
<table border="0" frame="\n
\t\t\t\t\tvoid\n
\t\t\t\t" class=""><thead title="thead"><tr title="table-row"><th class="td" title="\n
\t\t\t\t\ttable-head\n
\t\t\t\t " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t" scope="col" style="border-bottom: 2px solid black">Infectious encephalitis \t\t\t\t\t\t\n
\t\t\t\t\t\t</th><th class="td" title="\n
\t\t\t\t\ttable-head\n
\t\t\t\t " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t" scope="col" style="border-bottom: 2px solid black">Autoimmune encephalitis \t\t\t\t\t\t\n
\t\t\t\t\t\t</th><th class="td" title="\n
\t\t\t\t\ttable-head\n
\t\t\t\t " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t" scope="col" style="border-bottom: 2px solid black">Fulminant cerebral oedema \t\t\t\t\t\t\n
\t\t\t\t\t\t</th></tr></thead><tbody title="tbody"><tr title="table-row"><td class="td-with-role" title="\n
\t\t\t\t\ttable-entry\n
\t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t">Major criterion: altered mental status \t\t\t\t\t\t\n
\t\t\t\t</td><td class="td" title="\n
\t\t\t\t\ttable-entry\n
\t\t\t\t " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t">Altered mental status \t\t\t\t\t\t\n
\t\t\t\t</td><td class="td" title="\n
\t\t\t\t\ttable-entry\n
\t\t\t\t " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t">Increased intracranial pressure with neurological deterioration \t\t\t\t\t\t\n
\t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n
\t\t\t\t\ttable-entry\n
\t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t">Minor criteria:<ul class="elsevierStyleList" id="lis0005"><li class="elsevierStyleListItem" id="lsti0005"><span class="elsevierStyleLabel">a</span><p id="par0005" class="elsevierStylePara elsevierViewall">Fever >38 °C</p></li><li class="elsevierStyleListItem" id="lsti0010"><span class="elsevierStyleLabel">b</span><p id="par0010" class="elsevierStylePara elsevierViewall">Partial or generalised seizures</p></li><li class="elsevierStyleListItem" id="lsti0015"><span class="elsevierStyleLabel">c</span><p id="par0015" class="elsevierStylePara elsevierViewall">New focal neurological signs</p></li><li class="elsevierStyleListItem" id="lsti0020"><span class="elsevierStyleLabel">d</span><p id="par0020" class="elsevierStylePara elsevierViewall">CSF pleocytosis</p></li><li class="elsevierStyleListItem" id="lsti0025"><span class="elsevierStyleLabel">e</span><p id="par0025" class="elsevierStylePara elsevierViewall">Abnormal EEG</p></li><li class="elsevierStyleListItem" id="lsti0030"><span class="elsevierStyleLabel">f</span><p id="par0030" class="elsevierStylePara elsevierViewall">Abnormalities in neuroimaging tests</p></li></ul> \t\t\t\t\t\t\n
\t\t\t\t</td><td class="td" title="\n
\t\t\t\t\ttable-entry\n
\t\t\t\t " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t"><ul class="elsevierStyleList" id="lis0010"><li class="elsevierStyleListItem" id="lsti0035"><span class="elsevierStyleLabel">a</span><p id="par0035" class="elsevierStylePara elsevierViewall">Partial or generalised seizures</p></li><li class="elsevierStyleListItem" id="lsti0040"><span class="elsevierStyleLabel">b</span><p id="par0040" class="elsevierStylePara elsevierViewall">New focal neurological signs</p></li><li class="elsevierStyleListItem" id="lsti0045"><span class="elsevierStyleLabel">c</span><p id="par0045" class="elsevierStylePara elsevierViewall">CSF pleocytosis</p></li><li class="elsevierStyleListItem" id="lsti0050"><span class="elsevierStyleLabel">d</span><p id="par0050" class="elsevierStylePara elsevierViewall">Abnormalities in neuroimaging tests</p></li></ul> \t\t\t\t\t\t\n
\t\t\t\t</td><td class="td" title="\n
\t\t\t\t\ttable-entry\n
\t\t\t\t " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t">Signs of brainstem dysfunction \t\t\t\t\t\t\n
\t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n
\t\t\t\t\ttable-entry\n
\t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t"> \t\t\t\t\t\t\n
\t\t\t\t</td><td class="td" title="\n
\t\t\t\t\ttable-entry\n
\t\t\t\t " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t">Exclusion of other causes of encephalitis \t\t\t\t\t\t\n
\t\t\t\t</td><td class="td" title="\n
\t\t\t\t\ttable-entry\n
\t\t\t\t " align="left" valign="\n
\t\t\t\t\ttop\n
\t\t\t\t">Brain herniation on neuroimaging tests \t\t\t\t\t\t\n
\t\t\t\t</td></tr></tbody></table>
"""
]
"imagenFichero" => array:1 [
0 => "xTab3613162.png"
]
]
]
]
"descripcion" => array:1 [
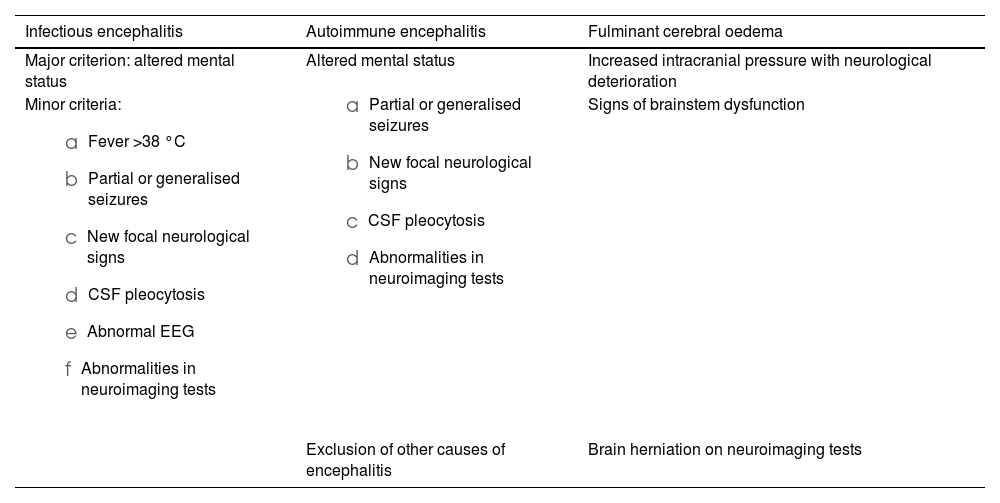
"en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Diagnostic criteria for infectious and autoimmune encephalitis and fulminant cerebral oedema.</p>"
]
]
]
"bibliografia" => array:2 [
"titulo" => "References"
"seccion" => array:1 [
0 => array:2 [
"identificador" => "bibs0005"
"bibliografiaReferencia" => array:15 [
0 => array:3 [
"identificador" => "bib0005"
"etiqueta" => "1"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Acute fulminant cerebral edema in a child with suspected meningoencephalitis"
"autores" => array:1 [
0 => array:2 [
"etal" => true
"autores" => array:6 [
0 => "S. Monteiro"
1 => "B. Teixeira"
2 => "C. Fraga"
3 => "A. Dias"
4 => "A.L. Cardoso"
5 => "D. Meireles"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.7759/cureus.45339"
"Revista" => array:4 [
"tituloSerie" => "Cureus"
"fecha" => "2023"
"volumen" => "15"
"numero" => "9"
]
]
]
]
]
]
1 => array:3 [
"identificador" => "bib0010"
"etiqueta" => "2"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Acute fulminant cerebral edema: a newly recognized phenotype in children with suspected encephalitis"
"autores" => array:1 [
0 => array:2 [
"etal" => true
"autores" => array:6 [
0 => "P. Krishnan"
1 => "O.A. Glenn"
2 => "M.C. Samuel"
3 => "H. Sheriff"
4 => "A. Foster-Barber"
5 => "J.J. Sejvar"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/jpids/piaa063"
"Revista" => array:7 [
"tituloSerie" => "J Pediatric Infect Dis Soc"
"fecha" => "2021"
"volumen" => "10"
"numero" => "3"
"paginaInicial" => "289"
"paginaFinal" => "294"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/32667036"
"web" => "Medline"
]
]
]
]
]
]
]
]
2 => array:3 [
"identificador" => "bib0015"
"etiqueta" => "3"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Papel de la craniectomía descompresiva en el tratamiento de la hipertensión intracraneal refractaria, secundaria a encefalitis [The role of decompressive craniectomy in management of refractory intracranial hypertension due to encephalitis]"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:4 [
0 => "C. Cayuela Guerrero"
1 => "F.J. Cambra Lasaosa"
2 => "A. Palomeque Rico"
3 => "A. Guillen Quesada"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.anpedi.2011.12.007"
"Revista" => array:8 [
"tituloSerie" => "An Pediatr (Barc)"
"fecha" => "2014"
"volumen" => "80"
"numero" => "1"
"paginaInicial" => "e12"
"paginaFinal" => "e13"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/22326637"
"web" => "Medline"
]
]
"itemHostRev" => array:3 [
"pii" => "S2215036621000912"
"estado" => "S300"
"issn" => "22150366"
]
]
]
]
]
]
]
3 => array:3 [
"identificador" => "bib0020"
"etiqueta" => "4"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Analysis of fulminant cerebral edema in acute pediatric encephalitis"
"autores" => array:1 [
0 => array:3 [
"colaboracion" => "CHEESE Study Group"
"etal" => false
"autores" => array:6 [
0 => "S.Y. Lan"
1 => "J.J. Lin"
2 => "S.H. Hsia"
3 => "H.S. Wang"
4 => "C.H. Chiu"
5 => "K.L. Lin"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.pedneo.2015.11.002"
"Revista" => array:8 [
"tituloSerie" => "Pediatr Neonatol."
"fecha" => "2016"
"volumen" => "57"
"numero" => "5"
"paginaInicial" => "402"
"paginaFinal" => "407"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/26852357"
"web" => "Medline"
]
]
"itemHostRev" => array:3 [
"pii" => "S2215036620301425"
"estado" => "S300"
"issn" => "22150366"
]
]
]
]
]
]
]
4 => array:3 [
"identificador" => "bib0025"
"etiqueta" => "5"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium"
"autores" => array:1 [
0 => array:3 [
"colaboracion" => "International Encephalitis Consortium"
"etal" => true
"autores" => array:6 [
0 => "A. Venkatesan"
1 => "A.R. Tunkel"
2 => "K.C. Bloch"
3 => "A.S. Lauring"
4 => "J. Sejvar"
5 => "A. Bitnun"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1093/cid/cit458"
"Revista" => array:7 [
"tituloSerie" => "Clin Infect Dis."
"fecha" => "2013"
"volumen" => "57"
"numero" => "8"
"paginaInicial" => "1114"
"paginaFinal" => "1128"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/23861361"
"web" => "Medline"
]
]
]
]
]
]
]
]
5 => array:3 [
"identificador" => "bib0030"
"etiqueta" => "6"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Sociedad y fundación española de cuidados intensivos pediátricos"
"autores" => array:1 [
0 => array:2 [
"colaboracion" => "SECIP"
"etal" => false
]
]
]
]
"host" => array:2 [
0 => array:1 [
"Libro" => array:1 [
"fecha" => "2023"
]
]
1 => array:1 [
"WWW" => array:1 [
"link" => "https://secip.com/index.php/publicaciones/protocolos"
]
]
]
]
]
]
6 => array:3 [
"identificador" => "bib0035"
"etiqueta" => "7"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "A clinical approach to diagnosis of autoimmune encephalitis"
"autores" => array:1 [
0 => array:2 [
"etal" => true
"autores" => array:6 [
0 => "F. Graus"
1 => "M.J. Titulaer"
2 => "R. Balu"
3 => "S. Benseler"
4 => "C.G. Bien"
5 => "T. Cellucci"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/S1474-4422(15)00401-9"
"Revista" => array:7 [
"tituloSerie" => "Lancet Neurol."
"fecha" => "2016"
"volumen" => "15"
"numero" => "4"
"paginaInicial" => "391"
"paginaFinal" => "404"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/26906964"
"web" => "Medline"
]
]
]
]
]
]
]
]
7 => array:3 [
"identificador" => "bib0040"
"etiqueta" => "8"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Raised intracranial pressure in acute viral encephalitis"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:3 [
0 => "G. Kumar"
1 => "J. Kalita"
2 => "U.K. Misra"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1016/j.clineuro.2009.03.004"
"Revista" => array:7 [
"tituloSerie" => "Clin Neurol Neurosurg"
"fecha" => "2009"
"volumen" => "111"
"numero" => "5"
"paginaInicial" => "399"
"paginaFinal" => "406"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/19372001"
"web" => "Medline"
]
]
]
]
]
]
]
]
8 => array:3 [
"identificador" => "bib0045"
"etiqueta" => "9"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Emergency decompressive craniectomy for fulminating infectious encephalitis"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:2 [
0 => "M.A. Adamo"
1 => "E.M. Deshaies"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.3171/JNS/2008/108/01/0174"
"Revista" => array:8 [
"tituloSerie" => "J Neurosurg"
"fecha" => "2008"
"volumen" => "108"
"numero" => "1"
"paginaInicial" => "174"
"paginaFinal" => "176"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/18173329"
"web" => "Medline"
]
]
"itemHostRev" => array:3 [
"pii" => "S2215036614001187"
"estado" => "S300"
"issn" => "22150366"
]
]
]
]
]
]
]
9 => array:3 [
"identificador" => "bib0050"
"etiqueta" => "10"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Decompressive craniectomy for encephalitis with brain herniation: case report and review of the literature"
"autores" => array:1 [
0 => array:2 [
"etal" => true
"autores" => array:6 [
0 => "J. Pérez-Bovet"
1 => "R. Garcia-Armengol"
2 => "M. Buxó-Pujolràs"
3 => "N. Lorite-Díaz"
4 => "Y. Narváez-Martínez"
5 => "J.L. Caro-Cardera"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1007/s00701-012-1323-3"
"Revista" => array:7 [
"tituloSerie" => "Acta Neurochir (Wien)."
"fecha" => "2012"
"volumen" => "154"
"numero" => "9"
"paginaInicial" => "1717"
"paginaFinal" => "1724"
"itemHostRev" => array:3 [
"pii" => "S2215036620301413"
"estado" => "S300"
"issn" => "22150366"
]
]
]
]
]
]
]
10 => array:3 [
"identificador" => "bib0055"
"etiqueta" => "11"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Acute fulminant cerebral edema caused by influenza type B in an 18-year-old female: a rare case"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:4 [
0 => "L.E. Santiago"
1 => "A.T. Alvi"
2 => "Z. Nadeem"
3 => "A. Chaudhry"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.7759/cureus.45501"
"Revista" => array:4 [
"tituloSerie" => "Cureus"
"fecha" => "2023"
"volumen" => "15"
"numero" => "9"
]
]
]
]
]
]
11 => array:3 [
"identificador" => "bib0060"
"etiqueta" => "12"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Acute fulminant cerebral edema: a case series at a large pediatric tertiary center"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:5 [
0 => "D. Hardy"
1 => "C. Patterson Gentile"
2 => "L.A. Beslow"
3 => "M. Santi"
4 => "S. Agarwal"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1055/s-0041-1724099"
"Revista" => array:6 [
"tituloSerie" => "J Ped Neurol"
"fecha" => "2022"
"volumen" => "20"
"numero" => "01"
"paginaInicial" => "052"
"paginaFinal" => "056"
]
]
]
]
]
]
12 => array:3 [
"identificador" => "bib0065"
"etiqueta" => "13"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Clinical approach to the diagnosis of autoimmune encephalitis in the pediatric patient"
"autores" => array:1 [
0 => array:2 [
"etal" => true
"autores" => array:6 [
0 => "T. Cellucci"
1 => "H. Van Mater"
2 => "F. Graus"
3 => "E. Muscal"
4 => "W. Gallentine"
5 => "M.S. Klein-Gitelman"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1212/NXI.0000000000000663"
"Revista" => array:4 [
"tituloSerie" => "Neurol Neuroimmunol Neuroinflamm."
"fecha" => "2020"
"volumen" => "7"
"paginaInicial" => "17"
]
]
]
]
]
]
13 => array:3 [
"identificador" => "bib0070"
"etiqueta" => "14"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Diagnostic yield of brain biopsies in children presenting to neurology"
"autores" => array:1 [
0 => array:2 [
"etal" => false
"autores" => array:3 [
0 => "S. Venkateswaran"
1 => "C. Hawkins"
2 => "E. Wassmer"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1177/0883073807309254"
"Revista" => array:7 [
"tituloSerie" => "J Child Neurol"
"fecha" => "2008"
"volumen" => "23"
"numero" => "3"
"paginaInicial" => "253"
"paginaFinal" => "258"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/18192645"
"web" => "Medline"
]
]
]
]
]
]
]
]
14 => array:3 [
"identificador" => "bib0075"
"etiqueta" => "15"
"referencia" => array:1 [
0 => array:2 [
"contribucion" => array:1 [
0 => array:2 [
"titulo" => "Brain biopsy for neurological diseases of unknown etiology in critically ill patients: feasibility, safety, and diagnostic yield"
"autores" => array:1 [
0 => array:3 [
"colaboracion" => "PSL Brain-Biopsy Study Group"
"etal" => true
"autores" => array:6 [
0 => "B. Mathon"
1 => "M. Favreau"
2 => "V. Degos"
3 => "A. Amelot"
4 => "A. Le Joncour"
5 => "N. Weiss"
]
]
]
]
]
"host" => array:1 [
0 => array:2 [
"doi" => "10.1097/CCM.0000000000005439"
"Revista" => array:7 [
"tituloSerie" => "Crit Care Med."
"fecha" => "2022"
"volumen" => "50"
"numero" => "6"
"paginaInicial" => "e516"
"paginaFinal" => "e525"
"link" => array:1 [
0 => array:2 [
"url" => "https://www.ncbi.nlm.nih.gov/pubmed/34995211"
"web" => "Medline"
]
]
]
]
]
]
]
]
]
]
]
]
]
"idiomaDefecto" => "en"
"url" => "/25298496/unassign/S2529849624000479/v1_202408050416/en/main.assets"
"Apartado" => null
"PDF" => "https://static.elsevier.es/multimedia/25298496/unassign/S2529849624000479/v1_202408050416/en/main.pdf?idApp=UINPBA00004B&text.app=https://revistaneurocirugia.com/"
"EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2529849624000479?idApp=UINPBA00004B"
]