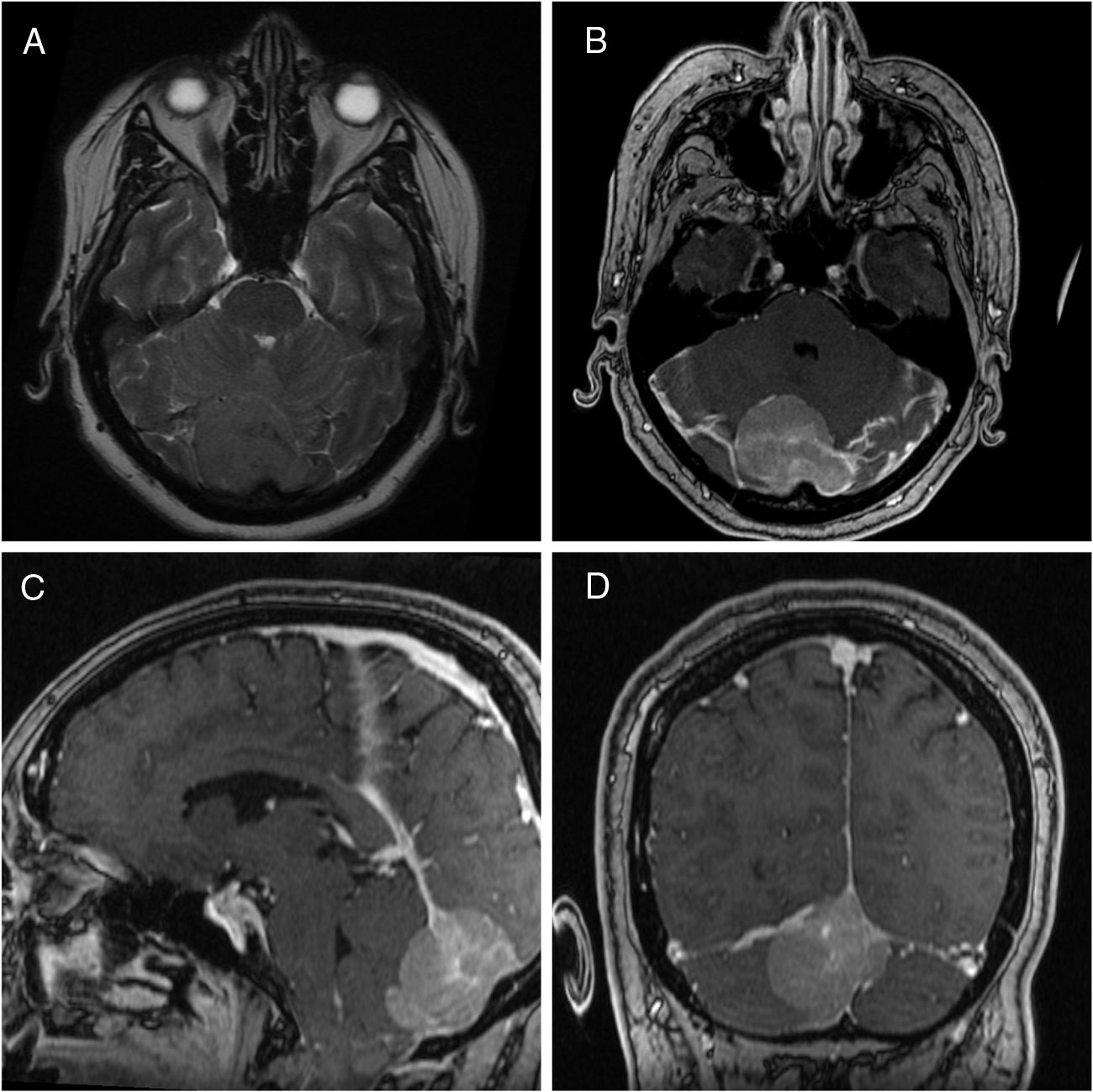
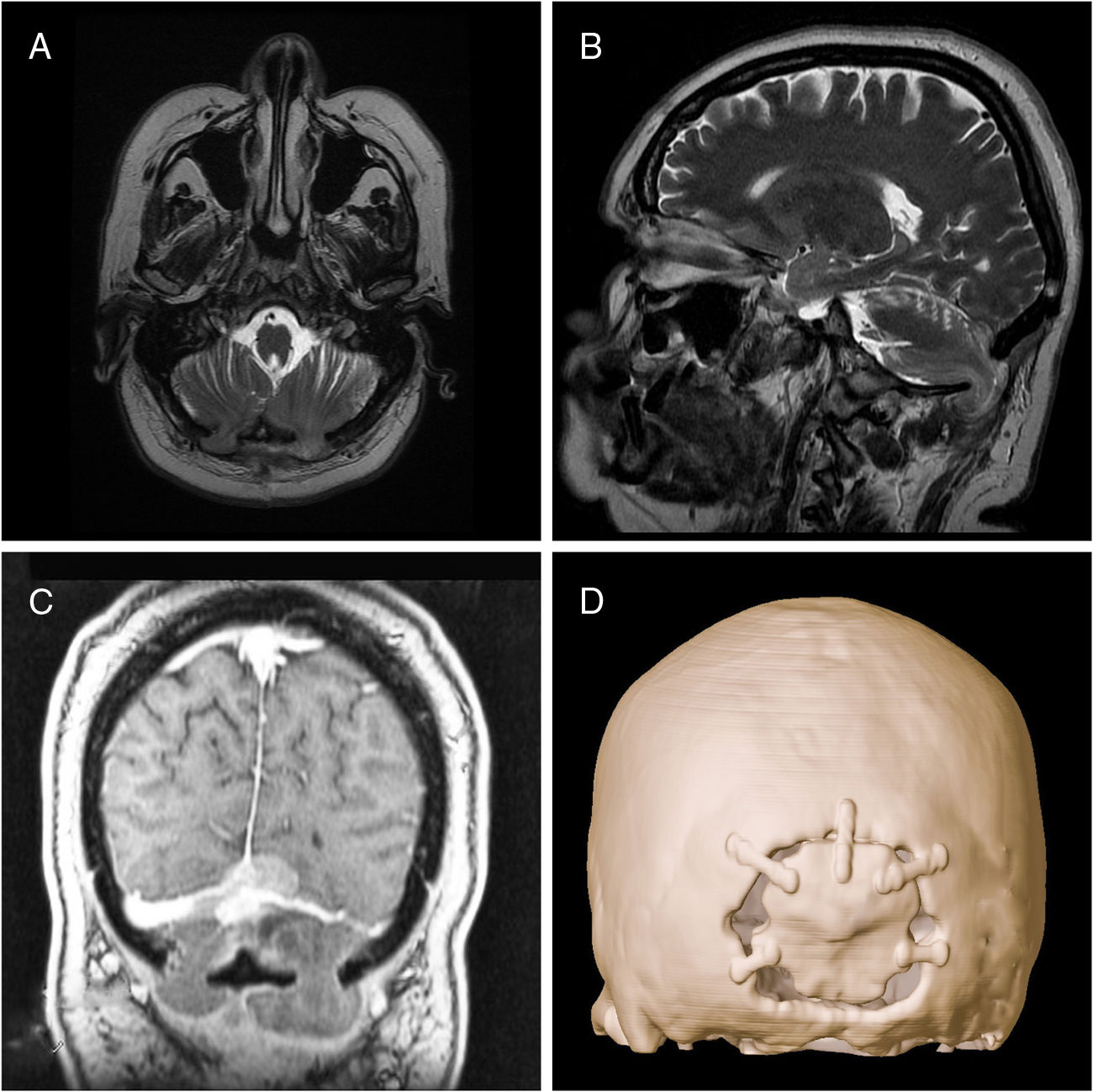
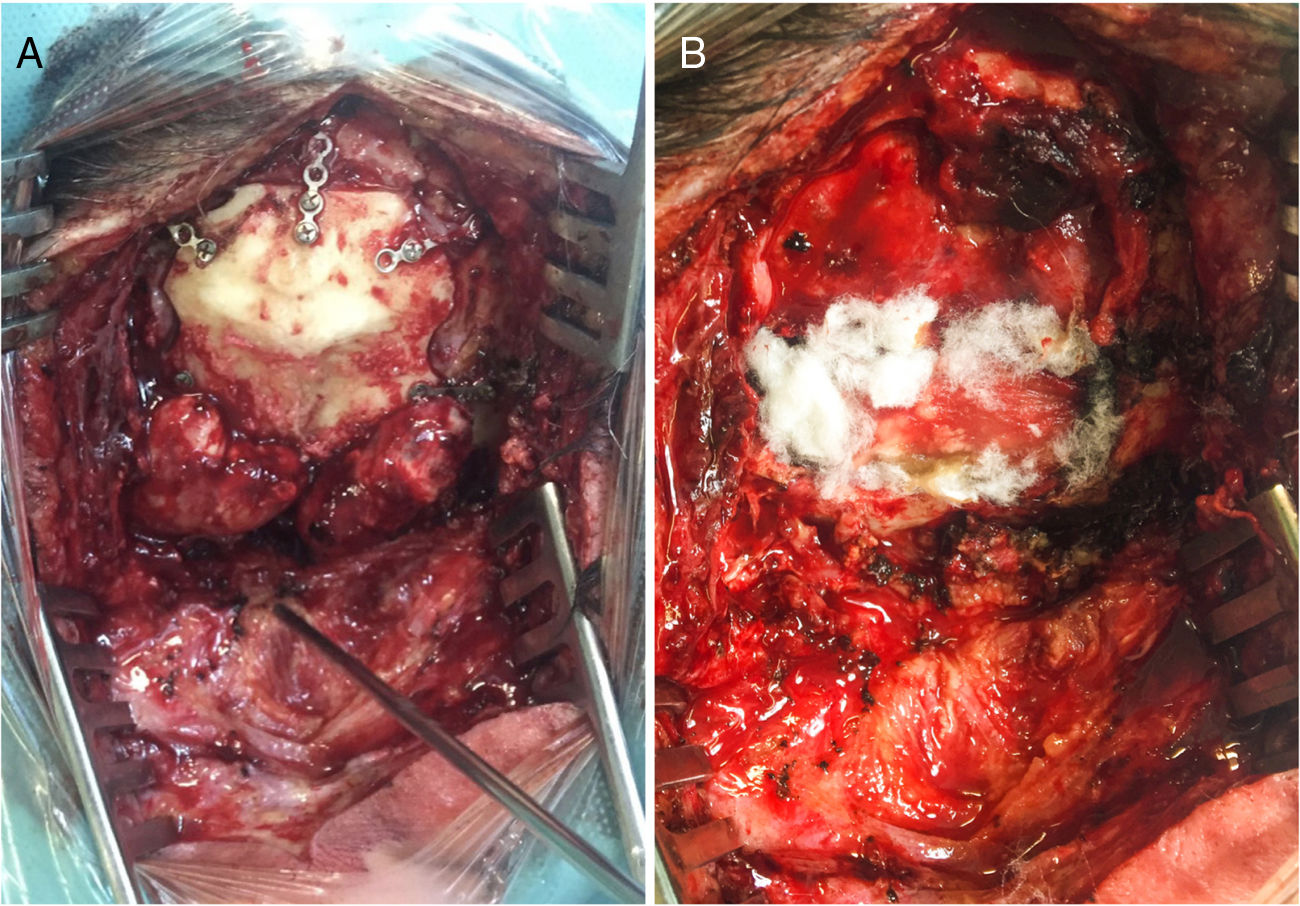
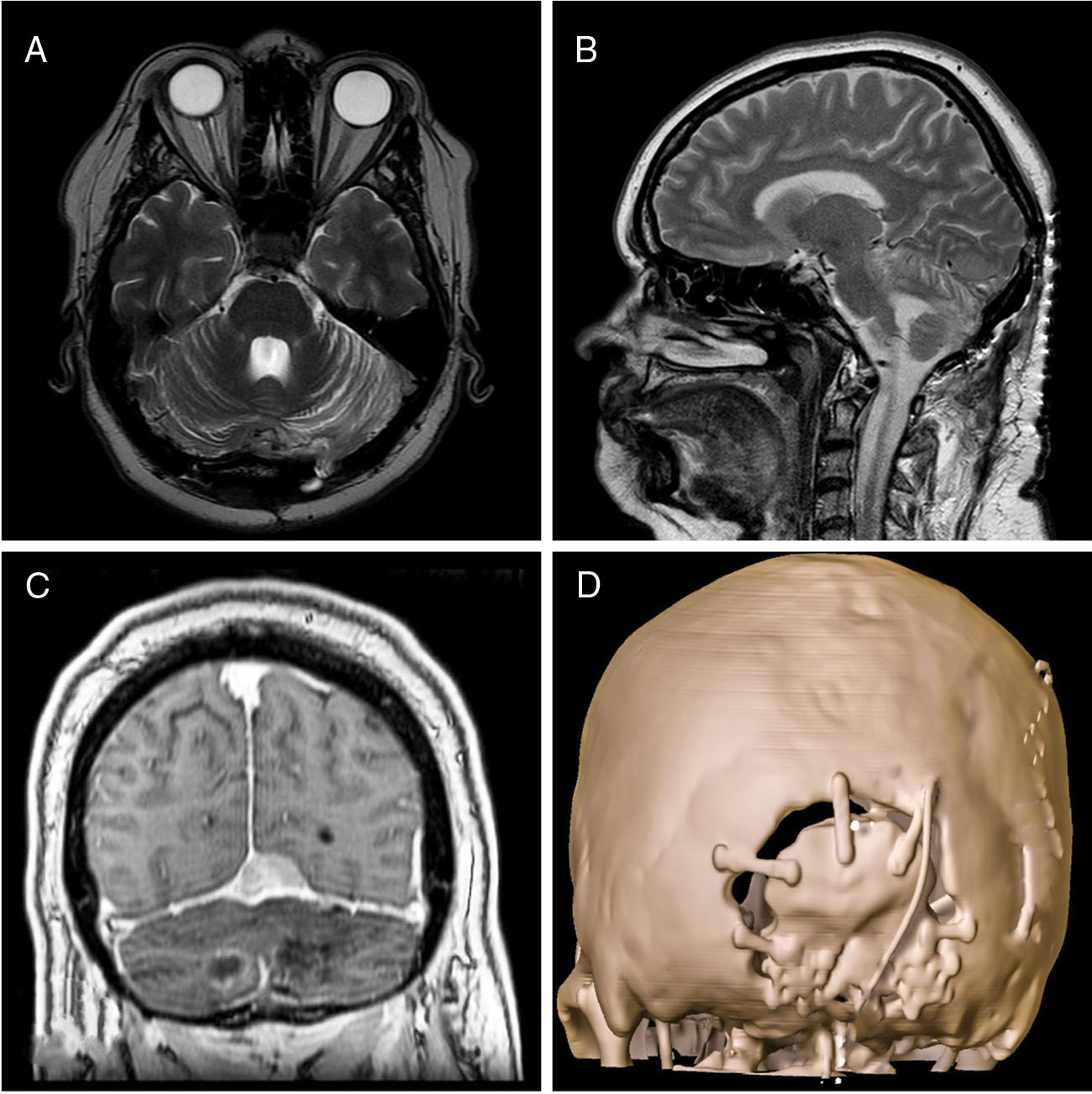
To report a case of post-surgical encephalocele through craniotomy burr holes following the resection of a meningioma of the posterior fossa. A 49-year-old female presented in the emergency room with cephalea. The MRI showed a meningioma of the convexity of the posterior fossa. A resection was performed and the bone flap replaced. The patient recovered uneventfully and was discharged. After 30 days the patient consulted referring cephalea, vomiting and imbalance. Brain MRI revealed a trans-cranial cerebellar herniation through the craniotomy burr holes. An urgent surgery was performed to repair the encephalocele. Post-surgical brain MRI was performed and did not show complications.
Post-surgical encephalocele is an uncommon complication after the resection of a posterior fossa lesion. To avoid this complication, it is recommended thorough dural and bony closure, particularly in the posterior fossa surgeries and in high-risk patients.
Reportamos un caso de un encefalocele posquirúrgico tras la realización de una craneotomía para la resección de un meningioma de fosa posterior. Se trata de una mujer de 49 años que acude al servicio de urgencias por cefalea. Se realizó una resonancia magnética (RM) cerebral que mostró un meningioma de la convexidad en fosa posterior. Se realizó su resección quirúrgica y reposición del colgajo óseo. La paciente se recuperó sin incidencias y fue dada de alta. Treinta días más tarde consultó por cefalea, vómitos e inestabilidad. Se realizó una RM que mostró una herniación cerebelosa a través de los orificios de trépano de la craneotomía, por lo que se llevó a cabo una reparación quirúrgica urgente del encefalocele. Se realizó una RM posquirúrgica, la cual no mostró complicaciones.
El encefalocele posquirúrgico es una complicación poco frecuente tras la resección de un meningioma de fosa posterior. Para evitar esta complicación se recomienda realizar un cierre dural y una reposición ósea cuidadosos, particularmente en las cirugías de fosa posterior y en pacientes con alto riesgo.
Artículo

Si es la primera vez que accede a la web puede obtener sus claves de acceso poniéndose en contacto con Elsevier España en suscripciones@elsevier.com o a través de su teléfono de Atención al Cliente 902 88 87 40 si llama desde territorio español o del +34 932 418 800 (de 9 a 18h., GMT + 1) si lo hace desde el extranjero.
Si ya tiene sus datos de acceso, clique aquí.
Si olvidó su clave de acceso puede recuperarla clicando aquí y seleccionando la opción "He olvidado mi contraseña".