P-168 - INTRACRANEAL TUBERCULOMA DISGUISED AS MALIGNANT CNS TUMOR
Hospital Universitario Marqués de Valdecilla, Santander, Spain.
Introduction: Though relatively common in developing countries, it is reasonably unusual to encounter cerebral tuberculosis in our medium nowadays, making its diagnosis a challenging task as the inflammatory-granulomatous process that mycobacteria undergo may mimic a malignant CNS lesion in radiological studies.
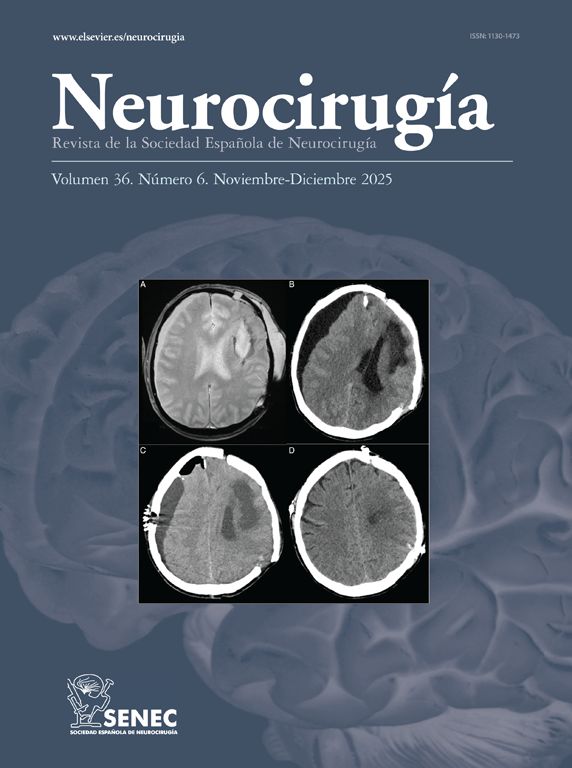
Case report: 25 yo patient originally from Gambia presents with ongoing history of GI problems including chronic gastritis, duodenitis, Chron’s disease follow-up, as well as with consistent vomiting, 30 kg weight loss in 2 years and persistent headache. A CT scan is initially performed showing a vermian space occupying lesion (SOL) with surrounding oedema that causes compression of the ventricular system with radiological signs of incipient hydrocephalus and trans-tentorial herniation. As a first measure, a ventriculo-peritoneal shunt is placed which instantly improved the patients symptomatology. All initial serological studies including bone marrow biopsy and cerebro-spinal fluid were negative for a broad spectrum of infectious agents. A biopsy of the CNS SOL was therefore performed via a modified supracerebellar-infratentorial lateral approach, which eventually reported positivity for Mycobacterium tuberculosis complex. The patient tolerated the surgical procedure correctly and tuberculostatic treatment was immediately started. With subsequent appropriate peri-operative evolution and treatment tolerance, he was discharged from the hospital without remarkable complications, currently being periodically followed-up in out-patient clinic with subsequent MRI showing significant lesion size reduction.
Discussion: In atypical scenarios in which infectious etiology may be suspected, the physician must always keep a fierce suspicion for unconventional diagnoses, even more so bearing in mind the increased migration from developing countries where the prevalence of infectious diseases is much greater. The treatment for intracranial TBC remains being tuberculostatic agents. In cases like such, all initial serological testing may be negative, leaving room only for an invasive diagnosis which must be carried out promptly to avoid worsening and extension of the lesions initially encountered.